Peek material is not free from tissue reaction and inflammation in such setting is not always infection.
Dr. Bishnu Prasad Patro, Department of Orthopaedics, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: bishnucolours@gmail.com
Introduction: Interferential screws and anchors have played a major role in fixation of soft tissue to bony tunnel. With advent of time, there developed metal anchors, biodegradable anchors, bioinert anchors, etc. Biodegradable anchors had complications such as reactive synovitis, cyst formation, soft-tissue inflammation, and local osteolysis. Polyether ether ketone (PEEK) which was biologically inert and radiolucent was introduced to overcome the disadvantages of anchors. We present a case of non-suppurative tissue reaction to PEEK anchor following rotator cuff repair.
Case Report: A 58-year-old male patient presented to us with signs of rotator cuff tear following injury to his shoulder. Magnetic resonance imaging depicted a massive cuff tear with retraction of cuff. Considering the degree of cuff tear, cuff was repaired with mini open method using two metallic suture anchor and two PEEK knotless bioraptor foot print suture anchor. Surgical wound healing was uneventful and suture was removed on 14th day following surgery. Three weeks following surgery, the patient had pain and rise in temperature over shoulder with raised erythrocyte sedimentation rate and C-reactive protein which subsided in 7 days with empirical antibiotics. Later, at 3 months, the patient had serous discharge from surgical site, on which exploration revealed pale yellow material vicinity to PEEK anchor. Other than pus cells in smear, discharge was negative to routine culture, grams stain, and cartridge-based nucleic acid amplification test for tuberculosis. Surprisingly, surrounding muscles were healthy, red in color, and contracting to stimulation. Following removal of both the PEEK anchors, local symptoms subsided with improvement in patients shoulder function.
Conclusion: There were cases of tissue reaction to PEEK material in the literature such as osteolysis and cyst formation. In addition, non-suppurative inflammation can occur in response to PEEK material. Awareness about the non-suppurative inflammation property of PEEK material may help future surgeons to manage the condition better than us.
Keywords: Polyether ether ketone, anchor, inflammation, non-suppurative.
Interferential screws and anchors have played a major role in fixation of soft tissue to bony tunnel. It has enhanced enormous possibilities in the treatment of rotator cuff tear and shoulder instability. With advent of time, there developed metal anchors, biodegradable anchors, bioinert anchors, etc. Metal anchors had promising results along with complication of glenohumoral chondral damage secondary to exposed implant, implant migration, implant breakage, etc. [1]. Bioabsorbable anchors preferred over metal anchors due to their similar pull out strength to that of metallic anchor and minimal interference with post-operative magnetic resonance imaging (MRI) [2, 3, 4]. Biodegradable anchors had complications such as reactive synovitis, cyst formation, soft-tissue inflammation, and local osteolysis [5, 6, 7, 8]. Polyether ether ketone (PEEK) which was biologically inert and radiolucent was introduced to overcome the disadvantages of biodegradable anchors. These implants have shown no cytotoxicity, irritation, or microscopic reaction in animal studies with high pull-out strength [9]. PEEK does not interfere with MRI imaging and complications related to degradation and tissue reaction [10, 11, 12]. It has no local inflammatory reaction as per animal studies, but it has very poor osteointegration [13]. Despite wide spread orthopedic use, only few cases of minimal inflammatory reaction and a single case of hypersensitivity reaction have been documented [14]. Case involving osteolysis and foreign body reaction following rotator cuff repair with PEEK material suture anchor/screw has not been reported till now. We present a case of non-suppurative tissue reaction to PEEK anchor following rotator cuff repair.
A 58-year-old male patient presented to us with chief complain of pain in the right shoulder for 2 months with difficulty in raising the arm. Pain is localized to shoulder joint that aggravates with exertion and relieved with rest and medication. He had a history of trivial injury 2 months back. Pain was not relived with physiotherapy and medication.
On examination, there was not any sign of infection such as redness, swelling, or increased local temperature. Shoulder had not witnessed any previous fracture or surgery. Clinical sign for rotator cuff tear was positive. He had flexion 0°–80°, abduction 0°–15°, external rotation 0°–10°, and internal rotation 0°–15°. There was no visible muscle wasting around shoulder or scapula. At the time of presentation, the visual analog score was six. On investigation, his plain radiograph was normal other than minimal proximal migration of humeral head. MRI detected a full thickness tear of supraspinatus and infraspinatus tendon with proximal migration of humerus head and break in Maloney line (Fig. 1).
