The use of long hip cephalomedullary nails appears to be a very good choice in the treatment of intertrochanteric hip fractures combined with ipsilateral atypical fractures of the femoral diaphysis.
Dr. Georgios F Georgiadis, Department of Orthopaedics and Osteoporosis, Asclepieion Voulas General Hospital, Voula, 16673, Athens, Greece. E-mail: gegeorgiades@yahoo.com
Introduction: Osteoporotic hip fractures can occur at the femoral neck and intertrochanteric area, with the peritrochanteric fracture being responsible for half of these fractures in the geriatric population. Atypical femoral fractures have been associated in the literature with long-term use of bisphosphonates or denosumab. However, few cases with the characteristics of these fractures have been reported in the past in patients not receiving antiresorptive drugs. To date, no combination of an intertrochanteric fracture with an impending incomplete atypical fracture of the ipsilateral femoral diaphysis has been previously reported in the literature.
Case Report: We present a rare case of a 97-year-old female patient with an intertrochanteric femoral fracture, with a preexisting focal cortical thickening along the lateral aspect of the ipsilateral proximal femoral diaphysis which is a warning sing for an incomplete atypical femoral fracture. A long gamma nail was used to fix the intertrochanteric fracture and simultaneously to stabilize and protect the area of the atypical femoral fracture.
Conclusion: Any patient with a peritrochanteric hip fracture who was under long-term treatment with antiresorptive agents against osteoporosis, or has other risk factors predisposing to atypical femoral fracture, should undergo a thorough radiological examination of the ipsilateral femur, to exclude the possibility of simultaneous presence of both of the above pathologies. In any such case, the use of a long hip cephalomedullary nail seems to be the best treatment option, because it can treat both fractures at the same time.
Keywords: Intertrochanteric hip fracture, atypical femoral fracture, long hip cephalomedullary nail.
Globally, the incidence of osteoporotic hip fractures increases as the population ages; over 8 million, hip fractures per year are expected worldwide by 2050 [1]. Peritrochanteric fractures account for half of osteoporotic hip fractures that occur in the geriatric population [2]. Various operative techniques and implants have been used to treat those fractures; however, short hip cephalomedullary nail (SHCN) became the gold standard since its introduction [3]. Long hip cephalomedullary nails (LHCN) are used when the peritrochanteric fracture is extended more than 3 cm below the lesser trochanter, and when there is another fracture more distal to the femoral diaphysis [3]. Although antiresorptive agents such as bisphosphonates (BPs) and denosumab are effective at preventing osteoporotic hip fractures among older adults; yet, many patients still have fractures during treatment for osteoporosis with those agents and more often when left untreated at all for osteoporosis [4, 5]. On the other hand, prolonged antiresorptive therapy is believed to be associated with atypical femoral fractures (AFFs), which could rarely occur in patients who never used antiresorptive therapy [6, 7]. According to the American Society for Bone and Mineral Research (ASBMR) task force an AFF, usually but not always begins as a small focal beak-like cortical thickening of the lateral cortex which is usually the result of a focal periosteal/endosteal thickening related to a microfracture [8]. Subsequently, a small incomplete lucent fracture line may appear in the lateral cortex, which may later progress to a complete, non-comminuted, transverse, or with a medial spike fracture, involving both the lateral and medial cortex. We present a case of an intertrochanteric femoral fracture in combination with a focal lateral cortex thickening of the femoral diaphysis distal to the fracture, treated with a long gamma nail (LGN), to treat both pathologies.
