In patients with lumbar degenerative disease presenting with L3 radiculopathy, it is necessary to consider the possibility of fragility fracture of the pelvis and perform MRI imaging to make an early diagnosis when the symptoms change.
Dr. Masahiro Inoue, Department of Orthopaedic Surgery, Eastern Chiba Medical Center, Togane, Japan, 3-6-2 Okayamadai, Togane City, Chiba 283-8686, Japan. E-mail: masain_96@hotmail.com
Introduction: Fragility fractures of the pelvis (FFP) are caused by low-energy impacts and can occur spontaneously in patients with severe osteoporosis. The clinical symptoms of FFP are frequently vague and nonspecific. Moreover, the symptoms of FFP can mimic lumbar spine pathologies. Therefore, accurate diagnosis of FFP is often difficult and the fracture may be misdiagnosed as lumbar degenerative disease. However, little is known regarding what kind of symptoms due to lumbar degenerative disease are similar to the symptoms of FFP.
Case Report: We encountered two cases in which FFP developed during the treatment of lumbar degenerative disease with radiculopathy. Both patients had undergone conservative treatment for lumbar degenerative disease, but their symptoms gradually worsened and they presented with gait disturbance. FFP was diagnosed by imaging, and surgery was required in one case. Both cases showed L3 foraminal stenosis on the image, and the symptoms of L3 radiculopathy presented with thigh pain, hip pain, and knee pain, which is similar to the pain site of FFP. Therefore, diagnosis of FFP was difficult.
Conclusion: In lumbar degenerative diseases presenting with radiculopathy, the pain site may be similar to that of FFP, which may make diagnosis of FFP difficult. Therefore, especially in patients with lumbar degenerative disease presenting with L3 radiculopathy, it is necessary to consider the possibility of FFP and perform MRI imaging to make an early diagnosis when the symptoms change.
Keywords: Fragility fracture of pelvis, lumbar degenerative disease, surgery, insufficiency fracture, magnetic resonance imaging.
Fragility fractures of the pelvis (FFP) are caused by a low-energy impact and can occur spontaneously in patients with severe osteoporosis [1, 2]. Because FFP is a fragile bone fracture, the treatment method is different from pelvic ring fractures associated with high-energy trauma. In FFP, the degree of posterior pelvic ring injury is graded based on the Rommens classification [1]. FFP Type-I is an isolated anterior pelvic ring fracture without the involvement of the posterior structures. FFP Type-II is a non-displaced fracture of the posterior pelvic ring. FFP Type-III is a displaced unilateral fracture of the posterior pelvic ring with simultaneous instability of the anterior pelvic ring. FFP Type-IV is a bilateral displaced posterior pelvic ring injury [3]. Most FFPs are minimally displaced and are conservatively treated particularly in the early phase; however, surgical stabilization should be recommended for patients who have persistent pain and apparent difficulty in mobilization [4, 5]. On the basis of the Rommens classification, FFP Type-I can be treated conservatively. In many cases, FFP Type-II can also be treated conservatively. When conservative treatment fails, percutaneous fixation is performed. FFP Type-III and FFP Type-IV are treated operatively [3]. Accurate diagnosis of FFP is often difficult and delayed. One key reason is that fracture involves a few dislocations, and it is often difficult to diagnose with radiographs [6]. In addition, the clinical symptoms of FFP are frequently vague and non-specific. Because the symptoms of FFP can mimic lumbar spine pathologies, initial imaging in FFP is frequently targeted at the lumbar spine rather than at the pelvis [7]. Therefore, the fracture may be misdiagnosed as lumbar degenerative disease. However, little was known about the kind of symptoms due to lumbar degenerative disease that were similar to those of FFP. In the present case reports, we present two patients with FFP who were initially diagnosed lumbar degenerative disease. We describe the difficulties in the diagnosis of FFP as it occurred in conjunction with lumbar degenerative disease, and compare symptoms of FFP with those of lumbar degenerative disease.
Case 1
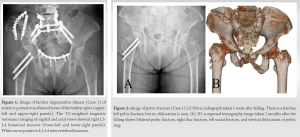
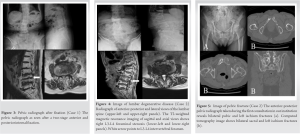
A 73-year-old woman with a medical history of a right femoral neck fracture, bilateral total knee arthroplasty, osteoporosis, and gastric cancer underwent a medical examination in our institution. Osteoporosis (bone mineral density compared with the mean bone mineral density of young adults; lumbar 0.80 and hip 0.40) was treated with bisphosphonate and Vitamin D preparation. She had no other comorbidities. She had degenerative lumbar scoliosis and complained of low back pain, buttock pain, and right lower limb pain for several years due to L3-L4 foraminal stenosis (Fig. 1). The pain was treated with medication and with an L3 nerve root block in our institution, but the pain gradually worsened. A week after she fell down at home, she visited our institution because of worsening pain in the right buttock, groin area, and calf muscles. Physical examination revealed right groin pain associated with weight-bearing and difficulty raising the right leg due to pain in the groin. No symptoms were noted in the left lower limb. The anterior-posterior pelvic radiograph revealed a left pubic fracture (Rommens classification Type-Ia) but did not identify fractures of the vertebrae, right pelvis, or proximal femur (Fig. 2a).
