Spinal epidural abscess in Tuberculosis of spine need early diagnosis and treatment by decompression.
Dr. Zafar Iqbal, Department of Orthopaedics, Dr. Shankarrao Chavan Government Medical College, Nanded - 431 606, Maharashtra, India. E-mail: docmdzafariqbal@gmail.com
Introduction: Spinal epidural abscess (SEA) refers to collection of infection of the epidural space due to various etiologies. Tuberculosis (TB) of the spine is one of the important causes of SEA. Patient with SEA usually presents with history of fever, back pain, difficulty in walking, and neurological weakness. Magnetic resonance imaging (MRI) is the initial modality for diagnosis and it can be confirmed by examination of abscess for microorganism growth. It can be treated by laminectomy and decompression which helps to drain out the pus and relive the compression on the cord.
Case Report: A 16-year-old male, student by profession, presented with a history of low back pain and progressive difficulty in walking for the past 12 days and lower limb weakness for the past 8 days associated with fever, generalized weakness, and malaise. Computed tomography brain and whole spine showed no significant changes MRI left facetal joint of L3 L4 vertebrae infective arthritis with abnormal soft-tissue collection in the posterior epidural region extending from D11-L5 vertebrae causing compression on the thecal sac, cauda equine nerve roots, and represents infective abscess with abnormal soft-tissue collection in the posterior paraspinal region and left psoas muscles representing infective abscess. Patient was taken for emergency decompression with clearance of abscess through posterior approach. Laminectomy was done extending from D11 TO L5 vertebrae and thick pus was drained through multiple pockets. Samples pus and soft tissue were sent for investigation. Pus culture ZN and Gram’s stain did not show growth of any organism, but GeneXpert was positive for growth of Mycobacterium tuberculosis. Patient was registered under RNTCP program and anti TB drugs were started as per the weight scale. Sutures were removed on post-operative day 12 and neurological evaluation was done for any signs of improvement. Patient showed improvement of power in both lower limb; power 5/5 on the right lower limb whereas 4/5 in the left lower limb. Patient also had improvements in other symptoms and has no complaints of back ache and malaise at discharge.
Conclusion: Tuberculous thoracolumbar epidural abscess is a rare disease with potential to cause lifelong vegetative state if diagnosis and treatment is not done promptly. Surgical decompression by unilateral laminectomy and evacuation of collection is both diagnostic and therapeutic.
Keywords: Spinal epidural abscess, thoracolumbar abscess, tuberculosis.
Thoraco-lumbar epidural abscess is an uncommon pathology with incidence rate of 1-2/10,000 [1] while tuberculosis (TB) accounts for only 2% of these abscesses [2, 3]. These abscess needs emergency decompression and drainage of pus to release the decompressive pressure on the epidural sac, spinal cord, and the roots. This case report presents a rare case of thoracolumbar epidural abscess of tubercular origin with extension of abscess into the left psoas muscle in an adolescent male presenting with bilateral lower limb weakness, loss of appetite, and low back pain at a tertiary care center.
A 16 years male, student by profession, came to Medicine outpatient department of our Institute with complaints of generalized weakness, malaise, episode of fever, lower limb weakness, and inability to walk. Patient was admitted under medicine care and was later transferred to orthopedics side after magnetic resonance imaging (MRI) reports were available. Patient initially had an episode of fever 12 days back following which he developed low back pain, malaise, and generalized weakness. Patient later developed progressive weakness of bilateral lower limb. Initially, he was able to walk with support but later he could not walk even with support. On examination, patient looked pale and cachexic, his general condition was moderate, afebrile with pulse rate of 88 beats/min, blood Pressure 114/70 mmHg, temperature 37.8°C, and SpO2 99% (in room air). On physical examination, patient was not able to walk. Severe tenderness was present in paraspinal region of dorsolumbar part of back and was radiating to the left buttock and hip. Flexion and extension of spine were severely painful. On neurological evaluation, patient had decreased power in both lower limb at hip and knee only, 4/5 on the right side whereas it was 3/5 on the left (Fig. 1).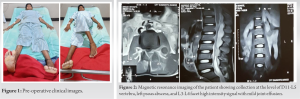

TB is a common disease in developing countries due to low socioeconomic status. Vertebral TB is a relatively rare entity accounting for <1% of all the TB in the body [4] and 50% of all musculoskeletal TB. It is considered the most serious type of skeletal TB, with possible neurological symptoms due to compression of the neural structures. It may also lead to deformity and significant vertebral structure destruction and instability [5]. The gravity of situation demands for early diagnosis and prompt treatment for good outcome. The delayed/missed diagnosis can lead or progress to neurological complications like even cauda equina syndrome [6]. Spinal epidural abscess (SEA) is a very rare entity especially without significant bony involvement [7]. Tubercular SEA develops secondary to vertebral body involvement, and rarely by hematogenous spread from a primary focus in the body [8, 9, 10]. The clinical presentation of tubercular SEA may be more insidious, leading to failure of early diagnosis treatment [6]. Patient with SEA presents with low back pain, fever, and weakness of limbs depending on the extent of involvement. Triad of fever, backache, and neurodeficit is seldom the presenting feature, found only in about 2% of the cases [2]. Thorough clinical examination and radiological investigations, it helps in reaching the diagnosis. MRI is the investigation of choice. TB can have a varied presentation, generally there are irregular hyper-intense lesions on T2-weighted images with erosion of the vertebral body and abscess collection around the body either anteriorly or posteriorly or both [11, 12]. T1- weighted images of the spine typically show decreased signal within the affected vertebral bodies, loss of disc height, and paraspinal soft-tissue collection. The presence of a thick rim of enhancement around paraspinal and intraosseous abscesses is reported to be diagnostic of TB spondylitis [13]. MRI findings of 24 patients were evaluated by Huang et al. [14] in patients with infectious spondylitis. Contagious multi-level involvement was noted only in patients with tuberculous spondylitis, as in our case. Fifteen of the 24 patients under study had SEA in the Huang’s series. SEA is a severe complication of spinal TB that requires urgent neurosurgical intervention (laminectomy), combined with specific antituberculous therapy. This is the treatment of choice to avoid neurological sequel [15]. Decompression surgery is advised for diagnostic and therapeutic purposes [1, 3]. Surgical decompression is indicated in cases with presence of pressure symptoms, failure of medical management to control the disease process, cases with spinal instability, and the need to obtain diagnostic tissue in doubtful cases [1, 3, 16]. In general, the goals of treatment in such cases include disease eradication, pain relief, preservation of neurological function, and spinal stability. In our cases, laminectomy and release of collection was done for diagnosis, pain relief and for the improvement of neurological status.
