This article describes a Hoffa fracture with a sagittal split, a rare subtype successfully treated with a buttress plate to address the sagittal plane fracture component.
Dr. Benjamin Schapira, West Hertfordshire Hospitals NHS Trust, United Kingdom. E-mail: ben.schapira@hotmail.com
Introduction: A Hoffa fracture is a rare coronal plane, intra-articular fracture of the femoral condyle involving the weight-bearing portion of the posterior distal femur. The anatomy of this fracture lends it to be an inherently unstable injury, requiring surgical fixation to achieve stability. To date, research describing Hoffa fractures is limited to small case series and case reports. This article aims to describe the first case discussion of a unique type of Hoffa fracture with a sagittal split within the fragment and intra-articular comminution. We review the etiology, management, and follow-up of this case with respect to the existing literature.
Case Presentation: A 40-year-old man involved in a high-speed motorcycle collision presented with a displaced coronal plane, intra-articular fracture of the lateral femoral condyle (Hoffa fracture). Cross-sectional imaging with MRI identified a sagittal split in the Hoffa fragment and partial anterior cruciate ligament rupture. This was managed with open reduction and internal fixation (ORIF) through a lateral parapatellar approach with cannulated compression screws and a distal radius plate used in buttress mode. Postoperatively, the patient was rehabilitated with graduated increase in range of knee movement range of motion (ROM) and weight-bearing. Five months after surgery, he had regained independent motion of the knee but suffered residual stiffness, which required arthroscopic adhesiolysis. At 6-month follow-up, the patient was pain free and had resumed normal activities with knee ROM 5–90°.
Conclusion: This article highlights a unique and rare subtype of Hoffa fracture not illustrated in current classifications. Management is notoriously challenging with little consensus as to the optimal approach, implants, and post-operative rehabilitation. ORIF provides the best choice for maximal post-operative knee function. In our case, a buttress plate was utilized to stabilize the sagittal fracture component. Post-operative rehabilitation may be complicated by soft-tissue and/or ligamentous injury. Choice of approach, technique, implant, and rehabilitation are dependent on fracture morphology. Close follow-up is required with strict physiotherapy to ensure sufficient long-term range of movement, patient satisfaction, and return to activity.
Keywords: Hoffa fracture, intracondylar, coronal, femoral condyle, sagittal split.
The Hoffa fracture has classically been described as a coronal plane, intra-articular fracture of the femoral condyle involving the weight-bearing parts of the posterior distal femur [1]. The rarity of this fracture is exemplified in its incidence, accounting for up to only 13% of distal femoral fractures [2]. Due to its instability, failure to achieve rigid fixation often results in malalignment, osteonecrosis, and post-traumatic osteoarthritis [3]. The injury mechanism remains debated in literature but is hypothesized to involve an axial ground force transmitted through the tibial plateau in a knee flexed at 90° [4]. This article aims to describe the first case discussion of a unique type of Hoffa fracture with a sagittal split within the fragment and intra-articular comminution. We review the etiology, management, and follow-up of this case with respect to the existing literature.
A 40-year-old male motorcyclist was involved in a high-speed road traffic collision. He was hit by a car and fell onto a flexed right knee. He was unable to bear weight and presented to the emergency department the following day where he was immobilized in an above knee backslab. Radiographs of the right knee confirmed a displaced unicondylar fracture of the lateral femoral condyle (Fig. 1). Computed tomography (CT) demonstrated a sagittal split in the Hoffa fragment and intra-articular comminution (Fig. 2). A subsequent MRI scan showed partial rupture of the anterior cruciate ligament (ACL).
