Pathological fractures secondary to UBC in pediatric patients with ASD are best treated with open curettage, allograft impaction, and definitive fixation using locking compression plate, even if the fracture is present in a non-weight bearing bone.
Dr. Amyn M Rajani, Department of Orthopaedics, OAKS Clinic, Mumbai, Maharashtra, India. E-mail: dramrajani@gmail.com
Introduction: Pathological fractures in pediatric age group are most commonly secondary to bone tumors. Management of such cases in patients with autism spectrum disorder (ASD) is complicated by the prevalence of low bone mineral density (BMD) in these patients.
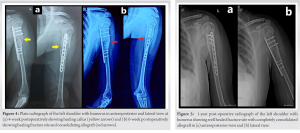
Case Report: Through this case, we report a 13-year-old male diagnosed with autism spectrum disease, who was brought by his parents with a history of trivial trauma and gross deformity of the left humerus. On plain radiography, a displaced fracture in the foreground of a lytic, cystic lesion was noted which on magnetic resonance imaging was confirmed to be metadiaphyseal unicameral bone cyst. The patient underwent extensive curettage, allograft impaction, and definitive fixation by a locking compression plate. Following a relatively extended period of immobilization, he was started on range of motion exercises followed by strengthening. He was able to return to his pre-operative activity levels at 14 weeks postoperatively. At 1-year postoperatively, the patient achieved excellent clinical and radiological outcomes, without any signs of failure, complications, or signs of recurrence.
Conclusion: Management of pathological fractures in pediatric patients with ASD can be challenging due to the associated low BMD and potential non-compliance from the patient’s end. Such cases are best treated with open curettage, allograft impaction, and definitive fixation by locking compression plate, even if present in a non-weight bearing bone.
Keywords: Pathological fracture, humerus, bone cyst, management, plating, graft, curettage, autism.
Pathological fractures in the pediatric age group are suspected following a history of trivial trauma, uncommon anatomical site, or abnormal changes in the bone intensity at the fracture site on radiological imaging [1]. In these patients, pathological fractures are most common secondary to intrinsic pathologies that negatively alter the bone mineral density (BMD) or normal trabecular meshwork of the growing bone such as tumors (benign or metastatic), infection, and genetic diseases such as osteogenesis imperfecta [1]. The site of the disease process and subsequently the net vector of loading force concentrated at that site precedes such fractures [2]. The risk of such factors, both biological and mechanical, are aggravated in genetic such as autism spectrum disorder (ASD). It has been well documented in the literature that ASD is associated with adversely affected BMD of growing bones, especially in males of peripubertal age group [3]. However, the fracture rates in ASD patients has been poorly established, with some studies reporting a negative correlation due to decreased participation in sporting activities [4]. Similarly, the treatment options for pathological fractures in such patients are not well documented in orthopedic literature. With this case report, we document open curettage and allograft impaction along with plate osteosynthesis as an effective treatment modality for pathological fractures in children with ASD.
A 13-year-old, right-hand dominant male, was brought to our clinic by his parents with a history of fall from bed while sitting. They presented to the clinic with complaints of pain and deformity over the left arm and inability to move the left upper limb due to pain. The patient was a previously diagnosed case of ASD, on regular medications in the form of anticonvulsants. On examination, a gross deformity was noted over the proximal third of the left arm, along with swelling, tenderness, and crepitus. The distal pulsations were normal and there was no neurological deficit.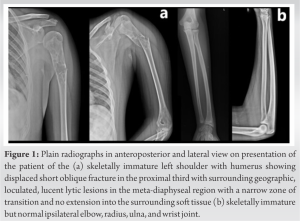
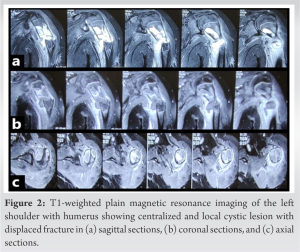
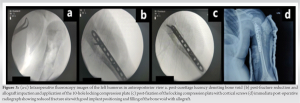
Fractures following trivial trauma in the pediatric age group are rare and most commonly attributable to bone tumors, infection, or genetic bone disorders [5]. Out of these, primary bone tumors form the majority of the cases. Unicameral bone cyst accounts for nearly 3% of all benign bone tumors in the population of this age group, and three in every four patients with UBC present with a pathological fracture [6, 7]. The most common site of pathological fractures secondary to UBC in pediatric age group is the proximal humerus (as was the case in our report) followed by the proximal femur [7]. Various treatment modalities have been described depending on fracture morphology, ranging from conservative management by splinting and immobilization of stable, minimally displaced fractures for 4–6 weeks, to surgery for unstable fractures [7]. Our case was confounded by the diagnosis of ASD in our patient, along with the use of anticonvulsants, both of which are associated with decreased BMD and consequently reduced bone strength [3, 8]. A negative correlation between ASD and the risk of fractures has been documented by a few authors; however, the implications of compromised bone strength on fracture healing in such patients have not been studied in detail [4]. Our patient typically presented with a gross deformity over his left upper arm, and an inability to move the affected limb. After a thorough history and clinical assessment, a plain radiograph in two orthogonal planes was ordered, as is the norm [5]. We suspected a pathological fracture based on the history given by the parents of the patient, which was confirmed on the radiograph which showed features typical of a UBC. An MRI scan supplemented the diagnosis. Due to the patient profile and fracture being unstable and displaced, conservative management was not opted for. Although numerous other management