Intraarticular osteoid osteomas may cause paşn, swelling and mechanical symptoms. Coexistence of other intraarticular pathologies may overshadow it and detain the treatment. Diagnostic ankle arthroscopy is worth to consider both for diagnosis and treatment.
Dr. Arman Vahabi, Department of Orthopedics and Traumatology, Ege University School of Medicine, 35040, Izmir, Turkey. E-mail: armanvy@gmail.com
Background: Talus osteoid osteomas are often overlooked. This pathology, which can cause chronic ankle pain, should be kept in mind when evaluating differential diagnoses.
Case Report: A 21-year-old female applied to our clinic with chronic ankle pain diagnosed as talus OCD. The patient’s pain was refractory to non-operative treatments. The detection of talar osteoid osteoma is delayed due to atypical radiologic findings and coexistent osteochondral lesion of talus. The patient is treated with ankle arthroscopy with excellent results.
Conclusion: Chronic ankle pain causes severe functional limitations. Dealing with such cases especially in the young population, one should consider that atypical radiologic signs could have further meaning. When radiology fails to describe the lesion, ankle arthroscopy could be a good option, both for diagnosis and treatment.
Keywords: Case report, osteoid osteoma, talus, ankle arthroscopy.
Osteoid Osteoma is the third common bone tumor [1]. It is a “benign, primary, and bone-forming” lesion. A typical case of osteoid osteoma would be a young male in his 20s. Night pain that responses well to painkillers is the classical complaint that led clinician to diagnose, but it is not always easy to do so [2]. Some of the cases remain undiagnosed for a long time, even though they have complaints that resemble osteoid osteoma. Bone tenderness, local swelling, weakness, and atrophy are other clinical presentations [3]. Half of the osteoid osteomas involve femur or tibia, the probability of osteoid osteoma involving talus is higher than you possibly guess, ranking 4th among all sites with the percentage of 2–10% [4]. In most cases, plain radiography combined with computerized tomography is adequate for diagnosis. Plain radiography or magnetic resonance imaging (MRI) alone could mislead diagnosis since nidus may not be tracked [3, 4]. Although spontaneous regression is possible in osteoid osteomas, most of the patients require surgical intervention due to disturbing pain [5]. In recent years, radiofrequency ablation and surgical excision are preferable treatment methods for most cases, but when it comes to talar osteoid osteomas, total excision through ankle arthroscopy is the pioneer treatment method [6]. We report a case of talus osteoid osteoma with delayed diagnosis due to concealing pathology. One should keep in mind that the talus is not an extreme site for osteoid osteomas. Speaking of small bones, the possibility of not indicating classical radiological findings such as in diaphyseal osteoid osteoma could be misleading. That should be kept in mind when dealing with patients who have chronic ankle pain, especially when imaging studies reveal suspicious findings.
History
A 21-year-old female patient was admitted to our clinic with complaints of pain and swelling in her right ankle that had been going on for 4 years. She did not remember any significant injury to her ankle. She had a body-mass index of 25. She did not have any other medical condition. She described her pain as continuous pain, which worsens while loading, especially when going downstairs. She was able to attend daily activities, but she has not been able to participate in sports activities since the onset of pain. She was admitted to three other clinics before us, diagnosed with talar osteochondral lesion. All previous radiological reports were compatible with the diagnosis with no additional pathology reported. The patient had tried several nonsurgical treatments such as non-weight-bearing mobilization, splinting for a period but did not benefit. She described her pain as partially responsive to non-steroidal anti-inflammatory drugs.

Examination
In physical examination, no signs of instability were detected, despite the feeling of instability described by the patient. Further, examination revealed bilateral slight pes planovalgus and sensitivity on the anteromedial side of the ankle. Active ankle range of motion was slightly restricted in all three planes compared to the left one. These limitations in movements were thought to be due to sensitivity and were not considered to have any further clinical significance. The neurovascular examination was normal.
