A high suspicion for hydatid infestation in bone pathologies could help in diagnosing the disease at the earliest.
Dr. Sumant Chacko Verghese, Department of Orthopaedics, KMCH Institute of Health Sciences and Research, Coimbatore, Tamil Nadu, India. E-mail: sumant.chacko810@gmail.com
Introduction: Hydatid disease of the bone is a parasitic infestation in the form of cystic echinococcosis by a tapeworm echinococcus granulosus. Its manifestation in the bone is relatively low and has the ability to mimic other skeletal pathologies.
Case Report: We came across a 30-year-old male farmer with complaints of sero-purulent discharge from a sinus tract wound in the axilla for the past 3 years. He had been previously evaluated elsewhere with blood investigations, pus culture/sensitivity tests, MRI, and CT scans. Blood reports and culture/sensitivity tests were inconclusive and imaging tests were suggestive of a sinus tract originating from the right scapula. He was incorrectly diagnosed as a case of Tuberculosis of the Scapula and started on anti-tubercular medications for 9 months which was ineffective. To confirm the diagnosis, a biopsy was taken from the scapular lesion through a posterior approach. Histological tests revealed a cystic lesion composed of trilaminar membrane consisting of dead and degenerating scolices consistent with “Hydatid Cyst of Bone.”
Conclusion: Hydatid disease of the bone has an inconsistent clinical picture which makes diagnosing this rare disease even more difficult. A high suspicion for hydatid infestation in bone pathologies could help in diagnosing the disease at the earliest.
Keywords: Hydatid disease, echinococcus granulosis, scapula.
Hydatid disease of the bone is a parasitic infestation by a tapeworm of the genus Echinococcus [1]. Of the known species, the most commonly seen affecting humans are E. granulosus in the form of cystic echinococcosis [2]. Theoretically, echinococcosis can involve any organ. The liver is the most commonly involved organ, followed by the lungs and these two organs account for approximately 90% of the cases [3]. Its manifestation within the bone is relatively low (~4%) and is most commonly seen in the spine (50–60%) [4]. Osseous hydatidosis can remain dormant for as long as 40 years. Since hydatid disease of the bone is often asymptomatic for such a long duration, it is usually detected at an advanced stage when radiological lesions are already extensive [5]. We present a case of late presentation of hydatid disease of the scapula, which was misdiagnosed and mismanaged for over 3 years, due to its ability to mimic other skeletal pathologies.
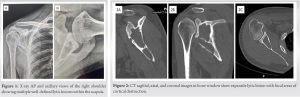 A 30-year-old male farmer hailing from a small village in Rajasthan, India presented to the out-patient department with complaints of intermittent seropurulent discharge from a sinus tract wound on the posteromedial aspect of the proximal right arm adjacent to the base of the axilla. The patient was apparently alright 3 years ago when he sustained injury to the right shoulder axillary region, where he was struck with a leather ball while playing cricket. He was evaluated at a local hospital with X-rays which did not show any acute bony injury and was informed that there might be a localized soft tissue injury. He was treated with an arm-sling, ice-packs, and pain-relief medications. Initially, the patient responded well and had symptomatic pain relief; however, the swelling still persisted. Approximately a month after the injury, he developed a discharging sinus from the posteromedial aspect of the proximal right arm just adjacent to the base of the axilla. This was associated with severe pain in the right shoulder and restriction of movements. The patient was referred to a tertiary health-care center, where he was, further, evaluated to determine the source of the discharging sinus. The patient did not possess any of these tests final reports which were done at this tertiary center. As per the patient, he first underwent an MRI which revealed an infectious origin of the discharging sinus originating from the right scapula. Next a swab-stick and a tissue sampl e from the sinus tract were sent for culture/sensitivity and biopsy, respectively. However, the final growth culture report and the biopsy report were inconclusive, as the tests were negative. The patient was diagnosed (most likely by a method of exclusion) as a case of “Right Scapula Tuberculosis” and was started on anti-tubercular medications for a duration of 9 months. The patient responded well to the anti-tubercular medications and the sinus tract healed within a few months. The patient had complete relief of pain and his right shoulder range of movements was back to normal. The patient was doing well for approximately 2 months after he stopped the anti-tubercular medications, when he again noticed seropurulent discharge from the sinus tract. However, this time the pain was relatively less in intensity with no restriction in movements of the affected shoulder. The patient only complaint was an intermittent on-off