Though a rare complication, angiosarcoma needs to be diagnosed correctly and treated adequately for better outcomes.
Dr. Amar Kamat, Department of Orthopedic Oncology, HCG Hospital, Bengaluru, Karnataka, India. E-mail: dramar.kamat@gmail.com
Introduction: Cutaneous angiosarcoma is an uncommon aggressive tumor known to arise in chronic lymphedema of various etiologies with post mastectomy lymphedema being the most common cause also known as Stewart–Treves syndrome. Chronic filarial lymphedema is the most uncommon etiology for development of angiosarcoma.
Case Report: We describe two cases of angiosarcoma developing in a setting of long-standing filarial lymphedema. The patient presented with the same clinical features of rapidly progressing nodules.
Conclusion: With India harboring most of the filarial load, this scenario should be kept in mind by clinicians for early diagnosis and treatment. Angiosarcoma is a rapidly progressing tumor and is fatal; hence, an idea about its diagnosis is of utmost importance.
Keywords: Stewart–Treves syndrome, angiosarcoma, chronic filarial lymphedema.
India once being an endemic country for lymphatic filariasis has many known complications. Angiosarcoma is a rare but significant complication that has received little attention in the literature. We present two examples of the same.
A 61-year-old female presented with an enlarged and edematous right leg (Fig. 1). The patient reported a history of lymphatic filariasis diagnosed 15 years previously. She complained of rapidly increasing skin nodules over her leg progressing upward for 6 months. Her prior treatment consisted of antibiotics with variable response. On examination, there was extensive skin thickening with multiple nodules and an ulcerating wound over the anterior surface of the leg measuring approximately 6 × 3 × 3 cm. 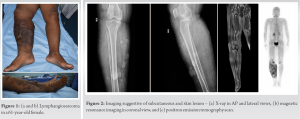 The superior most nodule was at the superior border of the patella. Magnetic resonance imaging (MRI) (Fig. 2) showed extensive skin thickening and subcutaneous edema, with normal skeletal muscle and bone. A positron emission tomography (PET) was performed, showing only local disease with no metastasis. An fine-needle aspiration cytology was suggestive of high-grade spindle cell sarcoma.
The superior most nodule was at the superior border of the patella. Magnetic resonance imaging (MRI) (Fig. 2) showed extensive skin thickening and subcutaneous edema, with normal skeletal muscle and bone. A positron emission tomography (PET) was performed, showing only local disease with no metastasis. An fine-needle aspiration cytology was suggestive of high-grade spindle cell sarcoma.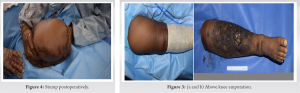 Following pre-operative evaluation, it was noted that all hematological parameters were normal and serological parameters including HBsAg, HCV, and HIV I and II which were negative. The patient was planned for an above-knee amputation (Figs. 3 and 4), maintaining a 2 cm margin for the same. Intraoperative frozen section was performed, showing clear margins.
Following pre-operative evaluation, it was noted that all hematological parameters were normal and serological parameters including HBsAg, HCV, and HIV I and II which were negative. The patient was planned for an above-knee amputation (Figs. 3 and 4), maintaining a 2 cm margin for the same. Intraoperative frozen section was performed, showing clear margins.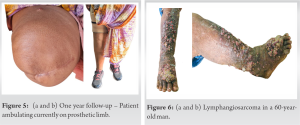 The post-operative histopathology confirmed the diagnosis of angiosarcoma spindle-shaped solid type expressing CD31 and CD34. Subsequently, she received adjuvant chemotherapy regimen with doxorubicin-paclitaxel-based therapy. Prosthetic fitting was done at week 6 and the patient was made to weight bear with support for another 6 weeks. At one-year follow-up, an interval PET scan confirmed the disease-free status of the patient. The stump had healed well and consolidated. The patient is currently walking on the prosthesis without support (Fig. 5).
The post-operative histopathology confirmed the diagnosis of angiosarcoma spindle-shaped solid type expressing CD31 and CD34. Subsequently, she received adjuvant chemotherapy regimen with doxorubicin-paclitaxel-based therapy. Prosthetic fitting was done at week 6 and the patient was made to weight bear with support for another 6 weeks. At one-year follow-up, an interval PET scan confirmed the disease-free status of the patient. The stump had healed well and consolidated. The patient is currently walking on the prosthesis without support (Fig. 5).