Diagnostic assessment
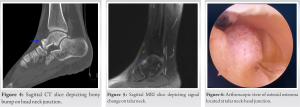
Evaluating the plain radiographs, the first thing to catch an eye was the osteochondral lesion of talus (OLT) on the medial talar articular surface (Fig. 1). That was the first trap that we and every other clinician prior to us fell into. Because there was too, a cortical irregularity on head-neck junction visible on lateral plain radiographs (Fig. 2). The same thing with the computerized tomography (CT), the most striking finding was again the OLT. Its maximum depth was 2 mm, and the chondral fragment was sclerosed, suggesting a chronic lesion (Fig. 3). There was a bony bump where the x-ray suggested cortical irregularity (Fig. 4), but it was not specific for any bony lesion. MRI, as other radiological assessments, was suggesting an OLT on the medial talar articular face. There was a signal change in the head-neck junction on the medial side of the talus (Fig. 5). Nevertheless, it was also not diagnostic, and not mentioned in MRI result. Assuming that if the final diagnosis would be an osteochondral lesion at the talar dome, the lack of edema in the subchondral area beneath OLT would be inconsistent with clinical findings. Considering the incompatibility of the lesion with the patient’s symptoms, and question marks about the nonspecific findings at the head-neck junction of the talus, we made direct contact with the radiology team. Again, their diagnosis was talar OLT, describing the other site as a nonspecific sclerosing bone lesion. Blood panels were all normal at preoperative phase. We were not comfortable with the current findings, and we decided that ankle arthroscopy would be beneficial for both the diagnosis and possible treatment. After discussing with the patient, ankle arthroscopy was scheduled. It has planned to evaluate the OCD site and the suspicious area at the first phase of the surgery. What to do next would be decided after the team had been convinced about the source of the pain.
Intervention
Surgery was performed under general anesthesia, with an above-the-knee tourniquet. Classic anteromedial and anterolateral joint portals were used. First The OLT site is examined; it was compatible with healed chronic chondral damage. No further intervention seemed necessary. Moving on to the talar head, an obvious juxtacortical bony lesion was observed in the medial of the head-neck junction (Fig. 6). Since the site and size of the lesion were compatible with our predictions, it was decided as the main pathology responsible for patient’ complaints. After the examination of all the other sites with scope to rule out any additional pathologies, we moved on to the excision step. The pedunculated lesion was freed with the help of an osteotome; the adhesion site was curetted, then cauterized. The sample was sent to pathological examination and the operation was terminated.
Follow-up and outcomes
The patient was pain-free, even on the night of the operation. She was allowed to bear full weight with a compressive bandage from the day 1. She did not need any painkillers afterward. At the 2nd week follow-up, the patient was pain-free and she had a full range of motion. Pathologic examination resulted as osteoid osteoma. At the 6th-month follow-up, the patient was free of symptoms. She had returned to sports activities without any discomfort. The Hind-Foot AOFAS score, which was 67 at the time of admission, was calculated as 94 at the 6th-month follow-up.
Osteoid osteoma of the lower extremity is mostly seen in long bones. Small bones are less frequently affected. Talus is the most affected bone in the ankle and foot region [6]. Edeiken’s classification suggests four types of osteoid osteomas. Among them, subperiosteal type is seen normally femoral neck, hands, feet, and neck of the talus [7]. Osteoid osteoma has distinctive radiological features such as nidus formation. Nidus is considered a diagnostic sign and can be defined in X-ray, computerized tomography, and MRI. Computerized tomography has the highest specificity and sensitivity among radiological diagnostic methods. Technetium-99 bone scintigraphy has also high sensitivity but has lower specificity compared to CT. Talar localization of osteoid osteoma is relatively rare; thus sometimes, it is a diagnostic challenge for physicians [8]. The road to diagnosis of talar osteoid osteoma mostly requires the combined use of plain radiographs and CT. In selected cases, scintigraphy could be helpful too. In the present case, the patient had X-ray, CT, and MRI studies. X-ray demonstrated osteochondral lesion at the talar dome with less significant changes on the head-neck junction of the talus. The MRI revealed an osteochondral lesion at the talar dome with no edema underneath. There was a small area with a signal change on the head-neck junction of the talus, which has not mentioned in the MRI result. Jordan et al. showed that an MRI study could diagnose 65% of osteoid osteoma cases localized at the ankle and foot region [4]. Based on this finding they suggested the usage of CT scan and scintigraphy for suspected cases. Even though CT is considered the golden standard method to detect nidus formation of osteoid osteoma; in our case, CT ailed to detect nidus formation. Database research revealed only one case, in which CT is failed to diagnose osteoid osteoma, reported by David et al. [9]. In that case, MRI succeeded to demonstrate nidus unlike our patient. Since she had a coexistent osteochondral lesion at the talar dome, the diagnostic process in our patient was more confusing. To the best of our knowledge, there is no reported case with an osteochondral lesion of talus accompanying osteoid osteoma on the talar neck in the literature. The previous studies suggested that in cases with osteoid osteoma on the talus, diagnosis time might take up to 4 years [10]. The coincidence of these two conditions in one patient made diagnosis even more difficult and thus delayed the treatment. Osteoid osteomas of intra-articular localization may have different clinical features. Nocturnal pain alleviates with non-steroidal anti-inflammatory drugs or salicylates causes high suspicion for osteoid osteoma. Different from extra-articular ones, patients with intra-articular osteoid osteomas have a lower frequency of nocturnal pain. Intra-articular type of osteoid osteoma presents with joint swelling, ankle pain, recurrent ankle sprains, and may mimic arthrosynovitis [8]. In the presented case, the patient had joint swelling and daytime pain with loading. Information gathered from radiological findings suggested the diagnosis of the osteochondral lesion of the talus even if the chronic appearance and lack of edema were not fully explaining the clinical picture. The conservative treatment methods should be considered in patients with non-displaced osteochondral lesions of the talus [11]. The current literature failed to suggest level I evidence treatment of choice in the setting of the osteochondral lesion of the talus. If conservative treatment fails, like in our case, the surgical option should come into question. Looking at what we had, performing ankle arthroscopy to evaluate osteochondral lesion of talus and the suspicious sclerotic area seemed appropriate. The utilization of non-motorized tools during arthroscopy is suggested by current literature. Usage of a motorized shaver to remove the tumor could lead to incorrect pathological diagnosis since there would be a fragmented the sample [12]. Complete removal of the lesion must be achieved since the failure to do so may cause recurrences. Talar osteoid osteomas could have confusing symptoms that cause late diagnosis. Misdiagnosis could lead to unsatisfactory treatments. Even with a correct preliminary diagnosis, a poor surgical technique could cause recurrence or inappropriate pathological sampling.
