Management of an enchondroma found in weight-bearing sites such as the epi-metaphyseal region of the tibia done by curettage, allograft impaction, and augmentation by a PEEK plate gives excellent functional, clinical and radiological results and can be considered as a viable treatment modality.
Dr. Amyn M Rajani, Department of Orthopaedics, OAKS Clinic, Mumbai, Maharashtra, India. E-mail: dramrajani@gmail.com
Introduction: Enchondroma is a common bone tumor; however, its location in the proximal epi-metaphyseal region of the tibia is a rare finding. Its management is complicated by the weight-bearing nature of the site and despite an array of available treatment modalities in the literature, there is no fixed consensus.
Case Report: Through this case, we report a 60-year-old female who was evaluated for bilateral knee osteoarthritis. On plain radiography, a lytic lesion was noted which on CT guided biopsy was confirmed to be an enchondroma of the right proximal tibia. The patient underwent extensive curettage, allograft impaction, and supplementary fixation by a poly ethyl ether ketone plate. Following a period of immobilization, she was able to walk full weight-bearing after 3 weeks of the surgery and carry out her daily activities at 2 months. At 1 year postoperatively, the patient achieved excellent clinical, radiological, and functional outcomes without any complications.
Conclusion: Management of an enchondroma in weight-bearing regions of long bones can pose multiple challenges. Timely diagnosis and management by thorough curettage, uncompromised allograft impaction, and supplementary fixation by a PEEK plate give excellent short-term and long-term results.
Keywords: Enchondroma, tibia, allograft, graft, plating, curettage, PEEK plate.
Enchondroma is commonly an incidental finding. It is a benign neoplasm with mature hyaline cartilage. Enchondroma is one of the most common osseous neoplasms, representing 12–24% of all benign bone tumors and 3–10% of all bone tumors [1, 2]. The symptoms are often non-specific and found as a result of a pathologic fracture/trauma or localized versus radiating pain. Consequently, most of them are discovered incidentally through radiographic imaging [3]. Enchondromas typically appear as well-defined solitary defects in the metaphyseal region of long bones. Their appearance depends heavily on the location and extent of calcification of the tumor. Centrally located lesions usually appear as well-circumscribed areas of rarefaction, most frequently diaphyseal, and with an expanded cortex around it. Juxtacortical lesions are eccentric and beneath the periosteum, in well-defined cortical defects. Small, flocculent foci of calcification are generally visible within the tumor [4]. Treatment modalities vary from wait and watch to surgical intervention in the form of curettage, with or without augmentation using biologics or synthetics [5]. We provide a case for curettage and augmentation along with supplementary fixation for a female patient with an enchondroma in the proximal tibia through this report.
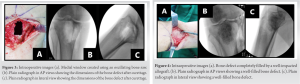
A 60-year-old female patient presented to the clinic with complaints of bilateral knee pain, difficulty in walking, and sitting cross-legged for the past 6 months. Based on the history and complaints, the patient was primarily assessed for arthritic changes in the knee joint. However, on examination, the patient had pain which was out of proportion to the arthritic changes around the right knee joint. On thorough examination, a pin-pointed, localized tenderness was elicited on the anterior portion of the right proximal tibia. The patient was advised radiographs of the knee in routine anteroposterior and lateral views. The radiographs showed a lytic lesion in the epi-metaphyseal region of the right proximal tibial. It showed rarefaction with a well-defined boundary around it (Fig. 1). The finding was corroborated by magnetic resonance imaging, which suggested it to be an enchondroma (Fig. 2) involving the epi-metaphyseal region without articular extension, thereby sparing the articular cartilage. The patient was then advised to undergo a CT-guided biopsy of the lesion. On biopsy, the lesion was diagnosed as an enchondroma of the right proximal tibia. Considering that it was a solitary enchondroma and was symptomatic, the patient was taken up for surgery. Using a medial incision, pes anserine bursa was incised and lifted subperiosteally. By creating a medial window using a drill and an oscillating saw, the lesion was thoroughly scooped out and the sample was sent for histopathological biopsy (Fig. 3). On confirming adequate clearance of the lesion by fluoroscopy, the void was filled with allograft (Fig. 4). On adequate compaction of the cancellous allograft, a three-hole polyether ether ketone (PEEK) plate was applied for supplementary fixation (Fig. 5).
The skin was closed in layers and the patient was mobilized with walker-assisted non-weight bearing walking in the aftermath. At 3 weeks, the patient was then mobilized full weight-bearing without aid. At 2 months follow-up, the patient was able to carry out all her activities of daily living.
On clinical examination at 12 months follow-up, the patient had a full range of motion of the knee joint and a well-healed scar and was completely pain-free at the site of the lesion. On functional outcome assessment at 12 months, the international knee documentation committee (IKDC) score was 78/87 (89.7%) and the Tegner Lysholm score was 92/100, both falling within the excellent range. The radiographs suggested complete consolidation of bone graft, suggesting a well-healed lesion (Fig. 6).
