Non-tuberculous mycobacterial infections must be suspected in operated cases with low grade indolent infections, and appropriately treated with source control and targeted antibiotics.
Dr. Aditya Menon, Department of Orthopaedics, PD Hinduja Hospital and MRC, Veer Savarkar Marg, Mumbai - 400 016, Maharashtra, India. E-mail: docmenon83@gmail.com
Introduction: Non-tuberculous mycobacteria (NTM) infections of the musculoskeletal system are commonly missed due to their rarity and the absence of systemic symptoms. Here, we present a rare case of NTM infection following repair of an avulsed pectoralis major tendon in an immunocompetent host managed by a multi-disciplinary team specializing in musculoskeletal infections.
Case Report: A 23-year-old male patient presented with discharging sinus in the right axilla for 6 months. He sustained the right pectoralis major muscle avulsion following an accident which was surgically repaired using FiberWire® and endo buttons. He developed a discharging sinus 4-month post-surgery. He presented with persistent infection in spite of empirical antibiotics elsewhere. Radiographs and MRI sonogram showed intra-medullar endo buttons in the proximal humerus with marginal pus collection in the axillary region with minimal medial extension into pectoralis major and minor muscles along the superior aspect. A detailed plan was made with inputs from a multidisciplinary bone infection team. Wound was radically debrided, implants and sutures removed, humerus scraped, and tissues sent for microbiology and histopathology. Extended incubation of deep tissue culture as suggested by ID specialists grew Rapidly growing mycobacteria, a type of NTM 3 weeks after surgery. Patient was started on intravenous amikacin along with oral clarithromycin and linezolid based on antibiotic susceptibility. Wound discharge persisted for almost 5-week post-surgery and stopped 2 weeks after initiation of appropriate antibiotics. Amikacin was given for 1 month and oral antibiotics were continued for 6 months. The pectoralis major function was unaffected after surgery and patient returned to normal activities 3 months after debridement. Patient has an infection free follow-up of 4 years.
Conclusion: This case outlines the importance of having a high degree of suspicion for the diagnosing orthopedic NTM infections. In addition, it showcases the advantages of having good communication between surgeons, infectious disease specialist, and microbiologist for achieving good functional outcomes.
Keywords: Surgical site infection, FiberWire®, tendon repair, atypical mycobacteria, debridement, sinogram, endo button.
Nontuberculous mycobacteria (NTM) infections of the musculoskeletal system are commonly missed due to their rarity and the absence of systemic symptoms [1] Previously thought to be saprophytes and a rare infection in humans, observed particularly in immunocompromised patients and elderly, a high clinical index of suspicion is required to recognize such infections as they may occur in immunocompetent hosts [2]. Clinically and on histopathology, musculoskeletal infections caused by NTM resemble, those caused by Mycobacterium tuberculosis, but are mostly resistant to routine anti-tuberculous therapy (ATT). Immunocompetent patients usually present with focal infections in tendon sheaths, bursa, joints, and bones, which are caused by direct inoculation of the organisms through trauma, penetrating injury, needle injection, or contamination during surgical procedures [2]. Here, we present a rare case of NTM infection following repair of an avulsed pectoralis major tendon in an immunocompetent host managed by a multi-disciplinary team specializing in musculoskeletal infections.
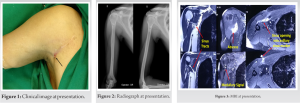
A 23-year-old male patient presented to our institute in November 2016 with discharging sinus in the right axilla for 6 months. He had an alleged history of fall from bike in February 2016 after which he sustained a right pectoralis major muscle avulsion from its humeral attachment. Open repair was done with FiberWire® and endo buttons. In June 2016 (4 months after primary surgery), he developed discharging sinus from axillary region. Discharge was purulent scanty, intermittent, and non-foul smelling. There was no history of fever, weight loss, pain, or restriction of movements. Infection persisted in spite of empirical antibiotics. The wound was not surgically debrided before presentation. He presented to us 5 months after developing the sinus. There was a well healed scar of the previous surgery, with a small sinus over anterior axillary fold in the superior part of the scar (Fig. 1). Discharge was seropurulent and non-foul smelling. There was no tenderness, erythema, or other signs of inflammation around the sinus. Range of motion of shoulder joint was normal and free. Radiographs showed intramedullar endo buttons in the proximal humerus (Fig. 2). MRI of the right chest wall with sinography revealed marginal pus collection in the axillaryregion measuring 3.2 × 2.0 × 1.2 cm with minimal medial extension into pectoralis major and minor muscles along the superior aspect. Three sinus tracts leading from this collection were found converging into axillary discharging sinus at marker site (Fig. 3).
