Novel method of patellar resurfacing in TKA for egg-shell patellar defect in single stage.
Dr. Hiroshi Fujii, Department of Orthopaedic Surgery, Ogori Daiichi General Hospital, Yamaguchi, Japan. E-mail: hfjii@ogoridaiichi.jp
Introduction: Patellofemoral biomechanics are a very critical factor for patient satisfaction after total knee arthroplasty. Patellar defects in a primary total knee arthroplasty are rare. We present a rare case of valgus deformed knee with an eroded egg-shell like patella managed with primary knee arthroplasty.
Case Report: A 58-year-old female with bilateral knee pain for 35-years presented to us with a bilateral valgus knee. The knee range of movement was restricted more on the left side and severely restricting her activities of daily living. She had an egg-shell like eroded patellar defect in an osteoarthritic knee for which, she underwent primary total knee arthroplasty and patellar resurfacing with autologous bone graft harvested from the tibial cut bone.
Conclusion: We have presented a rare case of a combination of patellar defect in an Osteoarthritic knee which was managed by modified gap-balancing technique of TKA with a novel method of patellar resurfacing in a single stage with good functional results at 1-year postoperatively. This case improves our understanding of the management of such complex scenarios and, more importantly raises the questions our understanding and need of classification of such patellar defects in a primary arthritic knee.
Keywords: Shell patella, bone graft, single-stage, primary arthroplasty, resurfacing.
Osteoarthritis is a leading cause of pain and disability affecting all the three compartments of the knee. The patellofemoral joint is a complex articulation and a very critical factor for patient satisfaction after total knee arthroplasty [1]. Almost 25.7% of the causes of the first revision TKA are due to patellofemoral problem [2]. Management of defective patella with altered morphology is challenging and is more commonly encountered in revision surgeries [3]. Extensor mechanism impairment and anterior knee pain are often the sequelae in patients with patellar defects who undergo resurfacing during revision TKA [4]. The literature available for management of patellar defect in primary TKA is limited. The patellar defect encountered in a primary TKA is commonly a sequelae of patella-femoral malalignment which needs to be addressed, unlike those in revision arthroplasty where the patellar defect is usually the sequelae of implant removal [5]. Here, we present a novel surgical management of egg-shell patellar defect in primary knee arthroplasty. The patient displayed a good range of motion with no complaints and an intact extensor mechanism performing activities of daily living at 1-year follow-up. The patient was informed that the data concerning the case would be submitted for publication, and she provided consent.
History and radiographic findings
A 58-year-old female presented to our hospital with complain of bilateral knee pain with the left side worser. The patient experienced progressively worsening pain on weight-bearing activities. The pain gradually increased over the course of 35 years to the present state, with the inability to perform her activities of daily living. She had history of more than one episode of patellar dislocation in her left knee during her junior school when she was 14 years old, which was treated conservatively. She had no associated complains of other joint involvement and no family history of rheumatoid arthritis. On clinical examination, both her knees were markedly tender and effused, with the left side being more symptomatic. The knee range of motion was severely restricted on the left side with a movement arc of 35–100° compared to the right side of 10–100°. Patellofemoral crepitus was felt throughout the range of motion. Pre-operative knee society score (KSS) was 25 on bilateral sides, quality of life assessed using japan knee osteoarthritis measure (QOL-JKOM) was 68 and visual analog scale pain scale (VAS)-8 on the left side [6]. The clinical and radiological examination of Hip and Spine was normal with bilateral Hallux Valgus noted in the foot. The patient was evaluated for inflammatory arthropathy with the inflammatory blood parameters and RF factor in the normal range.
Osteoarthritis was Kellgren-Lawrence Grade 4 with a concave shaped patella on radiological evaluation and the femoral-tibial axis was 166° with a Q-angle of 13° (Fig. 1). The patella was thickest at 12 mm superomedially and thinnest at 5 mm centrally on computed tomography (CT) imaging (Fig. 2).
Operative and post-operative course
The knee was exposed using a midline incision followed by a medial parapatellar arthrotomy (Fig. 3). On everting the patella, an egg-shell like morphology devoid of cartilage cover was found. After the bone cut of distal femur and proximal tibia, the posterior condyle of the femur was cut using by the modified gap balancing technique. An autologous cortical bone was harvested from proximal tibial cut and preserved for bone grafting. Using the ROM/Self adjustment method, the unsecured tibial tray could seek its own rotation on the cut surface of proximal tibia with the femoral trial, patella relocated with trail in-situ and medial arthrotomy held by three tissue clamps followed by flexion/extension cycling movements of the knee [7]. The rotational axis was marked on the proximal bone cut surface of tibia and was confirmed more externally rotated compared to the previously drawn Akagi’s line [8] (Fig. 4).