Enchondroma is a benign, slow-growing tumor, composed of hyaline cartilage cells that persist throughout development. It is the most common primary bone tumor of the hand. It is also commonly seen in the diaphysis of long bones such as the humerus and tibia [5, 6]. In our case, it was a proximal epi-metaphyseal region lesion which is a notably rare presentation. This lesion was exactly under the subchondral surface of the tibial plateau. Normally, such lesions when present in the diaphyseal region are not susceptible to collapse and consequently, are asymptomatic. In such rare cases, the patient requires surgical intervention if there are symptoms in the form of pain, difficulty in walking, or difficulty in carrying out activities of daily living. Fractures associated with these benign lesions may be allowed to heal before definitive treatment of the tumor. However, surgical intervention is inevitable if the lesion is symptomatic, avoids complications, and allows early mobilization [7, 8]. In our case, the size and location of the lesion warranted a curettage and allograft impaction. Since the lesion was in the epi-metaphyseal region, the subchondral bone was bare on curettage and the defect required supplementation of the impacted allograft in the form of a plate and subchondral screws. There is no standardized algorithm for surgical treatment of this kind of tumor. It is not clear whether grafting after curettage is necessary, or whether the type of graft used affects healing, recurrence, complications, and malignant transformation [5, 9, 10]. In our case, on extensive curettage of the lesion, impaction bone grafting was done using allograft until a compact filling of the bone defect was achieved. After doing so, supplementary augmentation was done using a PEEK plate for its excellent biocompatibility, biostability, high tensile strength, and compatibility with other incorporated biomaterials [11]. There is no categorical functional outcome grading for surgical management of enchondroma. Hence, the functional outcome was evaluated as per the region operated. On functional outcome assessment at 12 months, the IKDC score was 78/87 (89.7%) and the Tegner Lysholm score was 92/100, both falling within the excellent range. Considering the presence of radiological and clinical signs of consolidation of the impacted allograft and no recurrence of the lesion even after a year, the patient was advised removal of the PEEK plate.
Enchondroma is a slow growing tumor, which often makes it an incidental finding due to its non-aggressive nature. When detected in uncommon locations and more so if these include the anatomical sites along the weight-bearing axis, the prognosis can rapidly worsen and even cause pathological fractures. It is best to manage such tumors by curettage, allograft impaction, and augmentation by a PEEK plate and was done in our case.
Management of an enchondroma found in weight-bearing sites such as the epi-metaphyseal region of the tibia done by curettage, allograft impaction, and augmentation by a PEEK plate gives excellent functional, clinical, and radiological results and can be considered as a viable treatment modality.
References
- 1.Dorfman DD, Bogdan C. Bone Tumors. St. Louis, MO: Mosby; 1998. p. 253-76. [Google Scholar]
- 2.Unni KK, Inwards CY, Bridge JA, Kindblom LG, Wold LE. AFIP Atlas of Tumor Pathology Series 4: Tumors of the Bones and Joints. Silver Spring, MD: ARP Press; 2005. p. 46-52. [Google Scholar]
- 3.Yildiz C, Erler K, Atesalp AS, Basbozkurt M. Benign bone tumors in children. Curr Opin Pediatr 2003;15:58-67. [Google Scholar]
- 4.Biondi NL, Varacallo M. Enchondroma. In: StatPearls. Treasure Island: StatPearls Publishing; 2022. [Google Scholar]
- 5.Bachoura A, Rice IS, Lubahn AR, Lubahn JD. The surgical management of hand enchondroma without post curettage void augmentation: Authors’ experience and a systematic review. Hand (N Y) 2015;10:461-71. [Google Scholar]
- 6.Yalcinkaya M, Akman YE, Bagatur AE. Recurrent metacarpal enchondroma treated with strut allograft: 14-year follow-up. Orthopedics 2015;38:e647-50. [Google Scholar]
- 7.Haase SC. Treatment of pathologic fractures. Hand Clin 2013;29:579-84. [Google Scholar]
- 8.Choy WS, Kim KJ, Lee SK, Yang DS, Jeung SW, Choi HG, et al. Surgical treatment of pathological fractures occurring at the proximal femur. Yonsei Med J 2015;56:460-5. [Google Scholar]
- 9.Sridhar H, Vijaya M, Clement W, Srinivas C. Chondrosarcoma arising in an enchondroma of the metacarpal bone-a case report. J Clin Diagn Res 2014;8:142-3. [Google Scholar]
- 10.Culver JE Jr., Sweet DE, McCue FC. Chondrosarcoma of the hand arising from a pre-existent benign solitary enchondroma. Clin Orthop Relat Res 1975;128-31. [Google Scholar]
- 11.Zhou K, He X, Tao X, Pan F, Yang H. A biomechanical matched-pair comparison of two different locking plates for tibial diaphyseal comminuted fracture: Carbon fiber-reinforced poly-ether-ether-ketone (CF-PEEK) versus titanium plates. J Orthop Surg Res 2020;15:558. [Google Scholar]