After all pre-operative preparations, mini open rotator cuff repair was done with two metallic suture anchor and two PEEK foot print suture anchor (Fig. 2). Suture removal was done 14 days following the operation and was uneventful. Nearly 3 weeks after operation, the patient complained of pain and mild rise of local temperature over shoulder. Clinical signs were normal other than mild warm at stich site compared to nearby skin. VAS score was five at this point of time with normal neutrophil and leucocyte count. Erythrocyte sedimentation rate and C-reactive protein (CRP) both positive with borderline procalcitonin test. We administered cefuroxime 500 mg twice daily for 7 days empirically. The patient improved clinically but his VAS score was 5 only. In 10 weeks from operation, his ESR decreased, but CRP was positive with normal neutrophil and leukocyte count. VAS score did not improve from a score of five. Nearly 3 months after operation, he presented with redness and serous discharge from stich site (Fig. 3). We immediately underwent an incision and drainage presuming all is not well. On incision, we found nearby muscles and soft-tissue healthy with collection of some pale-yellow semisolid substance near the screw site. At times, we were confused with tubercular affection. Sample was sent for routine culture sensitivity, grams stain, and cartridge-based nucleic acid amplification test (CBNAAT) for tuberculosis; all the test result was negative other than presence of pus cells in smear (Table 1).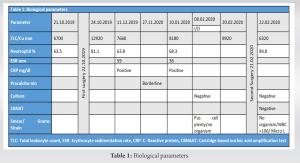
A 58-year-old male patient presented to us with chief complain of pain in the right shoulder for 2 months with difficulty in raising the arm. Pain is localized to shoulder joint that aggravates with exertion and relieved with rest and medication. He had a history of trivial injury 2 months back. Pain was not relived with physiotherapy and medication.
On examination, there was not any sign of infection such as redness, swelling, or increased local temperature. Shoulder had not witnessed any previous fracture or surgery. Clinical sign for rotator cuff tear was positive. He had flexion 0°–80°, abduction 0°–15°, external rotation 0°–10°, and internal rotation 0°–15°. There was no visible muscle wasting around shoulder or scapula. At the time of presentation, the visual analog score was six. On investigation, his plain radiograph was normal other than minimal proximal migration of humeral head. MRI detected a full thickness tear of supraspinatus and infraspinatus tendon with proximal migration of humerus head and break in Maloney line (Fig. 1).
After all pre-operative preparations, mini open rotator cuff repair was done with two metallic suture anchor and two PEEK foot print suture anchor (Fig. 2). Suture removal was done 14 days following the operation and was uneventful. Nearly 3 weeks after operation, the patient complained of pain and mild rise of local temperature over shoulder. Clinical signs were normal other than mild warm at stich site compared to nearby skin. VAS score was five at this point of time with normal neutrophil and leucocyte count. Erythrocyte sedimentation rate and C-reactive protein (CRP) both positive with borderline procalcitonin test. We administered cefuroxime 500 mg twice daily for 7 days empirically. The patient improved clinically but his VAS score was 5 only. In 10 weeks from operation, his ESR decreased, but CRP was positive with normal neutrophil and leukocyte count. VAS score did not improve from a score of five. Nearly 3 months after operation, he presented with redness and serous discharge from stich site (Fig. 3). We immediately underwent an incision and drainage presuming all is not well. On incision, we found nearby muscles and soft-tissue healthy with collection of some pale-yellow semisolid substance near the screw site. At times, we were confused with tubercular affection. Sample was sent for routine culture sensitivity, grams stain, and cartridge-based nucleic acid amplification test (CBNAAT) for tuberculosis; all the test result was negative other than presence of pus cells in smear (Table 1). Empirically, broad-spectrum antibiotic was administered. The patient was better than before but there was serous discharge from the stitch margin. We planned for a thorough debridement and nearly 4 months after first operation, we did another debridement under general anesthesia. We found similar straw color semisolid in consistency material near the screw site. Nearby, muscles were red, healthy, and contractile to stimulation. All the visible sutures and PEEK screw were removed (Fig. 4). Sample again sent for routine culture sensitivity, grams stain and CBNAAT; all the tests were negative other than increase number of WBC. Fortunately, patients improved from his symptoms and wound healed normally (Fig. 5). Patients present VAS score reduced to one at 6 months from the first surgery and 2 months from second surgery. There is marginal improvement of shoulder movement, no pain, and no rise of local temperature at 4 months following second surgery. At 25 months of follow-up, shoulder function is excellent without sign of local inflammation or recurrence of similar symptoms with VAS score one or less (Fig. 6).