Surgery:
Surgical technique (Procedure one)
The patient was placed in a supine position under general anesthesia. An anterior midline skin incision over the knee was made followed by a lateral parapatellar approach. The fracture was exposed where a small amount of comminution was visible (Fig. 3).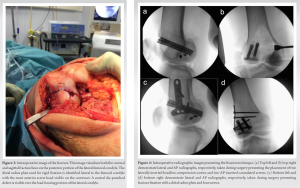
A central die-punch defect at the site of fracture line convergence was noted and deemed to be non-reconstructable. The fracture was reduced and held with a bone reduction clamp. Two K-wires were used to secure the fragments. Two headless compression screws were inserted from lateral to medial through the base of the lateral femoral condyle. A further two guidewires were passed from the anterior aspect of the femur to the main fracture fragment to allow two 7.5 mm × 60 mm cannulated screws to be inserted. A distal radius plate was used as a buttress plate over the lateral aspect of the femoral condyle and secured with screws (Fig. 4). Intraoperative fluoroscopy confirmed anatomical reduction. Postoperatively, the patient was instructed to remain strictly non-weight-bearing for 6 weeks in a hinged knee brace (0–60°). Range of movement was planned to increase by 20° every 2 weeks.

Procedure one follow-up
By 3 weeks after surgery, the patient reported no problems. Post-operative pain and swelling had settled, his range of motion (ROM) was increased to 0–90°, but he was advised to continue his non-weight-bearing status. Eight weeks postoperatively, the patient described a reduced range of active movement (0–45°), this was due to compliance difficulties with physiotherapy. As a natural consequence of not bearing weight and wearing a knee brace, he demonstrated quadriceps and gastrocnemius muscle wasting. At this point, the patient was encouraged to begin full weight-bearing through the knee, to discard the brace, and continue physiotherapy to regain muscle strength. At the 5-month consultation, examination revealed independent motion of the right knee. The patient was able to fully bear weight through the knee but walked with a limp due to knee stiffness. His ROM had plateaued at a range of 5–45°. Despite this, functionally, the patient was back to normal duties. Radiographically (Fig. 5), there was evidence of heterotrophic ossification around the lateral femoral condyle. Apart from this, the metal work was in situ and the fracture was healing in a satisfactory position. The patient was therefore offered a manipulation under anesthesia and arthroscopy to assess the status of articular cartilage in his knee.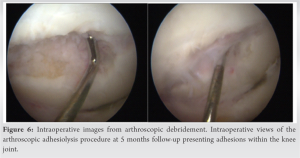
Arthroscopy and adhesiolysis (Procedure two)
During arthroscopy, the medial meniscus was found to be intact and the die-punch defect still visible. Significant adhesions were seen (Fig. 6), and therefore, adhesiolysis and microfracture treatment to the affected cartilage area were carried out. The patient was advised not to bear weight through the knee for 4 weeks but to commence full ROM with physiotherapy immediately. At the 6-month consultation after his original surgery, and 3 weeks post-adhesiolysis, the patient demonstrated pain-free range of movement of 5° flexion to 90° flexion. He was discharged from both orthopedic and physiotherapy care at just under 1-year post-surgery when he was pain free and undertaking his usual activities. He had a mild fixed flexion deformity of 10° but was content with his knee and overall treatment.
Injury description
Hoffa fractures are rare, coronal plane, intra-articular fractures of the femoral condyle described primarily in small case reports and series. First described by Friedrich Busch in 1869 and again by Albert Hoffa in 1904, these fractures are most commonly reported in the lateral condyle, as was seen in our case; but are also found in the medial condyle and even less frequently bicondylar [5]. The fracture occurs when a flexed knee contacts the ground, transmitting an axial force from the proximal femur and distal tibia through the posterior articular surface of the femur [4], concentrating a shear force over the posterior femoral condyle, and instigating the coronal split [3]. Furthermore, both the physiological valgus orientation of the knee and larger anteroposterior (AP) dimension of the lateral condyle lead to earlier impaction against the tibial plateau, explaining the lateral fracture predominance [6]. This position is analogous to that held while riding a motorcycle (knees flexed to 90° and hips abducted), thus explaining the higher prevalence among this population. However, to date, no biophysical study has confirmed this mechanism and so the exact cause remains unknown.