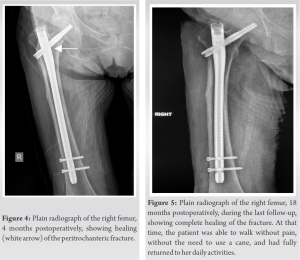
A 97-year-old woman presented to the emergency department of our hospital with an intertrochanteric fracture of the right femur, after falling from standing height. Plain radiographs revealed an AO A3.1 peritrochanteric fracture and a focal thickening of the lateral cortex of the diaphysis of the right femur (Fig. 1). Multidetector computed tomography of pelvis and femurs demonstrated a lateral cortex thickening of the shaft without a fracture line (Fig. 2). 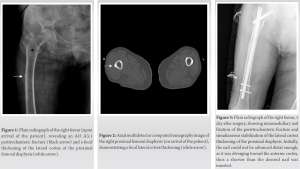
To the best of our knowledge, no combination of an intertrochanteric fracture with an impending incomplete diaphyseal atypical fracture of the ipsilateral femur has been previously reported in the literature. It is rather paradoxical that the patient presented with an intertrochanteric fracture after sustaining a standing height fall while she already had focal thickening of the lateral cortex of the femoral diaphysis. The patient never had a DXA measurement before the appearance of an osteoporotic vertebral fracture, and 6 months later, she had an osteoporotic hip fracture. Osteoporotic fractures are defined as fractures in bone areas associated with low BMD [9], and as the population ages, their incidence will increase [1]. Osteoporotic hip fractures can occur at the femoral neck and intertrochanteric area with the peritrochanteric fracture being responsible for half of these fractures in the geriatric population [2]. Cephalomedullary nailing has emerged as the most popular surgical technique for the treatment of peritrochanteric femoral fracture patterns in the past decade [10]. Cephalomedullary nails offer lower operation time, intraoperative blood loss, and post-operative complications, as well as higher biomechanical advantages against other implants [3]. Both SHCN and LHCN showed no differences on the functional outcome and the complications rate at the treatment of peritrochanteric fractures. SHCN has become the gold standard in the treatment of peritrochanteric fractures, because they are easier to insert, with shorter surgery time, less blood loss and radiographic exposure, and shorter hospital stay [3]. However, the use of the LHCN is unavoidable when the fracture extends more than three centimeters from the lesser trochanter and when there is another complete, incomplete, or impending fracture more distally in the femoral diaphysis, to stabilize both fractures. According to the ASBMR, usually an AFF begins as a focal lateral femoral cortex thickening (“beaking” or “flaring”) or endosteal thickening, which is usually the result of a microfracture [8]. Subsequently, there may be an appearance of a small incomplete lucent fracture line in the region of the periosteal thickening, which may later progress to a complete fracture involving both the lateral and medial cortex. Our patient presented focal lateral cortex thickening of the femoral diaphysis at the subtrochanteric region without an incomplete fracture line. Although long-term use of antiresorptive agents is thought to be associated with AFFs, the patient received only one dose of denosumab after the vertebral fracture and before the occurrence of the osteoporotic hip fracture. Low-energy femoral fractures with the characteristic radiographic pattern of atypical fractures have been reported in the past in patients not receiving BPs or denosumab, but presenting with other risk factors for AFFs, such as genetic metabolic bone disorders (hypophosphatasia and osteopetrosis), femoral geometry parameters (lateral femoral bowing and varus hip alignment), factors associated with deterioration of bone quality [use of certain medications (glucocorticoids, proton pump inhibitors), other comorbidities (type 1 diabetes, rheumatoid arthritis, and other autoimmune diseases)], and conditions that cause impaired bone mineralization (osteomalacia and vitamin D deficiency) [11,12,13,14]. In the present study, the patient had vitamin D deficiency and excessive anterolateral femoral bowing. We believe that in cases of a peritrochanteric fracture combined with an ipsilateral phenotypic expression of an AFF, the surgical plan and selection of the fixation device should address both pathologies. The LHCN has the ability to treat both peritrochanteric and ipsilateral diaphyseal AFF, which offers shorter surgical and fluoroscopy time and less blood loss, morbidity, and mortality. Its insertion can be challenging in case of severe femoral bowing, as it increases the risk of perforation of the anterior femoral cortex. The correct nail entry point and the use of a shorter nail as in the present case can prevent this complication. The presence of osteoporosis and two osteoporotic fractures in our patient increases the risk of another osteoporotic fracture and makes it mandatory to administer anti-osteoporotic treatment. Since the focal cortical thickening along the lateral aspect of the proximal femoral shaft could not be associated with the use of antiresorptive agents (patient received only one dose of denosumab), we considered it appropriate to administer antiresorptive therapy (BPs or denosumab) for osteoporosis and the prevention of new osteoporotic fractures, especially in our case where the bone turnover markers showed increased bone turnover, otherwise anabolic therapy with teriparatide should be used. Two months after fracture healing, our patient presented increased bone turnover markers and she received again treatment with denosumab. Denosumab does not appear to delay fracture healing or causes other complications when given at or near the time of fracture while, on the other hand, this treatment reduces the risk of a subsequent osteoporotic fracture [15]. Calcium and vitamin D administration were also necessary to increase low vitamin D levels and reduce high PTH levels. Patients with peritrochanteric hip fracture, who are receiving long-term antiresorptive therapy for osteoporosis or have other risk factors predisposing to AFFs, should undergo a thorough radiological examination of the entire femur, to exclude the coexistence of both pathological conditions.