Healing of soft tissue to bone needs stable fixation for a minimum period of 12 weeks. In the absence of this biomechanical stability, tissue will fail to heal [13, 15]. Soft tissue can be fixed to bone either by transosseous fixation or by anchors to bone. Metallic suture anchors have proved to replicate similar pull out strength as that of transosseous fixation [16, 17]. In due course time, metal anchors presented with complications such as loosening of fixation, migration of anchor, incarceration of the implant within the joint, and chondral damage, and most importantly, they interfered with the images in MRI [18, 19]. With the advent of biodegradable implants from 1990, it was postulated that they could avoid the complications of metallic screw. Pietschmann found that the pull-out strength of the biodegradable screws is as that of metallic screws [20]. As the biodegradable screws loose the mechanical strength with time due to degradation, the force is transferred to the soft tissue which helps in healing of the tissue [21]. Biodegradable screws degrade at different rate depending on their composition, ranging from few months for polyglycolic acid (PGA) to up to 5 years or more for poly-L-lactic acid (PLLA) [22, 23]. The first generation implants were made of PGA which degrades quickly before body could reabsorb the monomer debris leading to foreign body reactions [24]. The PLLA biodegradable implants were better in the sense that, they degraded slowly and allowed time for healing of the graft [25]. Biodegradable implants are associated with complication such as cyst formation, soft-tissue inflammation, and loose implant fragments in the joint and local osteolysis or foreign body Granulomas [5]. Rokkanen et al., in their study, described the occurrence of non-infectious foreign body reaction after 2–3 months following the use PGA suture anchors. This type of reaction was seen in 2% of patients with PGA implants but not seen in patients who received polylactide implants [26]. Freehill et al. documented substantial number of foreign body reactions, resulting in multiple osteolytic lesions and synovitis at the PLLA implant site in arthroscopic shoulder stabilization surgery. The usual presentation of symptoms was after 8 months of index surgery. Many of these patients had to manage with arthroscopic debridement, complete synovectomy, and implant removal [27]. Glueck et al. documented a case of extensive osteolysis in the humeral head 8 months after repair of a SLAP lesion with a poly L-lactide-co-D and L-lactide suture anchor [25]. In comparison to biodegradable materials, PEEK is a stable, which is resistant to chemical, thermal, and radiation induced degradation. PEEK does not interfere with MRI imaging which is an added advantage of PEEK and does not have tissue reaction to monomers [10, 11]. Even in animal studies, PEEK has been found be very stable without signs of acute inflammatory reaction, cytotoxicity, or immunogenicity to PEEK implants [13]. Ro et al. compared the bone reaction to different anchors used for repair of rotator cuff tear by post-operative MRI. At 9.6 months of operation, they found that 23 (10.8%, 23 of 213 patients) patients had developed peri-anchor cysts. It was 8.8%, 16.7%, and 12.5% in the all-suture-type, bioabsorbable, and PEEK-type anchor groups, respectively. There was no difference in all the groups in terms of visual analogue scale and Constant scores; re-tear rates, and peri-anchor bone reactions [28]. Haneveld et al. analyzed the osseous reaction in patients undergoing double row cuff repair, that is, using PLLA and PEEK suture anchors. He observed more tunnel widening with PLLA anchors compared to PEEK material (0.9 ± 0.7 mm in PLLA and 0.8 ± 0.6 mm in PEEK with P < 0.05) [29]. Kim et al., in their study on bone ingrowth into anchors, found that PEEK anchor had better bone ingrowth compared to non-vented biocomposite suture anchor at 12 months in patients with arthroscopic rotator cuff repair [30]. However, the rate of cyst formation around the anchor showed no difference between the two groups on the 6 months post-operative computed tomography.
