Intraosseous lipoma is an underrecognized, underdiagnosed benign bone tumor that should be included in a differential diagnosis of dull, chronic bone pain as prompt surgical treatment provides symptom resolution and return to function.
Dr. MaKenzie M Chambers, Cooper Medical School of Rowan University, 401 Broadway, Camden, New Jersey. E-mail: chambe42@rowan.edu
Introduction: Intraosseous lipomas are benign tumors composed of mature fat that reside within the intramedullary canal. Although many cases are asymptomatic, some patients report pain that interferes with daily living. For patients presenting with refractory pain, surgical excision may be performed. These tumors were once thought to be rare, but a recent increase in awareness and diagnostic capability may contradict this.
Case Presentations: A 27-year-old female presented with a 3-month history of deep and aching pain in her left shoulder. The second patient was a 24-year-old female who presented with a 3-year history of pain in her right tibia. The third was a 50 year old female who presented with a 4-month history of deep pain in her right humerus. The fourth patient was a 34-year-old female who presented with a 6-month history of the left heel pain. All were found to have intraosseous lipomas and were treated with excisional curettage, achieving resolution of symptoms.
Conclusion: These cases may help orthopedists better understand the presentation and treatment of intraosseous lipomas due to several shared characteristics. We also hope that this report may lead clinicians to include this pathology in their differential diagnosis when patients present with similar symptoms. As the prevalence of these tumors appears to be increasing, efficient diagnosis and treatment will become increasingly valuable to orthopedists and patients.
Keywords: Intraosseous lipoma, orthopedic oncology, bone tumor, curettage.
Intraosseous lipomas are rare and benign bone tumors that are derived from mature adipocytes existing within the intramedullary canal. They account for <0.1% of primary bone neoplasms and usually manifest in long bones [1, 2, 3]. They are thought to be idiopathic, with unexplained etiology and unknown pathogenesis. Diagnosis of an intraosseous lipoma must combine radiographic imaging findings with histopathologic features consisting of varying degrees of viable lipocytes, calcification, marrow necrosis, and bony trabeculae [4]. Symptoms include vague, throbbing bone pain that may or may not radiate or be related to activity. Recent advanced imaging techniques may explain the increased incidence of reported intraosseous lipomas, revealing that these tumors may not be as rare as once thought [5, 6]. Treatment for an intraosseous lipoma is usually conservative, as these lesions are often asymptomatic and do not carry a malignant degeneration risk [7]. Operative treatment is indicated for refractory pain or if the lesion is large enough to risk pathologic fracture [2] and involves corticotomy with excisional curettage of the lipomatous tumor. Prophylactic fixation may also be included in treatment [5]. There are few reports in the literature that thoroughly describe this entity, its presentation and natural history, treatment strategies, and outcomes after treatment [1, 2, 3, 4, 8] (Table 1). Due to this paucity in the literature, we aim to describe four cases of intraosseous lipomas that required surgical intervention to alleviate pain and prevent impending pathologic fracture.
Case Presentation: #1
A 27-year-old female complained of a 3-month history of throbbing activity-related pain in her left anterior shoulder. The left humerus radiographs revealed a lytic bone lesion within the diaphysis with loss of trabecular markings (Fig. 1a, 1b). Magnetic resonance imaging (MRI) revealed fatty replacement of the normal marrow, with areas of cyst-like fluid signal and inconsistent contrast-enhancement (Fig. 2a, 2b). Due to these discrete areas of cystic change, open biopsy was performed. Pathology revealed adipose tissue and normal marrow elements, confirming the diagnosis of intraosseous lipoma.
Intralesional excision was performed through the anterolateral approach to the left humerus. A 10 mm diameter trephine reamer was used to create a round cortical window in the anterolateral cortex to gain access to the intramedullary canal. Curved curettes were utilized to excise the tumor and a flexible suction tip was inserted to achieve thorough excision of its proximal- and distal-most extents. The tumor cavity was packed with cancellous allograft bone chips and the cortical window was replaced. The patient’s arm was placed in a sling and range of motion/weight bearing was progressed as cortical healing and incorporation of the graft was demonstrated on x-ray. She had returned to full function without pain by her 6-month post-operative appointment.