Both short and long cephalomedullary hip nails offer safe and predictable results for the management of peritrochanteric hip fractures. In cases where an intertrochanteric hip fracture is combined with focal thickening of the lateral cortex in the subtrochanteric or diaphyseal region of the femur, both issues should be treated accordingly, to avoid post-operative complications such as refracture distal to the nail. The use of LHCN can be a proper solution in such a case to fix theintertrochanteric fracture and at the same time to stabilize and protect the area of focal thickening.
Any patient with a peritrochanteric hip fracture who has been on long-term treatment with antiresorptive agents against osteoporosis, or has other risk factors for an atypical femoral fracture, should undergo a thorough radiological examination of the ipsilateral femoral diaphysis, to exclude the simultaneous presence of both of the above pathologies. In any such case, the use of a long hip cephalomedullary nail seems to be the best treatment option, because it can treat both fractures at the same time.
References
- 1.Sambrook P, Cooper C. Osteoporosis. Lancet 2006;367:2010-8. [Google Scholar]
- 2.Lindskog DM, Baumgaertner MR. Unstable intertrochanteric hip fractures in the elderly. J Am Acad Orthop Surg 2004;12:179-90. [Google Scholar]
- 3.Vaughn J, Cohen E, Vopat BG, Kane P, Abbood E, Born C. Complications of short versus long cephalomedullary nail for intertrochanteric femur fractures, minimum 1 year follow-up. Eur J Orthop Surg Traumatol 2015;25:665-70. [Google Scholar]
- 4.Zullo AR, Zhang T, Lee Y, McConeghy K, Daiello LA, Kiel DP, et al. Effect of bisphosphonates on fracture outcomes among frail older adults. J Am Geriatr Soc 2019;67:768-76. [Google Scholar]
- 5.Papapoulos S, Lippuner K, Roux C, Lin CJ, Kendler DL, Lewiecki EM, et al. The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: Results from the FREEDOM extension study. Osteoporos Int 2015;26:2773-83. [Google Scholar]
- 6.Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: A systematic review and meta-analysis. J Bone Miner Res 2013;28:1729-37. [Google Scholar]
- 7.Szolomayer LK, Ibe IK, Lindskog DM. Bilateral atypical femur fractures without bisphosphonate exposure. Skeletal Radiol 2017;46:241-7. [Google Scholar]
- 8.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American society for bone and mineral research. J Bone Miner Res 2014;29:1-23. [Google Scholar]
- 9.Kanis JA, Oden A, Johnell O, Jonsson B, De Laet C, Dawson A. The burden of osteoporotic fractures: A method for setting intervention thresholds. Osteoporosis Int 2001;12:417-27. [Google Scholar]
- 10.Anglen JO, Weinstein JN, American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: Changing pattern of practice. A review of the American board of orthopaedic surgery database. J Bone Joint Surg Am 2008;90:700-7. [Google Scholar]
- 11.Nguyen HH, Van de Laarschot DM, Verkerk AJ, Milat F, Zillikens MC, Ebeling PR. Genetic risk factors for atypical femoral fractures (AFFs): A systematic review. JBMR Plus 2018;2:1-11. [Google Scholar]
- 12.Sasaki S, Miyakoshi N, Hongo M, Kasukawa Y, Shimada Y. Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: A case series. J Bone Miner Metab 2012;30:561-7. [Google Scholar]
- 13.Rasmussen NH, Dal J, De Vries F, Van den Bergh JP, Jensen MH, Vestergaard P. Diabetes and fractures: New evidence of atypical femoral fractures? Osteoporos Int 2020;31:447-55. [Google Scholar]
- 14.Mizunashi K, Furukawa Y, Katano K, Abe K. Effect of omeprazole, an inhibitor of H+, K(+)-ATPase, on bone resorption in humans. Calcif Tissue Int 1993;53:21-5. [Google Scholar]
- 15.Adami S, Libanati C, Boonen S, Cummings SR, Ho PR, Wang A, et al. Denosumab treatment in postmenopausal women with osteoporosis does not interfere with fracture-healing: Results from the FREEDOM trial. J Bone Joint Surg Am 2012;94:2113-9. [Google Scholar]