We learn from the literature that PEEK is a more stable material compared to other biocomposite materials, but it has witnessed osteolysis, cyst around anchor, etc. We could not find any article depicting about the non-suppurative inflammation related to PEEK implant. We present the first such case of rotator cuff repair with metallic anchor and PEEK screws with significant non-suppurative inflammation around the PEEK anchor. In our case, none of the samples were positive for any culture or CBNAAT. The collection was purely non-suppurative and none of the samples revealed any organism in Gram’s stain. After the initial debridement, inflammation did not subside till removal of PEEK anchor at second debridement. Inflammation subsided to near completion with removal of the PEEK screw and debridement. Most importantly, the necrotic material was directly at the vicinity of screw with normal contractile healthy musculature all around. The underlying mechanism for such a non-suppurative inflammation with PEEK is not clear. It could be a reaction to PEEK implant or to the non-absorbable suture material attached to the anchor is a matter of debate. Although there is hardly any literature on non-suppurative reaction of PEEK material, few cases of local inflammation, osteolysis, and cyst around anchor have been reported. Further studies are needed to describe the biological reaction of PEEK monomer and the mechanism for non-suppurative inflammation around the suture anchor.
There were cases of tissue reaction to PEEK material in the literature such as osteolysis and cyst formation. In addition, non-suppurative inflammation can occur in response to PEEK material. Awareness about the non-suppurative inflammation property of PEEK material may help future surgeons to manage the condition better than us. Further studies on PEEK material can substantiate the relation of PEEK to non-suppurative inflammation.v
PEEK material produces local cyst and bone osteolysis as depicted in the literature. However, non-suppurative inflammation can occur in response to PEEK material. Early suspicion and action will prevent propagation of disease and osteolysis of bone.
References
- 1.1. Godinho GG, França FO, Alves Freitas JM, Aguiar PN, de Carvalho Leite M. Complications resulting from the use of metal anchors in shoulder arthroscopy. Rev Bras Ortop 2015;44:143-7. [Google Scholar]
- 2.2. Barber FA, Herbert MA, Coons DA, Boothby MH. Sutures and suture anchors--update 2006. Arthroscopy 2006;22:1063.e1-9. [Google Scholar]
- 3.3. Schneeberger AG, von Roll A, Kalberer F, Jacob HA, Gerber C. Mechanical strength of arthroscopic rotator cuff repair techniques: An in vitro study. J Bone Joint Surg Am 2002;84:2152-60. [Google Scholar]
- 4.4. Spoliti M. Glenoid osteolysis after arthroscopic labrum repair with a bioabsorbable suture anchor. Acta Orthop Belg 2007;73:107-10. [Google Scholar]
- 5.5. Nusselt T, Freche S, Klinger HM, Baums MH. Intraosseous foreign body granuloma in rotator cuff repair with bioabsorbable suture anchor. Arch Orthop Trauma Surg 2010;130:1037-40. [Google Scholar]
- 6.6. Park AY, Hatch JD. Proximal humerus osteolysis after revision rotator cuff repair with bioabsorbable suture anchors. Am J Orthop (Belle Mead NJ) 2011;40:139-41. [Google Scholar]
- 7.7. Kim SH, Oh JH, Lee OS, Lee HR, Hargens AR. Postoperative imaging of bioabsorbable anchors in rotator cuff repair. Am J Sports Med 2014;42:552-7. [Google Scholar]
- 8.8. McCarty LP 3rd, Buss DD, Datta MW, Freehill MQ, Giveans MR. Complications observed following labral or rotator cuff repair with use of poly-L-lactic acid implants. J Bone Joint Surg Am 2013;95:507-11. [Google Scholar]
- 9.9. Kurtz SM, Devine JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007;28:4845-69. [Google Scholar]
- 10.10. Brantigan JW, McAfee PC, Cunningham BW, Wang H, Orbegoso CM. Interbody lumbar fusion using a carbon fiber cage implant versus allograft bone. An investigational study in the Spanish goat. Spine (Phila Pa 1976) 1994;19:1436-44. [Google Scholar]