Then, the autologous bone from proximal tibia was reshaped to match the patellar defect (Fig. 5). The graft was inlaid in the defect after curetting the surface of cartilage and augmented with three cortical cannulated screws of 16 mm to the patella. The final thickness of the patella after grafting was 16 mm on which a 32 mm size, 8.5 mm thick patellar button trial implanted after strategically placing the peg holes based on pre-operative planning by the Zedknee system (LEXI, Tokyo, Japan). The patellar tracking was reconfirmed with passive flexion and extension of the knee joint after temporarily fixing the tibial trial component as per the previously determined axis without lateral release. Cemented posterior stabilized TKA (Zimmer Persona) was implanted with tibial component orientation based on the ROM/Self-adjustment method. The patella was resurfaced with a 32 mm button with cement in strategically placed peg holes avoiding the screws. The patient received compression stockings, mechanical calf pumps, and enoxaparin as once a day for post-operative thromboprophylaxis. She underwent the same post-operative physiotherapy protocol as other TKA patients in the institution. Continuous passive motion from 0° to 60° was started on the day of operation followed by 0° to 90° on post-operative day (POD) 1, and then 0° to maximal flexion as tolerated from POD 2 onward. Full weight bearing was allowed immediately postoperatively. At 1-year postoperatively, her KSS functional score improved to 90 and QOL-JKOM improved to 8. Her VAS pain score reduced to 0 and she could return to her work. The quadriceps strength and knee range of movement improved drastically with an arc of 0–135° of flexion with no patellofemoral crepitus. At 1-year, the patient could kneel and squat without pain with radiographs revealing no loosening (Fig. 6). Follow-up CT at 1-year revealed consolidation of the bone graft with maintained patellar thickness and freely able to perform kneeling activities (Fig. 7).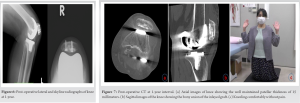
Patellar resurfacing in defective patella undergoing revision total knee arthroplasty has been well reported in the literature, but management of patellar defects in primary knee arthroplasty is rare. We believe our report to be one of the earliest, to the best of our knowledge, highlighting a novel approach for the management of patellar shell-like defect in primary arthroplasty. Abdel et al. showed satisfactory results and good bone resorption in revision TKA using autologous bone graft harvested from box cuts of femur to fill patellar cavitary defects [4]. We used the similar principle of using autologous bone graft harvested from the proximal tibial cut for filling the patellar cavitary defect. Unlike Abdel et al., we secured the graft using screws, which we believe would not only prevent the future collapse of construct due to resorption/remodeling but also secure the graft allowing early ROM of knee [4, 9]. At 1-year follow-up on CT imaging, the patellar thickness was be well maintained. A thin patella before resurfacing has an increased risk of fracture and osteonecrosis which has a disastrous effect with potentially long-standing disability for the patient [8]. A remnant of at least 12 mm is suggested to be ideal, regardless of the initial thickness to prevent patellar complications [10, 11]. Thus, we achieved a patellar thickness of 16 mm with adequate bone stock for patellar prosthesis, of reasonable thickness, and above the fracture risk threshold [12, 13]. In addition, restoring the patellar thickness post-resurfacing is critical for the quadriceps lever arm mechanism and a thickness of 20 mm and more is suggested to be ideal [4]. In our case, the final patellar thickness after resurfacing was 24.5 mm. We recommend further resection of patella if the flexion of knee is restricted, but it was not so in our case. An increased post-patellar thickness also improves the overall function in activities of high demand like negotiating stairs; hence, we believe it to be one of the reasons for a drastically improved post-operative functional score [10]. The ROM/self-adjustment method was a key step in identifying the ideal tibial axis for patellofemoral tracking due to varying anatomical landmarks in patients with patellofemoral dysplasia [7]. The tibial axis determined by ROM/self-adjustment method is primarily depends on the femoral component rotation and is considered being relevant only if adapted to each patient, which in our case was patient specific anatomy based on pre-operative CT-based planning [7]. The tibial component was noted to be more externally rotated compared to the Akagi’s line, which is in lieu of the increased external rotation in relation to native tibia seen in valgus knee [7]. Thus, a detailed patient specific pre-operative evaluation is essential in valgus deformity knee. We believe, the externally rotated alignment in this patient also improved our clinical outcome and results, including the patient’s ability to kneel without pain [14, 15]. The aim of patellar resurfacing is not only to relieve anterior knee pain but also to restore normal patellofemoral mechanics [10]. Restored patellofemoral mechanics are important for activities of high demand such as squatting, stairs ascent, and descent, thus patellar resurfacing was very crucial in our patient considering her younger age and higher demands.
