High degree of suspicion should be kept in mind in diagnosing shoulder TB and any sinus or swelling (scapular region or elsewhere around shoulder) should be suspected and evaluated for tuberculosis, especially in endemic areas like India.
Dr. Nikhil Tandon, Department of Orthopaedics, Seth VC Gandhi and MA Vora Municipal General Hospital, (Rajawadi Hospital), Ghatkopar East, Mumbai - 400 077, Maharashtra, India. E-mail: nikhil.tandon.nt@gmail.com
Introduction: Tuberculosis (TB) of shoulder joint is uncommon. It has an incidence rate of 0.9–1.7%. We report a case of 50 year old man presenting with cold abscess over scapula bone, secondary to the shoulder joint involvement (with sinus tracking to the anterior aspect of shoulder joint).
Case Report: A 50-year-old male presented to our hospital with complaints of swelling over right scapular area since 2 months. The patient had similar swelling on the anterior aspect of right shoulder about 4 months back, which drained spontaneously forming a sinus. At presentation, this sinus was healed but patient had a new sinus track in axilla draining pus. This patient also had a history of constitutional symptoms. His investigations were indicative of infective arthritis of the shoulder with humeral head destruction with associated abscess extending along the back and rotator cuff muscles. We treated this patient with incision and drainage of the scapular abscess. Around 100 mL of pus was drained. Furthermore, anterior aspect of shoulder was exposed to debride shoulder joint. Mycobacterium TB was isolated on gene expert and the patient was started on anti- TB treatment regimen (ATT; DOTS- category I). On subsequent follow-up, the patient had complete resolution of symptoms within 4 months. His overall condition improved - his appetite increased and he also gained weight.
Conclusion: High degree of suspicion should be kept in mind in diagnosing shoulder TB. Once diagnosed, the prognosis is excellent with appropriate treatment-ATT alone or in combination with surgical debridement.
Keywords: Tuberculosis, shoulder, scapular abscess.
Tuberculosis (TB) has been a health concern for several years. Osteoarticular involvement occurs in up to 2% of all TB patients [1]. Spinal TB is the most common amongst bone and joint TB cases. Shoulder TB is very rare manifestation of the extra-pulmonary TB. It varies from an incidence rate of 0.9–1.7% [2]. There are two varieties of shoulder TB: Caries sicca (dry form) and caries exudata (abscess form). Caries sicca manifests as marked wasting and painful movement restriction, whereas caries exudata manifests as cold abscess and swelling [3]. Very few cases of tubercular osteomyelitis of shoulder have been reported in literature till date. We treated one patient with TB of shoulder joint, presenting with scapular abscess successfully. We reviewed previous reports of shoulder TB in literature to analyze the common clinical presentation and modality of treatment for the same.
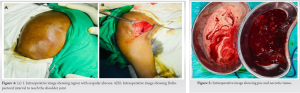
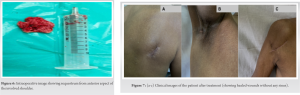
A 50-year-old male presented to us with complaints of swelling, measuring 10*9*4 cm in size over right scapular area since 2 months, which was gradually progressive. There was no history of trauma to the involved area. This swelling was tender, with some local warmth present. The patient had similar swelling on the anterior aspect of right shoulder about 4 months back, which drained spontaneously forming a sinus. At presentation, this sinus was healed but patient had a new sinus track in axilla draining pus. There was gross wasting of muscles and decreased range of motion of shoulder. On eliciting further history, the patient gave history of evening rise of temperature along with loss of weight and a decrease in appetite. There was no history of Koch’s or Koch’s contact. No significant comorbidities. No other significant history was elicited. This patient was started on oral antibiotics by a general practitioner before presenting to us. Radiographs of the involved part showed destruction of the humeral head along with sequestrum formation and generalized osteopenia. Blood investigations showed an elevated Erythrocyte Segmentation Rate, C-Reactive Protein (CRP), and White Blood Cell counts. Ultrasound demonstrated a hypoechoic collection measuring 10*4.4*8.8 cm with multiple central and peripheral foci within. Along with this, there was evidence of an irregular hypoechoic collection measuring 1.7*1.4*1.2 cm in right axilla tracking up to the skin surface. MRI demonstrated moderate sized collection/abscess within subcutaneous plane of the back, measuring 10*4.3*10 cm overlying the infraspinatus muscle, communicating with joint cavity. Furthermore, there was complete destruction of humeral head with marked osteolysis and marrow edema. These findings were indicative of infective arthritis of the shoulder with humeral head destruction with associated abscess extending along the back and rotator cuff muscles. We treated this patient with incision and drainage of the scapular abscess. Around 100 mL of pus was drained. Furthermore, anterior aspect of shoulder was exposed using deltopectoral approach to debride shoulder joint. Sequestrum was removed, which measured approximately 4*4cm. Tissue and pus samples were sent for bacterial culture, Acid Fast Bacillus smear, histopathology, and Xpert MTB/RIF test. Mycobacterium TB (MTB) was isolated on gene expert and the patient was started on anti-TB treatment regimen (ATT; DOTS-category I). Along with this, he was advised high protein diet. On subsequent follow-up, the patient had complete resolution of symptoms within 4 months. His overall condition improved – his appetite increased and he also gained weight.