A 60-year-old man presented to the hospital with multiple ulcerative nodules over his right leg for 1 year (Fig. 6). He was diagnosed with a right filarial limb 20 years previously. He was managed outside with an incision and drainage and antibiotics 6 months before the presentation. Subsequent to this procedure, he reported an increase in the size and the extent of the nodules. On examination, there was extensive skin thickening with multiple nodules and an ulcerating nodule of 10 × 5 × 3cm over the foot with palpable popliteal nodes. MRI (Fig. 7) suggested extensive skin thickening with subcutaneous edema of the right limb, with normal bone and skeletal muscles.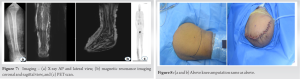 A PET scan demonstrated the popliteal nodes, representing a likely metastasis of the tumor. No systemic spread of the disease was observed in the PET scan. On histopathological evaluation, spindle cell sarcoma was suggested. Following the preoperative workup, an above-knee amputation was planned (Fig. 8), maintaining a 2 cm margin. Postoperative pathology confirmed angiosarcoma, expressing CD31 and CD34 and D2-40 (Fig. 9). The patient received doxorubicin-paclitaxel based adjuvant chemotherapy. At 6 months, patient had blisters on the stump and had to undergo re-fitting of the prosthesis. At 12 month follow-up (Fig. 10), the patient is disease-free as confirmed with PET scan. He is currently ambulant without any complaints.
A PET scan demonstrated the popliteal nodes, representing a likely metastasis of the tumor. No systemic spread of the disease was observed in the PET scan. On histopathological evaluation, spindle cell sarcoma was suggested. Following the preoperative workup, an above-knee amputation was planned (Fig. 8), maintaining a 2 cm margin. Postoperative pathology confirmed angiosarcoma, expressing CD31 and CD34 and D2-40 (Fig. 9). The patient received doxorubicin-paclitaxel based adjuvant chemotherapy. At 6 months, patient had blisters on the stump and had to undergo re-fitting of the prosthesis. At 12 month follow-up (Fig. 10), the patient is disease-free as confirmed with PET scan. He is currently ambulant without any complaints.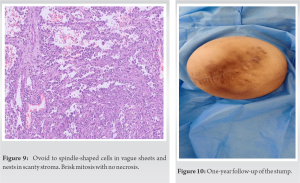
Angiosarcoma is an uncommon tumor arising in chronically edematous limbs. It has been reported to most commonly arise in females undergoing mastectomy with removal of axillary nodes (Stewart–Treves Syndrome) [1, 2]. Stewart and Treves were the first to describe a case of Angiosarcoma arising from chronic post-mastectomy lymphedema [1]. It can also occur in idiopathic, congenital, and post-operative chronic lymphedema [2, 3, 4, 5, 6]. The prognosis of this tumor is very poor, with a 5- year survival rate of between 12 and 33% [7]. Lymphatic filariasis is a neglected tropical disease and is caused by parasites, known as nematodes (roundworms). They can be: Wuchereria Bancrofti (most common), Brugia Malayi, and Brugia Timori. Adult worms harbor in the lymphatic system for almost 6–8 years producing millions of microfilariae. These microfilariae are ingested by the mosquito (mainly Culex and Anopheles) by ingesting blood of the infected host. The microfilariae mature into infected larvae in the mosquito. When these mosquitoes bite people, the larvae are deposited into the skin and proceed to the lymphatic vessels, maintaining the cycle. Lymphatic filariasis presents as asymptomatic, acute, or chronic stages. Asymptomatic filariasis may still be silently causing harm to the lymphatic system and kidneys. Acute filariasis may cause inflammation of the skin, lymphatic system, and nodes. Chronic lesions may present as lymphedema of limbs, elephantiasis, and/or hydrocele. Filariasis causes a massive social stigma. There is no clear consensus in the current literature regarding the malignant transformation of chronic filarial lymphoedema and it is optimum management. El Toraei [8] did not identify a single case of angiosarcoma in a large number of cases of filarial lymphedema. Many authors claim that they have not seen this tumor arising in patients with filarial lymphedema. Hence, this tumor occurring in a filarial limb is a rare entity [9, 10]. Devi and Bahuleyan [11] were the first to describe angiosarcoma in filariasis. They suggested chronic lymphatic stasis as a probable cause of tumor development. The patient had no systemic metastasis but died shortly after diagnosis due to unknown causes, before initiation of treatment. Sordillo et al. [12] described a patient with angiosarcoma in a 20-year-old filarial right lower limb. He was operated on for above knee amputation and radical groin dissection. No adjuvant therapy was given as the nodes were free of disease. The patient developed lung metastasis 8 years after the treatment. Muller et al. [13] demonstrated angiosarcoma in a 15-year-old filarial limb. The patient underwent a hind-quarter amputation. The patient was free from disease at 2-year follow-up. Krishnamoorty et al. [14] described a patient with angiosarcoma in a 33-year chronic filarial lymphedema. The patient underwent an above-knee amputation, but died at 5 months duration with lung metastasis. We have reported this case due to the rarity of such a phenomena and to highlight the rare complication of chronic filarial lymphedema. The physician should be made aware of this complication and how a radical and aggressive approach in a planned manner is vital to save the life of the patient. Although the number of patients with newly diagnosed filariasis has significantly decreased in the last decade due to various initiatives [15], there are still many patients with a filarial limb in the community with a potential to develop this dreaded complication. There seems to be an established role in getting a pre-operative PET scan done, as it helps the clinical to know whether it is a metastatic presentation or not. This may guide the subsequent use of adjuvant chemotherapy. In our study, popliteal nodes were positive for one patient suggestive of metastasis and the other patient had no metastasis. The surgical aspect for such a presentation needs attention. The limb should be wrapped preoperatively to prevent soiling of the surroundings and also of the operation theater. Limb elevation and steroids are started for the patient to decrease the lymphedema as much as possible as it minimizes wound complications. Antibiotics should be started a day before the surgery.