We have presented a rare case of a combination of patellar defect in an osteoarthritic knee which was managed by modified gap-balancing technique of TKA with a novel method of patellar resurfacing in a single stage with good functional results at 1-year postoperatively. This case improves our understanding of management of such complex scenarios and more importantly raises the questions our understanding and need of classification of such patellar defects in a primary arthritic knee.
Egg-shell patellar defect in a primary total knee arthroplasty is a very rare entity which can be managed by filling the patellar defect with autologous proximal tibial bone graft augmented by screws. Defective patellar reconstruction with a hybrid construct of bone cement-bone graft augmented by screws is a viable option which restores the patellafemoral biomechanics and improves the functional outcome in primary total knee arthroplasty.
References
- 1.Bengs BC, Scott RD. The effect of patellar thickness on intraoperative knee flexion and patellar tracking in total knee arthroplasty. J Arthroplasty 2006;21:650-5. [Google Scholar]
- 2.Mathis DT, Lohrer L, Amsler F, Hirschmann MT. Reasons for failure in primary total knee arthroplasty-an analysis of prospectively collected registry data. J Orthop 2020;23:60-6. [Google Scholar]
- 3.Tetreault MW, Gross CE, Yi PH, Bohl DD, Sporer SM, Valle CJ. A classification-based approach to the patella in revision total knee arthroplasty. Arthroplast Today 2017;3:264-8. [Google Scholar]
- 4.Abdel MP, Petis SM, Taunton MJ, Perry KI, Lewallen DG, Hanssen AD. Long-term results of patellar bone-grafting for severe patellar bone loss during revision total knee arthroplasty. J Bone Joint Surg Am 2019;101:1636-44. [Google Scholar]
- 5.Macri EM, Felson DT, Zhang Y, Guermazi A, Roemer FW, Crossley KM, et al. Patellofemoral morphology and alignment: Reference values and dose-response patterns for the relation to MRI features of patellofemoral osteoarthritis. Osteoarthritis Cartilage 2017;25:1690-7. [Google Scholar]
- 6.Akai M, Doi T, Fujino K, Iwaya T, Kurosawa H, Nasu T. An outcome measure for Japanese people with knee osteoarthritis. J Rheumatol 2005;32:1524-32. [Google Scholar]
- 7.Berhouet J, Beaufils P, Boisrenoult P, Frasca D, Pujol N. Rotational positioning of the tibial tray in total knee arthroplasty: A CT evaluation. Orthop Traumatol Surg Res 2011;97:699-704. [Google Scholar]
- 8.Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C. An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 2004;420:213-9. [Google Scholar]
- 9.McPherson EJ, Sherif SM, Dipane MV, Arshi A. Patellar rebar augmentation in revision total knee arthroplasty. J Arthroplasty 2021;36:670-5. [Google Scholar]
- 10.Hamilton WG, Ammeen DJ, Parks NL, Goyal N, Engh GA, Engh CA Jr. Patellar cut and composite thickness: The influence on postoperative motion and complications in total knee arthroplasty. J Arthroplasty 2017;32:1803-7. [Google Scholar]
- 11.Putman S, Boureau F, Girard J, Migaud H, Pasquier G. Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res 2019;105:S43-51. [Google Scholar]
- 12.Parke EA, Nakasone CK, Andrews SN, Wright AR, Stickley CD. The effect of patellar thickness on gait biomechanics following total knee arthroplasty. Knee 2019;26:1354-9. [Google Scholar]
- 13.Garcia RM, Kraay MJ, Conroy-Smith PA, Goldberg VM. Management of the deficient patella in revision total knee arthroplasty. Clin Orthop Relat Res 2008;466:2790-7. [Google Scholar]
- 14.Nakamura S, Shima K, Kuriyama S, Nishitani K, Ito H, Matsuda S. Tibial tubercle-trochlear groove distance influences patellar tilt after total knee arthroplasty. J Arthroplasty 2019;34:3080-7. [Google Scholar]
- 15.Steinbrück A, Schröder C, Woiczinski M, Müller T, Müller PE, Jansson V, et al. Influence of tibial rotation in total knee arthroplasty on knee kinematics and retropatellar pressure: An in vitro study. Knee Surg Sports Traumatol Arthrosc 2016;24:2395-401. [Google Scholar]