discharge from the sinus tract, which was usually for 2–3 days every few weeks. The patient presented to us at this stage of his disease. On taking a further detailed history, the patient informed us that he has pets and farm animals at his hometown – dogs, sheep, and goats. On examination, there was a sinus tract in the posteromedial aspect of the proximal right arm just adjacent to the base of the axilla which, on presentation, was dry. The right shoulder movements were within normal range and not associated with any pain. The only complaint the patient had on presentation was the intermittent seropurulent discharge from the sinus tract which was affecting his daily living condition. The patient was first evaluated with X-rays of the right shoulder which showed multiple well-defined lytic lesions within the body of scapula, as shown in Fig. 1. Blood investigations demonstrated a slightly raised ESR (13 mm/h) with a negative CRP (5.9 mg/L), a negative Mantoux test, and normal WBC counts (4,800/mm3). Liver and renal function tests were also within normal limits. The CT scan (Fig. 2) revealed expansile lytic lesions involving the lateral aspect of the body of scapula, extending into the coracoid process and up to the base of the spine with multi-focal areas of destruction along the lateral border of scapula and coracoid process. On the MRI scan (Fig. 3), a sinus tract was noted with enhancing granulation tissue from the lateral border of the scapula at the infra-glenoid region, which extended inferiorly along the tendon of the long head of the triceps muscle and opened into the skin surface at the posteromedial aspect of upper arm. A decision was made to obtain a direct biopsy from the lesion in the scapula to reach a final diagnosis. The patient was positioned in lateral position (Fig. 4a), and the scapula was exposed via posterior approach. A vertical skin incision of size 10cm was made starting at the tip of the posterolateral corner of the acromion toward the scapular angle, parallel to the lateral border of the scapula. The deltoid muscle was dissected and retracted superiorly. Inter-muscular plane interval was developed between the infraspinatus and the teres minor muscle to expose the axillary and lateral border of the scapula (Fig. 4b).
A 30-year-old male farmer hailing from a small village in Rajasthan, India presented to the out-patient department with complaints of intermittent seropurulent discharge from a sinus tract wound on the posteromedial aspect of the proximal right arm adjacent to the base of the axilla. The patient was apparently alright 3 years ago when he sustained injury to the right shoulder axillary region, where he was struck with a leather ball while playing cricket. He was evaluated at a local hospital with X-rays which did not show any acute bony injury and was informed that there might be a localized soft tissue injury. He was treated with an arm-sling, ice-packs, and pain-relief medications. Initially, the patient responded well and had symptomatic pain relief; however, the swelling still persisted. Approximately a month after the injury, he developed a discharging sinus from the posteromedial aspect of the proximal right arm just adjacent to the base of the axilla. This was associated with severe pain in the right shoulder and restriction of movements. The patient was referred to a tertiary health-care center, where he was, further, evaluated to determine the source of the discharging sinus. The patient did not possess any of these tests final reports which were done at this tertiary center. As per the patient, he first underwent an MRI which revealed an infectious origin of the discharging sinus originating from the right scapula. Next a swab-stick and a tissue sampl e from the sinus tract were sent for culture/sensitivity and biopsy, respectively. However, the final growth culture report and the biopsy report were inconclusive, as the tests were negative. The patient was diagnosed (most likely by a method of exclusion) as a case of “Right Scapula Tuberculosis” and was started on anti-tubercular medications for a duration of 9 months. The patient responded well to the anti-tubercular medications and the sinus tract healed within a few months. The patient had complete relief of pain and his right shoulder range of movements was back to normal. The patient was doing well for approximately 2 months after he stopped the anti-tubercular medications, when he again noticed seropurulent discharge from the sinus tract. However, this time the pain was relatively less in intensity with no restriction in movements of the affected shoulder. The patient only complaint was an intermittent on-off discharge from the sinus tract, which was usually for 2–3 days every few weeks. The patient presented to us at this stage of his disease. On taking a further detailed history, the patient informed us that he has pets and farm animals at his hometown – dogs, sheep, and goats. On examination, there was a sinus tract in the posteromedial aspect of the proximal right arm just adjacent to the base of the