Chart 1: The Yellow Ribbon (TYR) protocol for management of leg ulcers before surgery
Day 1-3: Start steroids and maintain limb elevation
Day 4: Start antibiotics and wrap the limb
Day 5: Surgery
Angiosarcoma setting in a scenario of chronic filarial lymphedema is a rare but significant complication with only a few cases reported world-wide. With India having harbored most endemic areas for lymphatic filariasis, close follow-up of these patients along with awareness of this phenomenon is crucial in early diagnosis and treatment. The study of adjuvant chemotherapy shall be done to judge the long-term survival in such cases.
This case report strives to achieve early diagnosis and treatment in a potentially curable case.
References
- 1.Stewart FW, Treves N. Lymphangiosarcoma in post-mastectomy lymphedema. Cancer 1948;1:64-81. [Google Scholar]
- 2.Hajdu SI. Pathology of Soft Tissue Tumors. Philadelphia: Lea and Febiger; 1979. [Google Scholar]
- 3.Mackenzie DH. Lymphangiosarcoma arising in chronic congenital and idiopathic lymphedema. J Clin Parhol 1971;24:524-9. [Google Scholar]
- 4.Memck TA , Erlandson RA, Hajdu SI. Lymphangiosarcoma of a congenitally lymphedematous arm. Arch Pathol 1971;21:365-71. [Google Scholar]
- 5.Burnett WO, Hardy JO, Hendrix JH. Lymphangiosarcoma following postmastectomy lymphedema. Ann Surg 1969;169:960-8. [Google Scholar]
- 6.Calnan J, Cowdell RH. Lymphangio-endothelioma of the anterior abdominal wall: Report of a case. Br J Surg 1959;46:375-9. [Google Scholar]
- 7.Fletcher CD. Diagnostic Histopathology of Tumors. 3rd ed., vol. 1. London, United Kingdom: Elsevier Churchill Livingstone; 2007. p. 63-7. [Google Scholar]
- 8.El-Toraei I. Filarial lymphedema. Angiology 1966;17:644-60. [Google Scholar]
- 9.Enzinger FM, Weiss SW. Soft Tissue Tumors. St. Louis: CV Mosby; 1983. [Google Scholar]
- 10.Scott RB, Nydick I, Conway H. Lymphangiosarcoma arising in lymphedema. Am J Med 1960;28:1008-12. [Google Scholar]
- 11.Devi L, Bahuleyan CK. Lymphangiosarcoma of the lower extremity associated with chronic lymphedema of filarial origin. Indian J Cancer 1977;14:176-8. [Google Scholar]
- 12.Sordillo EM, Sordillo PP, Hajdu SI, Good RA. Lymphangiosarcoma after filarial infection. J Dermatol Surg Oncol 1981;7:235-9. [Google Scholar]
- 13.Muller R, Hadju SI, Brennan MF. Lymphangiosarcoma associated with chronic filarial lymphedema. Cancer 1987;59:179-83. [Google Scholar]
- 14.Krishnamoorthy N, Viswanathan S, Rekhi B, Jambhekar NA. Lymphangiosarcoma arising after 33 years within a background of chronic filariasis: A case report with review of literature. J Cutan Pathol 2012;39:52-5. [Google Scholar]
- 15.Das PK, Ramaiah KD, Augustin DJ, Kumar A. Towards elimination of lymphatic filariasis in India. Trends Parasitol 2001;17:457-60. [Google Scholar]