Tuberculous thoracolumbar epidural abscess is a rare entity. It should be diagnosed early and treated promptly for good outcome. MRI is the initial modality of investigation. Laminectomy and decompression has proven to be good option for confirmation of diagnosis and treatment. Delay in treatment may cause lifelong neurological deficit and vegetative state. Patient may develop spondylodiscitis or spondylitis postoperatively. Hence, patient should be followed up for a long period.
Patient with neurological symptoms with background of fever should be suspected for SEA of mycobacterial origin and evaluated with MRI. Unilateral liminectomy of the involved spine and decompression helps in both diagnosis and treatment. Anti-TB drugs remain the main modality of treatment after confirmation of diagnosis.
References
- 1.Tuli SM. Tuberculosis of spine. In: Tuberculosis of Skeleted, System. 3rd ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2004. p. 191-343. [Google Scholar]
- 2.Smith C, Crawford CH III, Dimar J. Spinal epidural abscess: A review of diagnosis and treatment. Curr Orthop Pract 2014;25:29-33. [Google Scholar]
- 3.Rasouli MR, Mirkoohi M, Vaccaro AR, Yarandi KK, Rahimi-Movaghar V. Spinal tuberculosis: Diagnosis and management. Asian Spine J 2012;6:294-308. [Google Scholar]
- 4.Tali ET. Spinal infec tions. Eur J Radiol 2004;50:120-33. [Google Scholar]
- 5.Hasan GA, Kani SM, Alqatub A. Tuberculous lumbar spinal epidural abscess in a young adult (case report). SICOT J 2018;4:5. [Google Scholar]
- 6.Arora S, Kumar R. Tubercular spinal epidural abscess involving the dorsal-lumbar-sacral region without osseous involvement. J Infect Dev Ctries 2011;5:544-9. [Google Scholar]
- 7.Prasad H, Murthy PV, Murahari P, Kumar LM, Subbaiah GP, Chandrashekhar C, et al. Tuberculous spinal epidural abscess without osseous involvement: A report of two cases. J Clin Sci Res 2017;6:117-20. [Google Scholar]
- 8.Prakash A, Kubba S, Singh N, Garg D, Pathania A, Makhija A, et al. Tuberculous epidural abscess-an unusual presentation. Indian J Tuberc 2004;51:157-8. [Google Scholar]
- 9.Pareyson D, Savoiardo M, D’Incerti L, Sghirlanzoni A. Spinal epidural abscess complicating tuberculous spondylitis. Ital J Neurol Sci 1995;16:321-5. [Google Scholar]
- 10.Kumar A, Singh AK, Badole CM, Patond KR. Tubercular epidural abscess in children: Report of two cases. Indian J Tuberc 2009;56:217-9. [Google Scholar]
- 11.Moorthy S, Prabhu NK. Spectrum of MR imaging findings in spinal tuberculosis. AJR Am J Roentgenol 2002;179:979-83. [Google Scholar]
- 12.Smith AS, Weinstein MA, Mizushima A, Coughlin B, Hayden SP, Lakin MM, et al. MR imaging characteristics of tuberculous spondylitis vs vertebral osteomyelitis. AJR Am J Roentgenol 1989;153:399-405. [Google Scholar]
- 13.Sharif HS. Role of MR imaging in the management of spinal infections. AJR Am J Roentgenol 1992;158:1333-45. [Google Scholar]
- 14.Huang YC, Shih TT, Huang KM, Su CT. Infectious spondylitis: MRI characteristics. J Formos Med Assoc 1996;95:458-63. [Google Scholar]
- 15.Metta H, Corti H, Redini L, Yampolsky C, Schtirbu R. Spinal epidural abscess due to Mycobacterium tuberculosis in a patient with AIDS: Case report and review of the literature. Braz J Infect Dis 2006;10:146-8. [Google Scholar]
- 16.Pande KC, Babulkar SS. At y pical spinal tuberculosis. Clin Orthop Relat Res 2002;398:67-73. [Google Scholar]