Classification
Multiple classification systems exist to describe Hoffa fractures. The most popular, AO/OTA system, describes the 33B3 subtype of coronal plane distal femoral fractures with further division into anterior flake (33B3.1), unicondylar (33B3.2), and bicondylar (33B3.3) fractures [7]. The most recent classification systems describe subtypes of Hoffa fracture, inclusive of supracondylar, posterior diaphyseal, and comminuted fracture patterns but still fail to categorize our subtype of fracture [8]. It was not until 2017 that Xie et al. recognized the sagittal split and described its occurrence most commonly in the middle third area, as seen with our case [9]. They reviewed a classification pertaining to number of fracture lines and fragments, rather than distinct subtypes [10]. This classification may better represent our case as to date, no formal classification has identified our fracture pattern.
Imaging
The standard approach to imaging Hoffa fractures includes AP and lateral radiographs, with MRI indicated when ligamentous or cartilaginous injuries are of concern. However, there is often difficulty in identifying minimally displaced fractures with these views. As in our case, CT can be used for greater accuracy in demonstrating cross-sectional fracture morphology, given the commonly preceding high-energy trauma.
Management
The Hoffa fracture is inherently unstable, incurring high shear stresses along both coronal and sagittal fracture lines with any movement, bearing weight or axial compression [4]. Treatment has historically proved challenging, aiming for anatomical reduction, rigid fixation, and maximal function. Open reduction and internal fixation is the preferred and most commonly reported management strategy with excellent reports of post-operative recovery, range of movement, and clinical scores [6]. In contrast, non-surgical management is briefly described with complaints of early displacement, osteonecrosis, knee stiffness, and post-traumatic osteoarthritis, with subsequent need for delayed surgical fixation [11].
Surgical approach
There is much debate over the optimal approach to surgical management with enormous variance in surgical approach, screw type, length, direction, and choice of implants for fixation [6]. In our case, we employed a lateral parapatellar approach. This approach is familiar to most orthopedic surgeons performing total knee arthroplasty and does not compromise future joint replacement. Other reports describe direct lateral, posteromedial/lateral, and Swashbuckler approach, each emphasizing their merits [6].
Screw direction
There is also little agreement in choice of screw direction. Most studies promote either PA or AP insertion perpendicular to the fracture line. In our case, we inserted screws through an AP direction to reduce the risk of shattering the condylar fragment, reduced soft-tissue/neurovascular/articular damage [10], and reduced the risk of screw back-out and intra-articular penetration [12].
Implant choice
Screw size and plating options too vary among all published surgical cases. There is limited research available regarding screw size and stability. Studies report greater rigidity and load to failure with longer length screws with evidence proving one 6.5 mm screw to provide the same stability of two 3.5 mm screws [13]. Studies describe an ever-increasing array of plating options. We chose a lateral buttress plate with cannulated compression screws to prevent superior displacement of the lateral fragment in the sagittal fracture, while the cannulated screws achieved intra-articular compression and prevented displacement of the coronal plane fracture. We also used multiple headless compression screws to address the intra-articular comminution with as little articular damage as possible.
The vast array of surgical exposure, screw, and implant choice in Hoffa management proves that there is little consensus among surgeons. One must, therefore, consider the circumstances of each individual injury, associated injuries, and the surgeons’ own experience/comfort in choosing the optimal approach on a one-to-one basis.
Post-operative regimen and outcome
There is much debate over the optimal post-operative rehabilitation process. Early mobilization risks delayed or failed union and periprosthetic fracture but avoid stiffness, poor joint function, and subsequent osteoarthritis [14]. We opted for graduated increase in ROM followed by weight-bearing, a regimen reported widely in Hoffa management. Our patient experienced suboptimal ROM recovery complicated by adhesion formation, potentially related with the partial ACL rupture. Ultimately studies report the type of rehabilitation post-surgery to hold no significant bearing on final ROM (early vs. delayed mobilization) but advocate a slower rate of graduated return, more frequent follow-up, and prompt investigation of new pain or swelling [15].
Hoffa fractures are rare and difficult to treat. Diagnosis requires a high index of suspicion and surgical treatment is the best choice for maximal post-operative knee function. There is no consensus on management. Choices for surgical approach, technique, implants, and post-operative rehabilitation are dependent on the fracture configuration and surgeons’ preference. In this particular case, we described a Hoffa fracture with a sagittal split, a rare subtype not adequately illustrated by current classifications and emphasizes the importance of using a buttress plate to address the sagittal plane fracture component. Despite the need for a secondary procedure, the treatment has had positive early outcomes and may guide future management for similar fracture morphology.
