Although technically demanding, the management of unstable SCFE in adolescents using a modified Dunn procedure with safe surgical dislocation of the hip is highly effective with good functional outcomes.
Dr. Arulkumar Nallakumarasamy, Department of Orthopaedics, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: arulmmcian@gmail.com
Introduction: Slipped capital femoral epiphysis (SCFE) is commonly managed by in situ screw fixation. However, higher grades of slips require restoration of normal anatomy of the femoral head without compromising the blood supply.
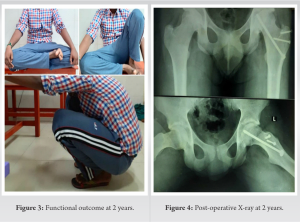
Case Report: A 16-year-old adolescent male presented with the left hip pain and progressive limping for 4 days with no history of previous trauma. On examination, the patient had severe tenderness and gross restriction of movements. Radiological examination revealed Grade 2 acute on chronic SCFE with unstable slip. Modified Dunn procedure through Ganz surgical hip dislocation facilitated the complete restoration of normal anatomy without avascular necrosis of femoral head changes at 2 years of follow-up.
Conclusion: Ganz safe surgical dislocation of the hip is safe for the femoral head, preserving its blood supply in toto and the modified Dunn procedure facilitated the complete restoration of normal anatomy even in acute on chronic type of SCFE cases.
Keywords: Slipped capital femoral epiphysis, Southwick angle, Ganz dislocation, Dunn procedure.
Slipped capital femoral epiphysis (SCFE) is a well-known disorder of adolescent hips. The common management employed is in situ screw fixation with acceptance of any deformity, for the fear of compromising femoral head vascularity in attempting to reduction [1, 2]. Many recent studies have shown that the residual deformity may lead to Femoro-Acetabular Impingement (FAI) eventually resulting in osteoarthritis [3, 4, 5]. Hence, efforts should be made to restore the normal anatomy of the femoral head, with utmost care to preserve the proximal femur blood supply.
A 16-year-old adolescent male presented with the left hip pain and progressive limping for 4 days without any history of significant previous trauma. The limp was mild initially progressing slowly to the level of severe inability to bear weight and walk. On examination, the systemic examination was found to be normal. Anthropometric measurements revealed tall stature and a pear-shaped body with a waist-hip ratio of 0.96. There was severe tenderness in the left hip with gross restriction of movements. External rotation and flexion were more painful than the rest of the movements. The patient was unable to bear weight and was having aided gait with assistance from family members. Basic blood investigations were found to be within normal limits. Radiographic evaluation showed a Southwick angle of 50° categorizing the patient into a moderate degree of SCFE, as shown in (Fig. 1). The X-ray also revealed attempted callus and remodeling in the neck region due to a pre-existent slip which warrants subcapital osteotomy procedures. Hence, the modified Dunn procedure through Ganz safe surgical dislocation of the hip was planned. Acute onset of pain with total inability to bear weight could be due to fracture or SCFE. The assisted gait with pain on weight-bearing could be due to synovitis or Perthes disease. However, the absence of warmth, fever, and other constitutional symptoms ruled out synovitis of the hip joint. The adolescent age group ruled out Perthes disease considering that even late-onset Perthes has been reported only as late as 14 to 15 years. Furthermore, radiological evaluation clearly shows increased Southwick angle pointing toward SCFE. Neck remodeling substantiates the diagnosis of a chronic SCFE, in which an acute slip has occurred. Through the lateral approach, the gluteus maximus was reached. Gibson interval between the anterior border of gluteus maximus and gluteus medius accessed. Piriformis tendon is identified and the interval between piriformis tendon and gluteus minimus is identified. This interval is sharply dissected for 1–2 cm. Trochanteric flip osteotomy is done with a fragment thickness of about 1.5 cm leaving behind at least a 5 mm cuff of the gluteus medius. Z-shaped capsular incision is made starting from the anterior edge of the osteotomy site and going longitudinally toward the acetabulum. Then, it is directed posteriorly along the edge of the acetabulum. Epiphysis and neck transfixed with a K wire. Then, the head is safely dislocated by flexion and external rotation of the hip, as shown in (Fig. 2).
SCFE is a common disorder in an adolescent male with characteristic features of hypothyroidism, hypogonadism such as obesity, abdominal striations, reduced pubic and axillary hair, and osteodystrophy [6, 7, 8]. Various researchers have suggested the genetic predisposition (X-linked dominant, autosomal dominant with variable penetrance, and autosomal recessive) in the occurrence of SCFE [9, 10]. The clinical symptomatology varies for acute [pain in the groin, inner thigh, and limping] and chronic [muscle wasting, chronic pain, and stiffness] presentation of SCFE. Gait may be altered with the leg outward [11,12]. Chronic cases with bony compensation may present acutely with slip due to trivial trauma or any of the multifactorial causes [13]. Radiology is the ultimate investigation in staging the slip, assessing the degree of slip angle, apprehending the severity, and framing the treatment plan [1, 14]. It can also prognosticate the inherent possibility of the slip occurring in the opposite hip [1]. Simple AP and Frog leg lateral views are adequate in assessing the slip. However, in acute presentation, wherein hip abduction is not possible to obtain the frog-leg lateral view, a CT scan of the pelvis comes to the rescue [15, 16]. Management of SCFE is based on two factors, namely, the grade of the slip (Southwick angle) and the stability (stable/unstable) of the slip [1, 14]. A mild degree of slip is managed by in situ pinning. Moderate-to-severe cases warrant subcapital osteotomy procedures to restore the normal anatomy to avoid future FAI. Safe surgical dislocation of the hip was described by Ganz et al., in 2001, which facilitates procedures on the femoral head and neck at the same time without affecting its blood supply. This approach is also used for fixing femoral head fractures [17]. Dunn, in 1964, described a promising surgical technique for subcapital reorientation with an AVN risk of only 4% [18]. Recent studies show that the modified Dunn procedure done through Ganz safe hip dislocation provides excellent results both radiologically and functionally [19, 20]. Our patient is a case of Grade 2 unstable slip managed by modified Dunn procedure through Ganz surgical hip dislocation has resulted in very good outcome and complete correction of slip angle.