- 11.11. Brantigan JW, Steffee AD. A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine (Phila Pa 1976) 1993;18:2106-7. [Google Scholar]
- 12.12. Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM. Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: Two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine (Phila Pa 1976) 2000;25:1437-46. [Google Scholar]
- 13.13. Tuoheti Y, Itoi E, Yamamoto N, Seki N, Abe H, Minagawa H, et al. Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med 2005;33:1869-74. [Google Scholar]
- 14.14. Maldonado-Naranjo AL, Healy AT, Kalfas IH. Polyetheretherketone (PEEK) intervertebral cage as a cause of chronic systemic allergy: A case report. Spine J 2015;15:e1-3. [Google Scholar]
- 15.15. Burkhart SS, Lo IK. Arthroscopic rotator cuff repair. J Am Acad Orthop Surg 2006;14:333-46. [Google Scholar]
- 16.16. Hecker AT, Shea M, Hayhurst JO, Myers ER, Meeks LW, Hayes WC. Pull-out strength of suture anchors for rotator cuff and Bankart lesion repairs. Am J Sports Med 1993;21:874-9. [Google Scholar]
- 17.17. Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy 2009;25:788-93. [Google Scholar]
- 18.18. Gaenslen ES, Satterlee CC, Hinson GW. Magnetic resonance imaging for evaluation of failed repairs of the rotator cuff. Relationship to operative findings. J Bone Joint Surg Am 1996;78:1391-6. [Google Scholar]
- 19.19. Ozbaydar M, Elhassan B, Warner JJ. The use of anchors in shoulder surgery: A shift from metallic to bioabsorbable anchors. Arthroscopy 2007;23:1124-6. [Google Scholar]
- 20.20. Pietschmann MF, Fröhlich V, Ficklscherer A, Gülecyüz MF, Wegener B, Jansson V, et al. Suture anchor fixation strength in osteopenic versus non-osteopenic bone for rotator cuff repair. Arch Orthop Trauma Surg 2009;129:373-9. [Google Scholar]
- 21.21. Böstman OM, Pihlajamäki HK. Late foreign-body reaction to an intraosseous bioabsorbable polylactic acid screw. A case report. J Bone Joint Surg Am 1998;80):1791-4. [Google Scholar]
- 22.22. Böstman OM. Absorbable implants for the fixation of fractures. J Bone Joint Surg Am 1991;73:148-53. [Google Scholar]
- 23.23. Bergsma JE, de Bruijn WC, Rozema FR, Bos RR, Boering G. Late degradation tissue response to poly(L-lactide) bone plates and screws. Biomaterials 1995;16:25-31. [Google Scholar]
- 24.24. Böstman OM, Pihlajamäki HK. Adverse tissue reactions to bioabsorbable fixation devices. Clin Orthop Relat Res 2000;371:216-27. [Google Scholar]
- 25.25. Glueck D, Wilson TC, Johnson DL. Extensive osteolysis after rotator cuff repair with a bioabsorbable suture anchor: A case report. Am J Sports Med 2005;33:742-4. [Google Scholar]
- 26.26. Rokkanen PU, Böstman O, Hirvensalo E, Mäkelä EA, Partio EK, Pätiälä H, et al. Bioabsorbable fixation in orthopaedic surgery and traumatology. Biomaterials 2000;21:2607-13. [Google Scholar]
- 27.27. Freehill MQ, Harms DJ, Huber SM, Atlihan D, Buss DD. Poly-L-lactic acid tack synovitis after arthroscopic stabilization of the shoulder. Am J Sports Med 2003;31:643-7. [Google Scholar]
- 28.28. Ro K, Pancholi S, Son HS, Rhee YG. Perianchor cyst formation after arthroscopic rotator cuff repair using all-suture-type, bioabsorbable-type, and PEEK-type anchors. Arthroscopy 2019;35:2284-92. [Google Scholar]
- 29.29. Haneveld H, Hug K, Diederichs G, Scheibel M, Gerhardt C. Arthroscopic double-row repair of the rotator cuff: A comparison of bio-absorbable and non-resorbable anchors regarding osseous reaction. Knee Surg Sports Traumatol Arthrosc 2013;21:1647-54. [Google Scholar]
- 30.30. Kim JH, Kim YS, Park I, Lee HJ, Han SY, Jung S, et al. A comparison of open-construct PEEK suture anchor and non-vented biocomposite suture anchor in arthroscopic rotator cuff repair: A prospective randomized clinical trial. Arthroscopy 2020;36:389-96. [Google Scholar]