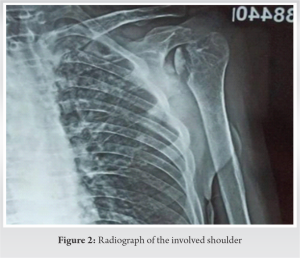

TB is a major health problem in developing countries. TB mostly affects the lungs. Musculoskeletal TB constitutes around 10–35% cases of extrapulmonary TB and only 2% of all cases of TB. <2% of all skeletal TB affects the shoulder joint [2]. One of the difficulties in diagnosing skeletal TB is its nonspecific clinical presentation. Therefore, high index of suspicion is necessary. Clinically, skeletal TB presents with pain and swelling. Occasionally, it may present with a discharging sinus. Constitutional symptoms may or may not be present. Clinically, the findings with restricted shoulder movements may mimic frozen shoulder and the diagnosis is delayed or missed. Erythrocyte sedimentation rate and CRP may be raised. Radiographs usually show osteopenia, osteolytic lesion with poorly defined edges and varying amounts of sclerosis and periostitis [2, 4]. CT and MRI are useful to delineate the extent of the lesion. The differential diagnosis for a lytic lesion in humeral head on radiograph are infections both bacterial and fungal, tumors such as bone cysts, telangiectatic osteosarcoma, sarcoidosis, or eosinophilic granuloma [4, 5]. Positive Ziehl-Neelsen staining and/or a positive culture of MTB from the affected bone or joint are the gold standard for diagnosing osteoarticular TB. The Xpert MTB/RIF (resistance to rifampicin) test is highly accurate for TB detection and offers early identification of rifampin resistance [6]. We did a review of literature [7, 8, 9, 10] of shoulder TB till date. Out of these, most presented secondary to pulmonary TB and without any scapular abscess. The most common presentation was pain and swelling of the involved area, with a few patients presenting with discharging sinus. Constitutional symptoms are present in few patients. Commonly affected age group is between 50 and 60 years. Primary treatment modality remained anti-tubercular drug therapy (ATT). Our patient presented with a scapular abscess secondary to TB of shoulder joint, which was secondarily infected with bacteria. Since patient was started on antibiotics, bacteria were not isolated in culture. Sequestrum from humeral head was evident on radiograph. Therefore, he had to be taken up for incision and drainage of the abscess with sequestrectomy from the humeral head. Along with this, he was started on ATT. He showed complete resolution of the disease after completing 9 months of ATT course.
High degree of suspicion should be kept in mind in diagnosing shoulder TB. Once diagnosed, the prognosis is excellent with appropriate treatment-ATT alone or in combination with surgical debridement.
TB of shoulder joint is an uncommon presentation. Any sinus or swelling (scapular region or elsewhere around shoulder) should be suspected and evaluated for TB, especially in endemic areas like India.
References
- 1.Morris BS, Varma R, Garg A, Awasthi M, Maheshwari M. Multifocal musculoskeletal tuberculosis in children: Appearances on computed tomography. Skeletal Radiol 2002;31:1-8. [Google Scholar]
- 2.Tuli SM. Tuberculosis of the Skeletal System. 2nd ed. New Delhi, Jaypee Brothers Medical Publisher P Ltd; 1993. [Google Scholar]
- 3.Patel PR, Patel DA, Thakker T, Shah K, Shah VB. Tuberculosis of shoulder joint. Indian J Orthop 2003;37:7 [Google Scholar]
- 4.Singh A, Chatterjee P, Pai MC, Chacko RT. Tuberculous osteomyelitis of the scapula masquerading as metastasis. Radiology Case 2009;3:27-31. [Google Scholar]
- 5.Teo HE, Peh WC. Skeletal tuberculosis in children. Pediatr Radiol 2004;34:853-60. [Google Scholar]
- 6.Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, Dendukuri N. Xpert® MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev 2014;2014:CD009593. [Google Scholar]
- 7.Deshmukh A, Deo S, Salgia AK, Agarwal T. A rare unusual case presentation of the tuberculosis of the shoulder joint. J Orthop Case Rep 2013;3:23-5. [Google Scholar]
- 8.Kizildag B, Sener A, Komurcu E, Karatag O, Kosar S. Glenohumeral joint tuberculosis with multiple cold abscesses: An uncommon cause of shoulder pain. Case Rep 2013;2013:bcr2013200592. [Google Scholar]
- 9.Longo UG, Marinozzi A, Cazzato L, Rabitti C, Maffulli N, Denaro V. Tuberculosis of the shoulder. J Shoulder Elbow Surg 2011;20:19-21. [Google Scholar]
- 10.Darraj M. Delayed presentation of shoulder tuberculosis. Case Rep Infect Dis 2018;2018:8591075. [Google Scholar]