Case Presentation: #2
A 24-year-old female patient complained of 3 years of aching and constant pain in the right proximal tibial metaphysis that was aggravated by activity. She reported a history of motor vehicle accident 2 years before, when she sustained a non-displaced right tibial plateau fracture treated nonoperatively. In the months before presentation to our clinic, she was diagnosed at an outside facility with tibial stress fracture as the cause of her pain and underwent anterior tibial cortical drilling without relief of symptoms. Radiographs were unremarkable, but MRI demonstrated subtle loss of trabecular markings within the tibial marrow space, replaced by homogeneous fat signal (Fig. 3a, 3b). There was also bone edema around the site of drilling, concerning for stress fracture. An open biopsy was performed and pathologic examination revealed marrow elements with mature adipose tissue, confirming the diagnosis of intraosseous lipoma. Excision of the intramedullary tumor was initiated through a longitudinal incision over the medial tibial metaphysis. A 3 cm oval cortical window was created and the lipomatous tissue was excised using curettes. There was considerable sclerotic bone found at the site of chronic stress reaction, concerning for incomplete healing, indicating prophylactic fixation. The surgeon then proceeded with uneventful prophylactic intramedullary nailing of the tibia through a medial parapatellar approach. The reamers served to secondarily excise the tumor. Finally, the cortical window was packed with allograft. Postoperatively, the patient was weightbearing as tolerated and reported complete resolution of symptoms a month later.
Case Presentation: #3
A 50-year-old female presented with a 4-month history of a constant and deep aching pain in her right proximal humerus that was aggravated by weather changes and sleeping on the affected side. Radiographs were unremarkable, but MRI revealed fatty replacement of the normal trabecular bone for nearly the length of the humerus.
Tumor excision was performed through an anterolateral approach to the humerus. A 10 cm incision centered over the junction of the proximal and middle thirds of the diaphysis was made, dissection was carried down to the anterolateral cortex of the humeral shaft, and a burr was used to create a 4 cm oval cortical window. Curettes and flexible suction tips were used to excise the tumor from the humeral head down to the epicondyles. After thorough excision, the canal was packed with allograft cancellous bone chips. Due to the length of the cortical window acting as a stress riser, the humerus was prophylactically stabilized using a carbon fiber plate (Fig. 4a, 4b). The patient’s arm was placed in a sling and she initiated immediate physical therapy. She had regained full range of motion and strength 3 months from surgery. Histopathologic examination revealed mature adipose tissue and bone marrow elements, compatible with intraosseous lipoma.
Case Presentation: #4
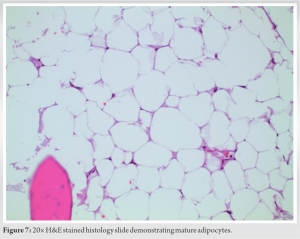
A 34-year-old female patient presented with a 6-month history of activity-related left heel pain. On initial assessment of a left foot CT scan, the lesion was thought to be a large fluid-filled cyst within the calcaneus. However, MRI revealed that the lytic bone lesion was composed of fat, as opposed to fluid (Fig. 5a, 5 b). No pathologic fracture was present, but there was slight remodeling of the adjacent cortical bone at Boehler’s angle and thinning of the cortex in some areas. The tumor filled the marrow space completely in the coronal plane. Excision of the intramedullary tumor was performed through a laterally-based incision over the hindfoot, using the longitudinal limb of the classic L-shaped extensile approach to the lateral calcaneus. The “no-touch technique” was employed. An ultrasonic bone scalpel (Sonopet Ultrasonic Aspirator, Stryker, Kalamazoo, MI) was used to create a 3 × 1 cm cortical window in the lateral calcaneus to access the marrow space. The tumor was excised using a pituitary, curettes, and suction. Once complete excision of the mass was confirmed, the tumor cavity was packed with allograft cancellous chips, and the excised cortical window fragment was replaced into the cortical defect. Postoperatively, the patient was placed in a CAM boot and was non-weight bearing on the lower left extremity for 7 weeks. At her most recent follow-up appointment, 9 weeks from surgery, X-rays revealed excellent incorporation of the bone graft and cortical fragment, and she had returned to normal function with residual mild soreness after extended periods of weight bearing (Fig. 6a, 6b). Final pathologic examination revealed mature adipose tissue, compatible with the diagnosis of intraosseous lipoma (Fig. 7).