Rest of the bones and soft tissues of shoulder and chest wall appeared unremarkable. Pre-operative consult with infectious disease (ID) specialist was sought. Detailed history was recorded, wound analyzed, and appropriate tissue sampling was recommended to the orthopedic team by the ID specialist. The ID specialist emphasized on the need for extended incubation suspecting slow growth pathogens such as cutibacterium acnes commonly seen infecting surgeries around the shoulder. Exploration, debridement of anterior axillary abscess with implant removal was planned. Surgical planning included:
1. Proposed incision – must include the sinus and previous surgical scar
2. Identifying the sinus tracts as delineated on the sinogram
3. Tracing the sinuses to their origin
4. Identifying all the suture materials within the pectoralis major muscle
5. Excising all necrotic tissue and suture materials and send for aerobic, anaerobic, fungal, mycobacterial cultures, and histopathology; Incubate the tissues for an extended period
6. Making an oval window in the humerus at the site on insertion of endo buttons
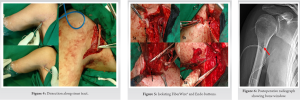
7. Removing buttons and scraping adjacent medullary canal Accordingly, a wide V-shaped incision was taken excising all the previous scar and sinus. Dissection was continued along the sinus tract going up to the humerus (Fig. 4). The previous avulsion of tendon from the bone was found to be healed. FiberWire® suture and tape were identified and found to be embedded in substance of the lower half of sternal head of pectoralis major with surrounding infected granulation tissue (Fig. 5a). It was traced toward lateral chest wall leading to walled purulent collection, which was drained and walls excised. Second FiberWire® was then found in clavicular part of muscle which was then traced laterally to the endo button on humeral attachment (Fig. 5b). Bone window was created in proximal humerus and both endo buttons were removed (Fig. 5c, 5d and 6).
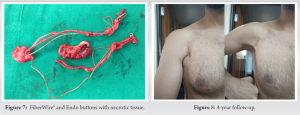
Intramedullary canal was scooped and scraped. FiberWire® and endo buttons were excised en masse along with the infected tissues around them (Fig. 7). Samples were sent for histopathology and culture (bacterial, fugal, mycobacterial, and Gene Xpert). Post-operative radiograph showed oval window through which medullary canal was scraped (Fig. 6). The histopathology reported chronic inflammation with occasional suture granulomas. There was no evidence of malignancy or tuberculosis. Extended incubation of deep tissue culture as suggested by ID specialists grew Rapidly growing mycobacteria, a type of non-tuberculous mycobacterium (NTM) 3 weeks after surgery. Patient was started on intravenous amikacin along with oral clarithromycin and linezolid based on antibiotic susceptibility. Wound discharge persisted for almost 5-week post-surgery and stopped 2 weeks after initiation of appropriate antibiotics. Amikacin was given for 1 month and oral antibiotics were continued for 6 months as per international guidelines. Amikacin was stopped once inflammatory markers showed a downward trend and wound showed no evidence of active infection. Audiometry was done before starting Amikacin to rule out any sensory-neural deafness. Patient was advised to report any reduction in hearing during therapy. Blood parameters such as complete blood count, ESR, CRP, and renal function tests were monitored every 15 days to watch for side effects and trend in inflammatory markers. The pectoralis major function was unaffected after surgery and patient returned to normal activities 3 months after debridement. Patient has an infection free follow-up of 4 years (Fig. 8).