axilla which, on presentation, was dry. The right shoulder movements were within normal range and not associated with any pain. The only complaint the patient had on presentation was the intermittent seropurulent discharge from the sinus tract which was affecting his daily living condition. The patient was first evaluated with X-rays of the right shoulder which showed multiple well-defined lytic lesions within the body of scapula, as shown in Fig. 1. Blood investigations demonstrated a slightly raised ESR (13 mm/h) with a negative CRP (5.9 mg/L), a negative Mantoux test, and normal WBC counts (4,800/mm3). Liver and renal function tests were also within normal limits. The CT scan (Fig. 2) revealed expansile lytic lesions involving the lateral aspect of the body of scapula, extending into the coracoid process and up to the base of the spine with multi-focal areas of destruction along the lateral border of scapula and coracoid process. On the MRI scan (Fig. 3), a sinus tract was noted with enhancing granulation tissue from the lateral border of the scapula at the infra-glenoid region, which extended inferiorly along the tendon of the long head of the triceps muscle and opened into the skin surface at the posteromedial aspect of upper arm. A decision was made to obtain a direct biopsy from the lesion in the scapula to reach a final diagnosis. The patient was positioned in lateral position (Fig. 4a), and the scapula was exposed via posterior approach. A vertical skin incision of size 10cm was made starting at the tip of the posterolateral corner of the acromion toward the scapular angle, parallel to the lateral border of the scapula. The deltoid muscle was dissected and retracted superiorly. Inter-muscular plane interval was developed between the infraspinatus and the teres minor muscle to expose the axillary and lateral border of the scapula (Fig. 4b). 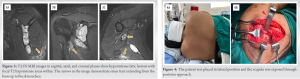 The lesion was identified and a small bone window of size 1 × 1 cm was initially made to extract the tissue from within as depicted in Fig. 5a and b. However, the posterior wall of the scapula at the site of the lesion was extremely thin and brittle leading to an irregular bony window (Fig. 5c). Gray-white flaky soft-tissue mass was curetted out of these lesions, as shown in Fig. 5d. The tissue sample and bone were sent for culture/sensitivity tests and biopsy. Wound was closed in layers over a drain. Postoperatively, the right shoulder was immobilized in an arm sling. Suture line dressings were done in the ward which was clean and the drain was removed on the 3rd post-operative day. Tissue culture and sensitivity tests were negative (Final report; No Growth). However, histological examination showed a cystic lesion composed of trilaminar membrane consisting of dead and degenerating scolices (Fig. 6) consistent with “Hydatid Cyst of Bone.” General medicine team and infection diseases team were consulted and the patient was started on tablet Albendazole 10 mg/kg daily. The abdomen and thorax were screened with a CT scan to determine a spread of the parasite to the liver or the lungs. The CT scan showed no spread to either of these organs. The patient was counseled regarding the severity of the diagnosis and the complications of the disease. The patient was planned for total scapulectomy with scapula-humeral reconstruction. However, the patient was not willing for the procedure and requested that he wanted to go back to his hometown to make a decision regarding the same. The patient was lost to follow-up and did not return for further management.
The lesion was identified and a small bone window of size 1 × 1 cm was initially made to extract the tissue from within as depicted in Fig. 5a and b. However, the posterior wall of the scapula at the site of the lesion was extremely thin and brittle leading to an irregular bony window (Fig. 5c). Gray-white flaky soft-tissue mass was curetted out of these lesions, as shown in Fig. 5d. The tissue sample and bone were sent for culture/sensitivity tests and biopsy. Wound was closed in layers over a drain. Postoperatively, the right shoulder was immobilized in an arm sling. Suture line dressings were done in the ward which was clean and the drain was removed on the 3rd post-operative day. Tissue culture and sensitivity tests were negative (Final report; No Growth). However, histological examination showed a cystic lesion composed of trilaminar membrane consisting of dead and degenerating scolices (Fig. 6) consistent with “Hydatid Cyst of Bone.” General medicine team and infection diseases team were consulted and the patient was started on tablet Albendazole 10 mg/kg daily. The abdomen and thorax were screened with a CT scan to determine a spread of the parasite to the liver or the lungs. The CT scan showed no spread to either of these organs. The patient was counseled regarding the severity of the diagnosis and the complications of the disease. The patient was planned for total scapulectomy with scapula-humeral reconstruction. However, the patient was not willing for the procedure and requested that he wanted to go back to his hometown to make a decision regarding the same. The patient was lost to follow-up and did not return for further management.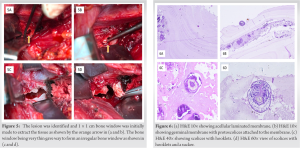