This article features the first case description of a rare subtype of Hoffa fracture featuring a sagittal split within the Hoffa fragment. With this case, we hope to shed light on a rare and unique fracture morphology not illustrated in current classification systems. Our case describes an in-depth account of surgical intervention, post-operative rehabilitation, and follow-up, reviewed in the context of other reports of Hoffa fractures. We believe this case highlights the optimal approach to surgical fixation with realistic goals of rehabilitation and recovery of function.
References
- 1.Bartonicek J, Rammelt S. History of femoral head fracture and coronal fracture of the femoral condyles. Int Ortho 2015;39:1245-50. [Google Scholar]
- 2.Xiao K, Chen C, Yang J, Yang D, Liu J. An attempt to treat Hoffa fractures under arthroscopy: A case report. Chin J Traumatol 2018;21:308-10. [Google Scholar]
- 3.Mierzwa A, Toy K, Tranovich M, Ebraheim N. Surgical approaches, postoperative care, and outcomes associated with intra-articular Hoffa fractures: A comprehensive review. JBJS Rev 2019;7:e8. [Google Scholar]
- 4.Wagih AM. Arthroscopic management of a posterior femoral condyle (Hoffa) fracture: Surgical technique. Arthrosc Tech 2015;4:e299-303. [Google Scholar]
- 5.Arastu MH, Kokke MC, Duffy PJ, Korley RE, Buckley RE. Coronal plane partial articular fractures of the distal femoral condyle. Bone Joint J 2013;95-B:1165-71. [Google Scholar]
- 6.Bali K, Mootha AK, Krishnan V, Kumar V, Rawall S, Goni V. A rare case of bicondylar Hoffa fracture associated with ipsilateral tibial spine avulsion and extensor mechanism disruption. Chin J Traumatol 2011;14:253-6. [Google Scholar]
- 7.Kellam JF, Meinberg EG, Agel J, Karam MD, Roberts CS. Fracture and dislocation classification compendium-2018. J Orthop Trauma 2018;32:S1-170. [Google Scholar]
- 8.Bagaria V, Sharma G, Waghchoure C, Chandak R, Nemade A, Tadepelli K, et al. A proposed radiological classification system of Hoffa’s fracture based on fracture configuration and consequent optimal treatment strategy along with the review of literature. SICOT J 2019;5:18. [Google Scholar]
- 9.Xie X, Zhan Y, Dong M, He Q, Lucas JF, Zhang Y, et al. Two and three-dimensional CT mapping of Hoffa fractures. J Bone Joint Surg 2017;99:1866-74. [Google Scholar]
- 10.Zhou Y, Pan Y, Wang Q, Hou Z, Chen W. Hoffa fracture of the femoral condyle injury mechanism, classification, diagnosis and treatment. Medicine (Baltimore) 2019;98:e14633. [Google Scholar]
- 11.Somford MP, Van Ooij B, Schafroth MU, Kloen P. Hoffa nonunion, two cases treated with headless compression screws. J Knee Surg 2013;26:589-93. [Google Scholar]
- 12.Borse V, Hahnel J, Cohen A. Hoffa fracture: Fixation using headless compression screws. Eur J Trauma Emerg Surg 2010;36:477-9. [Google Scholar]
- 13.Hak DJ, Nguyen J, Curtiss S, Hazelwood S. Coronal fractures of the distal femoral condyle: A biomechanical evaluation of four internal fixation constructs. Injury 2005;36:1103-6. [Google Scholar]
- 14.Jain SK, Jadaan M, Rahall E. Hoffa’s fracture lateral meniscus obstructing the fracture reduction a case report. Injury 2015;46:419-21. [Google Scholar]
- 15.Lohiya R, Jindal N, Bachhal V, Garg S, Bhowmik S. Hoffa fracture: Analysis of factors affecting the final outcome after treatment with partially threaded screws. Int J Res Orthop 2017;3:814-8. [Google Scholar]