protocols have been elucidated in the literature, such as fixation of the fracture followed by decompression by mechanical disruption of cyst wall, intralesional injections of steroids, bone marrow aspirate, demineralized bone matrix, and bone substitutes [9], or relatively newer percutaneous techniques such as percutaneous intramedullary decompression, curettage, and grafting with calcium sulfate pellets by Dormans et al. [10], or minimally invasive curettage, ethanol cauterization, disruption of the cystic boundary, insertion of a synthetic calcium sulfate bone-graft substitute, and placement of a cannulated screw by Hou et al. [11], or different combinations of autologous bone marrow injection (21–23% success rate), methylprednisolone injection (41–42% success rate), and percutaneous curettage by some authors [12, 13], we chose to undertake thorough curettage under vision and fluoroscopy guidance followed by allograft impaction and fixation by plate osteosynthesis. This choice of an invasive procedure was made based on drawbacks highlighted by other methods such as persistence of UBC in up to 50% of cases managed conservatively [7], recurrence or persistence rates of up to 30% with percutaneous techniques, and higher incidences of recurrent pathological fractures and repeat surgical procedures following the use of these techniques [11, 12], The backdrop of autism in our patient meant chances of non-compliance was high. In addition, we wanted to avoid subjecting the patient to a repeat procedure. Hence, even though the fracture was in a non-weight bearing bone, a decision to do open curettage with definitive fixation using locking compression plate with cortical locking screws was taken. The finding of paper-thin cortices and soft bone due to reduced BMD was consistent with the literature [3, 4]. Allograft impaction was done with the purpose of increasing chances for union by providing a scaffolding for osteogenesis and osteoinduction as well as providing structural support till the healing is achieved. The operated limb was kept immobilized in a U-slab and arm pouch until radiological evidence of union. We observed progressive healing of the fracture site at 4 weeks and 6 weeks, following which passive mobilization of the limb was started. As assessment in terms of subjective patient, related outcome measures was not possible, objective measurements in the form of range of motion and strength were done. Due to the ASD which affected patient compliance during physical therapy, rehabilitation was noticed to be delayed with a complete range of motion being achieved by 12 weeks postoperatively (Flexion:180°; Extension:60°; Abduction:180°; External rotation: 90°; Internal rotation: 70°, as measured by a goniometer), and regaining of strength same as the contralateral, unaffected side by 14 weeks postoperatively. 1- year follow-up showed excellent healing of the fracture site with complete consolidation of the allograft and no recurrence of the tumor.
Patients with ASD who present as a case of pathological fracture of the proximal humerus secondary to simple bone cyst are best treated aggressively with extensive open curettage, compact cancellous allograft impaction, and definitive fixation with locking compression plate. We suggest immobilization of the operated limb till radiological evidence of union followed by physical therapy to regain range of motion and strength.
Pathological fractures secondary to UBC in pediatric patients with ASD are best treated with open curettage, allograft impaction, and definitive fixation using locking compression plate, even if the fracture is present in a non-weight bearing bone.
References
- 1.Dormans JP, Pill SG. Fractures through bone cysts: Unicameral bone cysts, aneurysmal bone cysts, fibrous cortical defects, and nonossifying fibromas. Instr Course Lect 2002;51:457-67. [Google Scholar]
- 2.Snyder BD, Hauser-Kara DA, Hipp JA, Zurakowski D, Hecht AC, Gebhardt MC. Predicting fracture through benign skeletal lesions with quantitative computed tomography. J Bone Joint Surg Am 2006;88:55-70. [Google Scholar]
- 3.Neumeyer AM, Gates A, Ferrone C, Lee H, Misra M. Bone density in peripubertal boys with autism spectrum disorders. J Autism Dev Disord 2013;43:1623-9. [Google Scholar]
- 4.Neumeyer AM, O’Rourke JA, Massa A, Lee H, Lawson EA, McDougle CJ, et al. Brief report: Bone fractures in children and adults with autism spectrum disorders. J Autism Dev Disord 2015;45:881-7. [Google Scholar]
- 5.De Mattos CB, Binitie O, Dormans JP. Pathological fractures in children. Bone Joint Res 2012;1:272-80. [Google Scholar]
- 6.Wilkins RM. Unicameral bone cysts. J Am Acad Orthop Surg 2000;8:217-24. [Google Scholar]
- 7.Ortiz EJ, Isler MH, Navia JE, Canosa R. Pathologic fractures in children. Clin Orthop Relat Res 2005;432:116-26. [Google Scholar]
- 8.Zhang Y, Zheng YX, Zhu JM, Zhang JM, Zheng Z. Effects of antiepileptic drugs on bone mineral density and bone metabolism in children: A meta-analysis. J Zhejiang Univ Sci B 2015;16:611-21. [Google Scholar]
- 9.Donaldson S, Wright JG. Recent developments in treatment for simple bone cysts. Curr Opin Pediatr 2011;23:73-7. [Google Scholar]
- 10.Dormans JP, Sankar WN, Moroz L, Erol B. Percutaneous intramedullary decompression, curettage, and grafting with medical-grade calcium sulfate pellets for unicameral bone cysts in children: A new minimally invasive technique. J Pediatr Orthop 2005;25:804-11. [Google Scholar]
- 11.Hou HY, Wu K, Wang CT, Chang SM, Lin WH, Yang RS. Treatment of unicameral bone cyst: Surgical technique. J Bone Joint Surg Am 2011;93:92-9. [Google Scholar]
- 12.Canavese F, Wright JG, Cole WG, Hopyan S. Unicameral bone cysts: Comparison of percutaneous curettage, steroid, and autologous bone marrow injections. J Pediatr Orthop 2011;31:50-5. [Google Scholar]
- 13.Wright JG, Yandow S, Donaldson S, Marley L. A randomized clinical trial comparing intralesional bone marrow and steroid injections for simple bone cysts. J Bone Joint Surg Am 2008;90:722-30. [Google Scholar]