Because there were no significant symptoms on the left side (buttock pain, groin pain, and lower limb pain), the patient was diagnosed with acute exacerbation of radiculopathy. An L3 nerve root block was performed as a treatment for pain, and the pain was temporarily relieved. Therefore, she was provided conservative treatment continuously. Two months after falling, the lower limb pain, groin pain, and pubic pain under weight-bearing worsened and she was unable to stand and walk because of the pain. Computed tomography (CT) showed bilateral pubic fractures, bilateral ischium fractures, right iliac fracture, left sacral fracture, and a vertical shear fracture of the pelvic ring (Fig. 2b). She was diagnosed with FFP of Rommens classification Type-IVc. She was hospitalized for surgery, and a two-stage anterior and posterior internal fixation was performed (Fig. 3). 2 years after surgery, she was able to walk with a walking stick. Antiosteoporotic treatment was changed to denosumab and Vitamin D.
Case 2
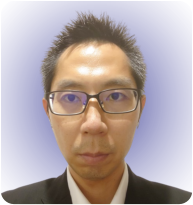
A 92-year-old woman with a medical history of old myocardial infarction, valvular disease, and osteoporosis. Osteoporosis (bone mineral density compared with the mean bone mineral density of young adults; lumbar 0.83 and hip 0.63) was treated with Bazedoxifene acetate and Vitamin D preparation. She had no other comorbidities. Following complaints of bilateral lower limb pain and bilateral lower limb weakness, she was diagnosed with L3-5 spinal canal and L3-4 bilateral foraminal stenosis (Fig. 4). The patient was treated with medication and physical therapy. However, the low back pain, bilateral lower limb pain, and left groin pain gradually worsened, and she was unable to walk due to these symptoms. Therefore, she had medical examination in our institution. Physical examination revealed tenderness of the left groin area and worsening left lower limb weakness. The anterior-posterior pelvic radiograph revealed bilateral pubic and left ischium fractures (Fig. 5a). CT showed bilateral sacral, bilateral pubic, and left ischium fractures (Fig. 5b). The patient was diagnosed with FFP of Rommens classification Type-IVc and was hospitalized. She was treated conservatively, with best rest because she was able to sit. Her symptoms improved and she was permitted to start of walker training 12 days after hospitalization. She was able to walk with full-weight bearing 1 month after hospitalization. Anti-osteoporotic treatment was changed to parathyroid hormone (PTH).
We encountered two cases in which FFP developed during the treatment of lumbar degenerative disease with radiculopathy, and in which diagnosis of FFP was difficult. We identified two important clinical issues. First, FFP coexisting with the lumbar degenerative disease was difficult to diagnose because FFP presents similar symptoms to those of lumbar degenerative disease with radiculopathy, especially L3 nerve radiculopathy. Second, fractures can progress gradually in FFP. As mentioned above, FFP presents similar symptoms to those of lumbar degenerative disease with radiculopathy. General symptoms of FFP include low back pain, buttock pain, groin pain, and sciatic neuralgia, where pseudoradicular pain may also occur [8, 9]. In particular, symptoms of L3 root radiculopathy can present with thigh pain, hip pain, and knee pain, which are similar to the pain site of FFP [10]. In the present cases, groin pain and thigh pain were initially diagnosed as L3 symptoms with similar pain sites. Therefore, we concluded that the neurological symptoms had exacerbated due to the fall or exercise. Attention should be given to the possibility of lumbar degenerative disease with radiculopathy of either L2 or L3 occurring, as the groin and thigh pain are similar to the symptoms of FFP. In addition, weight-bearing pain has been reported to be a more common symptom in FFP than in lumbar degenerative disease [2]. Hence, weight-bearing pain can be useful for differential diagnosis between FFP and degenerative lumbar disease. It is also necessary to consider the possibility of causing FFP during the treatment of lumbar degenerative diseases associated with osteoporosis. In the diagnosis of FFP, magnetic resonance imaging (MRI) was reported to be substantially better and preferable because of the inferior sensitivity of radiography and CT in detecting FFP [11]. A previous study reported that approximately 64.3% of FFP were diagnosed by lumbar spine MRI. Moreover, lumbar spine MRI was able to diagnose other comorbid causes of pain in 73.8% of patients with FFP [12]. Because the second case reported here had been treated at another hospital, FFP was already Rommens Type-Ⅳc at the first visit. Conversely, in first patient, the fracture was initially classified as Type-Ia as per the Rommens classification. However, during the conservative treatment, the fracture progressed to Type 4. Prolonged pain during conservative treatment is associated with fracture progression [13]. Fracture progression occurs in all fracture types, and most frequently in FFP Type-I. Fracture progression has been observed previously in 14.2% of patients undergoing conservative therapy [13]. Anti-osteoporotic treatment was indicated to improve bone quality and bone healing in fragility fractures [14]. Vitamin D deficiency was reported to be associated with FFP [15]. PTH is effective for osteoporosis in patients with FFP [6]. Therefore, Vitamin D preparation and PTH are recommended for osteoporosis in patients with FFP. In the current Case 1, a Vitamin D preparation was prescribed; however, PTH was not added because of the patient’s history of cancer. Even with the use of anti-osteoporosis treatment and dislocation progressed, and it was necessary to consider surgery immediately. We encountered two cases in which fragile fractures of the pelvis developed during treatment of lumbar degenerative disease with radiculopathy. In the present cases, a cognitive bias led to a failure in diagnosing FFP during the treatment of lumbar degenerative disease. However, the lumbar degenerative disease and FFP have many similarities in terms of patient characteristics and symptoms, which make the differentiation difficult. Moreover, attention should be given to avoid missing FFP in patients with groin pain where image findings suggest L2 or L3 nerve radiculopathy.