Considering the information provided by the previously published literature, our inference from this case is that in chronic ankle pain cases with suspicious clinical and radiological findings, ordering CT by mentioning that there is a suspicion of osteoid osteoma to the radiologist which could be in help with diagnosis alongside with X-ray and MRI. If it fails to solve the problem, an ankle arthroscopy should be discussed with the patient as a tool for both diagnosis and treatment.
Even with improved radiological assessments, clinical findings and patient history stand its important. In patients with characteristic symptoms and demographic findings, osteoid osteoma should kept in mind despite lack of diagnostic radiologic findings.
References
- 1.Zhang Y, Rosenberg AE. Bone-forming tumors. Surg Pathol Clin 2017;10:513-35. [Google Scholar]
- 2.Boscainos PJ, Cousins GR, Kulshreshtha R, Oliver TB, Papagelopoulos PJ. Osteoid osteoma. Orthopedics 2013;36:792-800. [Google Scholar]
- 3.Francesco B, Andrea LA, Vincenzo S. Intra-articular osteoid osteoma of the lower extremity: Diagnostic problems. Foot Ankle Int 2002;23:264-7. [Google Scholar]
- 4.Jordan RW, Koç T, Chapman AW, Taylorm HP. Osteoid osteoma of the foot and ankle-a systematic review. Foot Ankle Surg 2015;21:228-34. [Google Scholar]
- 5.Campanacci M, Ruggieri P, Gasbarrini A, Ferraro A, Campanacci L. Osteoid osteoma. Direct visual identification and intralesional excision of the nidus with minimal removal of bone. J Bone Joint Surg Br 1999;81:814-20. [Google Scholar]
- 6.Ge SM, Marwan Y, Addar A, Algarni N, Chaytor R, Turcotte RE. Arthroscopic management of osteoid osteoma of the ankle joint: A systematic review of the literature. J Foot Ankle Surg 2019;58:550-4. [Google Scholar]
- 7.Edeiken J, DePalma AF, Hodes PJ. Osteoid osteoma. (Roentgenographic emphasis). Clin Orthop Rel Res 1966;49:201-6. [Google Scholar]
- 8.Carneiro BC, Da Cruz İA, Filho AG, Silva IP, Guimarães JB, Silva FD, et al. Osteoid osteoma Imaging 2021;12:32. [Google Scholar]
- 9.David P, LegnameM, Dupond M. Arthroscopic removal of an osteoid osteoma of the talar neck. Orthop Traumatol Surg Res 2009;95:454-7. [Google Scholar]
- 10.Dubuc JE, Docquier PL, Schubert T, GalantC, Malghem J. Diagnosis failure led to the recurrence of an intra-articular osteoid osteoma at the talus neck after arthroscopic excision. Foot Ankle Surg 2014;20:e40-2. [Google Scholar]
- 11.Looze CA, Capo J, Ryan MK, Begly JP, Chapman C, Swanson D, et al. Evaluation and management of osteochondral lesions of the talus. Cartilage 2017;8:19-30. [Google Scholar]
- 12.Yercan HS, Okcu G, Ozalp T, Osiç U. Arthroscopic removal of the osteoid osteoma on the neck of the talus. Knee Surg Sports Traumatol Arthrosc 2004;12:246-9. [Google Scholar]