The effective hip joint preservation surgery for acute on chronic SCFE in adolescents is still controversial. The modified Dunn procedure restores the normal alignment of the caput-column of the proximal femur. It maintains the viability of the femoral head by preserving the precarious retinacular vessels and further the limb length discrepancy can be prevented by relocating the epiphysis without shortening the femoral neck.
The modified Dunn osteotomy through safe surgical dislocation of the hip addresses the physeal slippage directly under vision without compromising the precarious vascularity. The goal of “hip preservation surgeries” with the described technique is to prevent femoroacetabular impingement, avascular necrosis, and osteoarthritis.
References
- 1.Aprato A, Conti A, Bertolo F, Massè A. Slipped capital femoral epiphysis: Current management strategies. Orthop Res Rev 2019;11:47-54. [Google Scholar]
- 2.Naseem H, Chatterji S, Tsang K, Hakimi M, Chytas A, Alshryda S. Treatment of stable slipped capital femoral epiphysis: Systematic review and exploratory patient level analysis. J Orthop Traumatol 2017;18:379-94. [Google Scholar]
- 3.Hosalkar HS, Pandya NK, Bomar JD, Wenger DR. Hip impingement in slipped capital femoral epiphysis: A changing perspective. J Child Orthop 2012;6:161-72. [Google Scholar]
- 4.Chaudhry H, Ayeni OR. The etiology of femoroacetabular impingement. Sports Health 2014;6:157-61. [Google Scholar]
- 5.Pierannunzii L. Femoroacetabular impingement: Question-driven review of hip joint pathophysiology from asymptomatic skeletal deformity to end-stage osteoarthritis. J Orthop Traumatol 2019;20:32. [Google Scholar]
- 6.Kadowaki S, Hori T, Matsumoto H, Kanda K, Ozeki M, Shirakami Y, et al. Prepubertal onset of slipped capital femoral epiphysis associated with hypothyroidism: A case report and literature review. BMC Endocr Disord 2017;17:59 [Google Scholar]
- 7.Huang YF, Wang LS, Zhang S, Gao YH, Liu JG, Qi X. Slipped capital femoral epiphysis in an adult with congenital hypopituitarism. Medicine (Baltimore) 2019;98:e13997. [Google Scholar]
- 8.Rajaratnam H, Karuppiah D, Sridaran S. Slipped capital femoral epiphysis in a boy with hypogonadism. Sri Lanka J Diabetes Endocrinol Metab 2012;1:48-50. [Google Scholar]
- 9.Loder RT, Skopelja EN. The epidemiology and demographics of slipped capital femoral epiphysis. ISRN Orthop 2011;2011:486512 [Google Scholar]
- 10.Novais EN, Millis MB. Slipped capital femoral epiphysis: Prevalence, pathogenesis, and natural history. Clin Orthop 2012;470:3432-8 [Google Scholar]
- 11.Millis MB. SCFE: Clinical aspects, diagnosis, and classification. J Child Orthop 2017;11:93-8. [Google Scholar]
- 12.Johns K, Mabrouk A, Tavarez MM. Slipped Capital Femoral Epiphysis. Treasure Island (FL): StatPearls Publishing; 2022. [Google Scholar]
- 13.Herngren B, Stenmarker M, Vavruch L, Hagglund G. Slipped capital femoral epiphysis: A population-based study. BMC Musculoskelet Disord 2017;18:304. [Google Scholar]
- 14.Peck D. Slipped capital femoral epiphysis: Diagnosis and management. Am Fam Physician 2010;82:258-62. [Google Scholar]
- 15.Hesper T, Zilkens C, Bittersohl B, Krauspe R. Imaging modalities in patients with slipped capital femoral epiphysis. J Child Orthop 2017;11:99. [Google Scholar]
- 16.Wako M, Koyama K, Takayama Y, Haro H. The characteristics of the whole pelvic morphology in slipped capita l femora lepiphysis. Medicine (Baltimore) 2020;99:e19600. [Google Scholar]
- 17.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001;83:1119-24. [Google Scholar]
- 18.Dunn DM. The treatment of adolescent slipping of the upper femoral epiphysis. J Bone Joint Surg Br 1964;46:621-9. [Google Scholar]
- 19.Zuo B, Zhu JF, Wang XY, Wang CL, Ma F, Chen XD. Outcome of the modified Dunn procedure in severe slipped capital femoral epiphysis. J Orthop Surg 2020;15:506. [Google Scholar]
- 20.Agashe MV, Pinto DA, Vaidya S. Modified Dunn osteotomy for moderate and severe slipped capital femoral epiphysis-a retrospective study of thirty hips. Indian J Orthop 2021;55:100. [Google Scholar]