We encountered two cases in which FFP developed during treatment of lumbar degenerative disease with radiculopathy, and diagnosis of FFP was difficult. FFP presents similar symptoms to those of lumbar degenerative disease with radiculopathy, especially L3 nerve radiculopathy. Therefore, if there are changes in the symptoms of lumbar degenerative disease with osteoporosis, it is necessary to consider the possibility of FFP. Further, MRI imaging should be performed to make an early diagnosis, because dislocation may progress even with conservative treatment for FFP.
FFP coexisting with the lumbar degenerative disease was difficult to diagnose. However, there were no previous reports referencing what specific symptoms are likely to be misdiagnosed for lumbar degenerated disease. In the present report, we reported that FFP presents similar symptoms to those of lumbar degenerative disease with radiculopathy, especially L3 nerve radiculopathy. In the case of patients with lumbar spine disease who have nerve root symptoms, it is necessary to evaluate the FFP when the symptoms change or when groin pain associated with weight-bearing is observed.
References
- 1.Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 2013;44:1733-44. [Google Scholar]
- 2.Tsiridis E, Upadhyay N, Giannoudis PV. Sacral insufficiency fractures: Current concepts of management. Osteoporos Int 2006;17:1716-25. [Google Scholar]
- 3.Rommens PM, Dietz SO, Ossendorf C, Pairon P, Hofmann A. Fragility fractures of the pelvis: Should they be fixed? Acta Chir Orthop Traumatol Cech 2015;82:101-12. [Google Scholar]
- 4.Ueda Y, Inui T, Kurata Y, Tsuji H, Saito J, Shitan Y. Prolonged pain in patients with fragility fractures of the pelvis may be due to fracture progression. Eur J Trauma Emerg Surg 2021;47:507-13. [Google Scholar]
- 5.Rommens PM, Arand C, Hofmann A, Wagner D. When and how to operate fragility fractures of the pelvis? Indian J Orthop 2019;53:128-37. [Google Scholar]
- 6.Na WC, Lee SH, Jung S, Jang HW, Jo S. Pelvic insufficiency fracture in severe osteoporosis patient. Hip Pelvis 2017;29:120-6. [Google Scholar]
- 7.Sudhir G, Kalra KL. Acharya S, Chahal R. Sacral insufficiency fractures mimicking lumbar spine pathology. Asian Spine J 2016;10:558-64 [Google Scholar]
- 8.Tamaki Y, Nagamachi A, Inoue K, Takeuchi M, Sugiura K, Omichi Y, et al. Incidence and clinical features of sacral insufficiency fracture in the emergency department. Am J Emerg Med 2017;35:1314-6. [Google Scholar]
- 9.Ungaro E, Astore F, Bonora C, Ferrari MC. Groin pain in sacral insufficiency fracture. Avoiding delayed diagnosis. Int J Osteopath Med 2011;14:106-9. [Google Scholar]
- 10.Hirabayashi H, Takahashi J, Hashidate H, Ogihara N, Tashiro A, Misawa H, et al. Characteristics of L3 nerve root radiculopathy. Surg Neurol 2009;72:36-40. [Google Scholar]
- 11.Cabarrus MC, Ambekar A, Lu Y, Link TM. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am J Roentgenol 2008;191:995-1001. [Google Scholar]
- 12.Kim YY, Chung BM, Kim WT. Lumbar spine MRI versus non-lumbar imaging modalities in the diagnosis of sacral insufficiency fracture: A retrospective observational study. BMC Musculoskelet Disord 2018;19:257. [Google Scholar]
- 13.Rommens PM, Arand C, Hopf JC, Mehling I, Dietz SO, Wagner D. Progress of instability in fragility fractures of the pelvis: An observational study. Injury 2019;50:1966-73. [Google Scholar]