We report a unique case where an uncommon muscle tear of the pectoralis major developed secondary NTM infection after surgical repair using FiberWire® and endo buttons. The thought process encompassed appropriate pre-operative imaging, pre-operative surgical plan, execution of surgical plan, appropriate microbiology and histopathology tests, and targeted antibiotics. A pre-operative sonogram and MRI help define the course and extent of the sinus tract and its possible communications with neighboring structures [3]. The incidence of NTM infection is increasing worldwide. The most common clinical syndrome is pulmonary disease, but recent retrospective studies of laboratory records have revealed that 20–30% of NTM isolates are of extrapulmonary origin [4]. Clinically, musculoskeletal infection caused by NTM resemble chronic granulomatous infection and is commonly diagnosed as tuberculosis, especially in countries where TB is endemic [5]. The histopathology is often suggestive of chronic granulomatous reaction, confusing the picture with other granulomatous lesions such as foreign body granuloma or tuberculosis [6]. Accompanied by clinical data, such as history of open wound or surgical procedure or injections, it can help to establish the presumptive diagnosis of NTM infection [2]. However, the gold standard in diagnosis is the identification of Mycobacterium species in culture. The microbiological diagnosis includes direct microscopic observation of the microorganism in the samples, culture in selective media, and identification of the isolated species by phenotypic, molecular, biochemical, and chromatographic techniques. Besides confirming diagnosis, it allows us to do drug sensitivity so that appropriate drug regimen can be selected, as NTM is usually resistant to routine ATT and there is a variability in susceptibility among species. NTM musculoskeletal infections usually require combined medical and surgical management. Removal of all infected tissue is essential, and a minimum of 6 months of multidrug antibiotic therapy, determined according to the antibiotic susceptibilities of the organism, is usually recommended but the optimal length of therapy is yet not known [2, 5]. Our patient had clinical improvement on initiation of targeted antibiotics which were continued for 6 months. Surgical site infection with NTM in an immunocompetent host, especially following orthopedic surgeries, is rare [7], and the authors could not find reports in English literature of one after repair of Pectoralis Major Avulsion. There have been a few reports of stitch granulomas/surgical site infection associated with the use of FiberWire® [8, 9]. Ollievere et al. have reported a case of foreign body granuloma after the repair of tendoachillis with FiberWire®. It seemed highly likely to the author that the significant excursion of the Achilles tendon resulted in fatigue failure of the suture and subsequent abrasion of the material resulted in the generation of polyethylene particulate wear debris [8]. Willmott et al. reported similar complications after using FiberWire® tightropes in the treatment of ankle diastasis [10]. In a series of six patients where the FiberWire® device was used, two patients required removal of the suture as a result of inflammatory complications at 6–10 months following their initial surgery. Mack et al. have described five patients out of 178 with traumatic lower limb amputations who suffered with draining sinuses through previously well-healed incisions [9]. This was associated with a FiberWire® suture material and was confirmed by histopathological analysis. None of these reports mentioned NTM involvement. Our case highlights the importance of a multidisciplinary approach, where detailed pre-, intra, and post-operative communication between the orthopedic surgeons, ID specialist, and microbiologists helped identify a slow growing organism.
This case outlines the importance of having a high degree of suspicion for the diagnosing orthopedic NTM infections. In addition, it showcases the advantages of having good communication between surgeons, infectious disease specialist, and microbiologist for achieving good functional outcomes.
Non tuberculous mycobacterial infections must be suspected in operated cases with low-grade indolent infections. Appropriate imaging, surgical planning, and a multidisciplinary approach ensure a good functional outcome.
References
- 1.Bi S, Hu FS, Yu HY, Xu KJ, Zheng BW, Ji ZK, et al. Nontuberculous mycobacterial osteomyelitis. Infect Dis (Lond) 2015;47:673-85. [Google Scholar]
- 2.Gundavda MK, Patil HG, Agashe VM, Soman R, Rodrique s C, De shpande RB. Nontube rculous mycobacterial infection of the musculoskeletal system in immunocompetent hosts. Indian J Orthop 2017;51:205-12. [Google Scholar]
- 3.Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: The role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg 2009;23:80-9. [Google Scholar]
- 4.Kham-Ngam I, Chetchotisakd P, Ananta P, Chaimanee P, Sadee P, Reechaipichitkul W, et al. Epidemiology of and risk factors for extrapulmonary nontuberculous mycobacterial infections in Northeast Thailand. PeerJ 2018;6:e5479. [Google Scholar]
- 5.Lim JM, Kim JH, Yang HJ. Management of infections with rapidly growing mycobacteria after unexpected complications of skin and subcutaneous surgical procedures. Arch Plast Surg 2012;39:18-24. [Google Scholar]
- 6.Orme IM, Ordway DJ. Host response to nontuberculous mycobacterial infections of current clinical importance. Infect Immun 2014;82:3516-22. [Google Scholar]
- 7.Goldstein N, St Clair JB, Kasperbauer SH, Daley CL, Lindeque B. Nontuberculous mycobacterial musculoskeletal infection cases from a tertiary referral center, Colorado, USA. Emerg Infect Dis 2019;25:1075-83. [Google Scholar]
- 8.Ollivere BJ, Bosman HA, Bearcroft PW, Robinson AH. Foreign body granulomatous reaction associated with polyethelene “Fiberwire®” suture material used in Achilles tendon repair. Foot Ankle Surg 2014;20:e27-9. [Google Scholar]
- 9.Mack AW, Freedman BA, Shawen SB, Gajewski DA, Kalasinsky VF, Lewin-Smith MR. Wound complications following the use of fiberwire in lower-extremity traumatic amputations. J Bone Joint Surg Am 2009;91:680-5. [Google Scholar]
- 10.Willmott HJ, Singh B, David LA. Outcome and complications of treatment of ankle diastasis with tightrope fixation. Injury 2009;40:1204-6. [Google Scholar]