Hydatid disease of the bone is very rare and constitutes 1–5.4% of all of the cases which can mimic a soft tissue tumor [6]. Surgical intervention along with anti-helminthic chemotherapy is the therapeutic treatment of choice [5]. Chemotherapy using mebendazole or albendazole as only treatment is not adequate in most cases. However, it can be used as neoadjuvant therapy to shrink the cyst load before surgery and/or as adjuvant therapy to decrease the recurrence risk [5]. Radiotherapy is also an efficacious adjunct to the surgery, particularly in those with contraindications to medical treatment [7]. Chari PR reported a similar case of hydatid bone disease of the scapula with involvement of the upper-third of the ipsilateral humerus [8]. The patient was advised fore-quarter amputation but refused for the same and was surgically managed with a two-staged limb salvage procedure. In the first stage, en bloc excision of the scapula, upper half of humerus, and lateral end of clavicle were done. In the second stage, proximal humerus was reconstructed with the upper three-fourths of the fibula. The patient regained 30–40° active painless movements of the shoulder and reasonable stability with no recurrence of the disease. Inayat et al. reported a case of pelvic bone hydatidosis which was managed with anti-helminthic chemotherapy followed by surgery [9]. The patient was started on oral albendazole for 3 months which showed relative regression of the disease. The patient then underwent en bloc excision of the hydatid cyst with curettage and the gap was filled with bone cement. Ciftdemir et al. reported a case of bone hydatidosis of the femoral shaft which was managed with surgical debridement and excision of the cyst [10]. However, 10 days after discharge, the patient presented with a pathological fracture of the shaft of femur which was treated with a custom made intra-medullary inter-locking nail. To the best of our knowledge, there is no other case in the literature which describes an isolated hydatid bone disease of the scapula. Bone hydatid disease should be considered as a progressive tumor and managed accordingly to obtain the best possible functional outcome. The patient in our case presentation was screened to locate spread to other organs. Once it was confirmed that the disease was confined to the scapula, the patient was planned for total Scapulectomy with scapula-humeral reconstruction.
Hydatid infestation of bone has an inconsistent clinical picture which makes diagnosing this rare disease even more difficult. It may even lead to incorrectly diagnosing the disease as other infective pathologies and neoplasia. A high suspicion for hydatid infestation in bone pathologies could help in diagnosing the disease at the earliest. The fundamental step to successfully managing the disease is prompt recognition of the nature of the lesion and an early recourse to surgery.
Primary hydatid disease of the bone is a rare entity that is often misdiagnosed during the preliminary assessment (clinical and radiological) due to its non-specific characteristics. It is consequential to remember this entity in the differential diagnosis when evaluating bony pathologies.
References
- 1.Ravis E, Theron A, Lecomte B, Gariboldi V. Pulmonary cyst embolism: A rare complication of hydatidosis. Eur J Cardiothorac Surg 2018;53:286-7. [Google Scholar]
- 2.Wang N, Zhong X, Song X, Gu X, Lai W, Xie Y, et al. Molecular and biochemical characterization of calmodulin from Echinococcus granulosus. Parasit Vectors 2017;10:597. [Google Scholar]
- 3.Kayal A, Hussain A. A comprehensive prospective clinical study of hydatid disease. ISRN Gastroenterol 2014;2014:514757. [Google Scholar]
- 4.Herrera A, Martínez AA, Rodríguez J. Spinal hydatidosis. Spine 2005;30:2439-44. [Google Scholar]
- 5.Zlitni M, Ezzaouia K, Lebib H, Karray M, Kooli M, Mestiri M. Hydatid cyst of bone: Diagnosis and treatment. World J Surg 2001;25:75-82. [Google Scholar]
- 6.Pirhan Y, Necmi KU. Bone hydatid cyst disease. Dicle Tıp Dergisi 2017;44:401-4. [Google Scholar]
- 7.Inayat F, Azam S, Baig AS, Nawaz G, Ullah W. Presentation patterns, diagnostic modalities, management strategies, and clinical outcomes in patients with hydatid disease of the pelvic bone: A comparative review of 31 cases. Cureus 2019;11:e4178. [Google Scholar]
- 8.Chari PR. Hydatid disease of scapula and upper third of humerus treated by en bloc excision and fibular bone grafting. Indian J Orthop 2007;41:241-3. [Google Scholar]
- 9.Inayat F, Rana RE, Azam S, Ahmad R, Ahmad S. Pelvic bone hydatidosis: A dangerous crippling disease. Cureus 2019;11:e4465. [Google Scholar]
- 10.Ciftdemir M, Sezer A, Puyan FO, Copuroglu C, Ozcan M. Hydatid disease of the femur with an extraosseous extent due to a former biopsy complicated by a pathological fracture. Case Rep Orthop 2012;2012:169545. [Google Scholar]