Intraosseous lipomas are unique intramedullary lesions that can pose challenges in identification, diagnosis, and treatment. Due to their limited occurrence, non-specific symptom presentation, and subtle changes on radiographs, many intraosseous lipomas may be misdiagnosed or overlooked resulting in delayed treatment [2]. However, with advancing imaging techniques and improved physician understanding [1], we are able to highlight four cases of confirmed intraosseous lipomas treated at our institution. Vague, deep and throbbing pain are the most common symptoms that the patient will note. The presence of an intraosseous lipoma can lead to increased intraosseous pressure, which likely explains this sensation. Radiographic diagnosis remains difficult, as the majority of patients have X-rays that appear normal, yet some images do show subtle changes such as loss of trabecular markings. MRI can also show loss of bony trabeculae and replacement with homogenous fat signal, but this can be difficult to detect. Due to the subtle changes in imaging, physicians should have a high index of suspicion for an intraosseous lipoma when a patient presents with characteristic symptoms and other pain-generating phenomena such as trauma, rotator cuff pathology, radiculopathy, and degenerative joint disease have been ruled out. In general, the authors recommend having a low threshold for obtaining an MRI of a long bone that is painful for several weeks in the setting of normal X-ray findings, as marrow-replacing lesions may be undetectable on plain radiographs but obvious on MRI. Treatment in all four cases involved intralesional excision of the mass through a cortical window utilizing curettes and flexible suction tips. As it was determined necessary by the surgeon in two of our four cases, prophylactic fixation can also be performed. Risks of pathologic fracture secondary to the cortical thinning from the tumor itself, or secondary to the cortical window created iatrogenically, are indications for prophylactic fixation and should be considered on a case-specific basis. Postoperatively, all patients experienced resolution of their symptoms and demonstrated a return to full range of motion and radiographs consistent with healing. We hypothesize that excision of the tumor allows the intraosseous pressure to normalize, facilitating these patients’ symptomatic improvement. To date, no patient has experienced local recurrence or pathologic fracture, suggesting that intralesional excision is appropriate and successful when a patient meets surgical indications. Although there is limited literature detailing the pathogenesis, progression, and resolution of intraosseous lipomas (Table 1), it is important to note that our findings and approach to treatment are consistent with the current understanding of these lesions [1, 2, 3, 4]. Frangez et al. described a similar case of a calcaneal intraosseous lipoma that required surgical intervention and yielded post-operative improvements in symptoms and full rehabilitation time consistent with our fourth patient. Our cases all demonstrated similar histopathologic changes, specifically the presence of mature adipose tissue, which is also consistent with the current literature [8, 9, 10]. The authors hope that contribution of these four cases to the sparse available literature that exists will allow for increased awareness and understanding of these tumors.
Once thought to be extremely rare bone lesions, the incidence of intraosseous lipomas has increased due to the widespread nature of advanced imaging and more clinicians including this condition on their differential diagnoses. Proper diagnostic workup should be initiated for patients who present with symptoms of throbbing bone pain with subtle radiographic changes to evaluate for this diagnosis once other likely pathologies have been ruled out. If conservative treatment fails, intralesional excision with or without prophylactic fixation provides pain relief and return to function.
Intraosseous lipomas can cause vague and persistent bone pain and may be difficult to diagnose on physical examination and imaging studies. Pain control is achieved through excision of the tumor, occasionally paired with prophylactic fixation as indicated.
References
- 1.Dammerer D, Neugebauer J, Putzer D, Henninger B. Multiple intraosseous lipomatosis a case report and a review of the literature. In Vivo 2021;35:959-64. [Google Scholar]
- 2.Frangez I, Nizic-Kos T, Cimerman M. Threatening fracture of intraosseous lipoma treated by internal fixation. J Am Podiatr Med Assoc 2019;109:75-9. [Google Scholar]
- 3.Narang S, Gangopadhyay M. Calcaneal intraosseous lipoma: A case report and review of the literature. J Foot Ankle Surg 2011;50:216-20. [Google Scholar]
- 4.Sivrikoz MC, Döner E, Durceylan E. Intraosseous lipoma of the rib. Turk Gogus Kalp Damar Cerrahisi Derg 2019;27:590-2. [Google Scholar]
- 5.Hart JA. Intraosseous lipoma. J Bone Joint Surg Br 1973;55:624-32. [Google Scholar]
- 6.Coquerelle P, Cotten A, Flipo RM, Chastanet P, Duquesnoy B, Delcambre B. Intraosseous lipoma: Role and limitations of modern imaging techniques. Rev Rhum Engl Ed 1995;62:147-50. [Google Scholar]
- 7.Milgram JW. Intraosseous lipomas. A clinicopathologic study of 66 cases. Clin Orthop Relat Res 1988;231:277-302. [Google Scholar]
- 8.Bertram C, Popken F, Rütt J. Intraosseous lipoma of the calcaneus. Langenbecks Arch Surg 2001;386:313-7. [Google Scholar]
- 9.Eduardo E, Wang L, Garcia MK, Kumar R, Ayala A, Zoran G. Intraosseous lipoma. A clinical, radiologic, and pathologic study of 5 cases. Ann Diagn Pathol 2007;11:320-5. [Google Scholar]
- 10.Kang HS, Kim T, Oh S, Park S, Chung SH. Intraosseous lipoma: 18 years of experience at a single institution. Clin Orthop Surg 2018;10:234-9. [Google Scholar]