Perilunate injuries should be examined for every head injury patient as it's often missed.
Dr. Jimmy Joseph Meleppuram, Department of Orthopaedics, Centre of excellence in Orthopaedics and Rheumatology, Aster Medcity Hospital, Kochi, Kerala, India. E-mail: jimmyjoseph939@gmail.com
Introduction: Perilunate injuries are rare, complex, and high velocity trauma associated injuries accounting to <10% of wrist joint trauma. Volar peri-lunate dislocations account for <3% of these injuries. Perilunate injuries should, therefore, be focused and ruled out while examining a patient complaining wrist pain after high-energy accidents which are often missed.
Case Report: We report a case of, missed dislocation in a patient who presented delayed with wrist pain, post 4 months road traffic accident associated with heterotrophic ossified mass in a united scapular fracture. He underwent open reduction through a combined approach and internal fixation with K-wires. Aggressive wrist physiotherapy retrieved near-normal range of motion at the wrist by the end of 5 months as well as neither revealed recurrence of the dislocation nor signs of avascular necrosis.
Conclusion: Successful results in perilunate injuries can be obtained with open reduction, ligament reconstruction with K-wires fixation through a single combined approach in delayed presentation resulting in achieving near normal range of movements.
Keywords: Perilunate dislocation, carpal injuries, neglected wrist injuries, dorsal-volar approach.
Perilunate dislocations can be envisioned as a primary missed important differential diagnosis in patients with history of high velocity wrist trauma [1,2]. Either due to delay in presentation, poor quality of radiographs or due to associated injuries that require more indeferrible attention; nearly 25% of perilunate injuries are diagnosed belatedly [3]. The anticipated risk of avascular necrosis of lunate, scaphoid, and secondary osteoarthritis can be waived off by accurate diagnosis and prompt treatment.
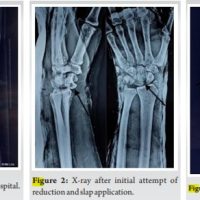
A 42-year-old gentleman presented to our department with difficulty to lift his right shoulder completely, after being initially treated for massive head injury and right scapular fracture post road traffic accident elsewhere past four months. His spouse noticed an un-resolving swelling in the left wrist associated with pain affecting his activity of daily living, in spite being recouped from head injury and was stressed for the same. On examination, he had non-tender bony prominence over the right scapula, passive shoulder abduction with forward flexion was restricted to 90°, nil neurovascular deficit, left wrist depicted to have swelling, diffuse tenderness over the carpal bones with severe restriction of movements’, and intact distal neurovascular status. Although he had delayed coherence, his pre-operative DASH and PRWE score was, respectively, 95/100 and 99/100 (poor) at the initial presentation. Standard roentgenogram of the shoulder revealed, a huge intra-communicating (toward clavicular and infrascapular territory) heterotrophic ossified mass at supra scapular region for a united scapular fracture; wrist depicted Mayfields Type IV perilunate dislocation with classical lunotriquetral disruption; and spilled tea cup sign in the conventional views (Fig. 1). 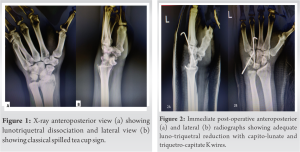 The patient underwent heterotrophic mass excision through a bra strap approach for the right shoulder. A combined dorsal (between third and fourth extensor compartment) and volar approach was utilized for the left wrist, intraoperatively, the lunate was found to be dislocated from the fossa with volar lunotriquetral ligament severed with its intact dorsal counterpart. Palmaris longus tendon graft was harvested utilizing the volar access, perilunate dislocation was reduced, graft was incorporated from triquetrum to lunate, suture tied after pilot hole drilled lateral to medial through and through, stabilized by a K wire through triquetro-capitate and capitolunate junction, confirmed by C arm, dorsal capsule tightly closed, and joint immobilized in below elbow slab (Fig. 2). Immediate post-operative X-rays showed satisfactory reduction, sutures removed after 2 weeks, K wire and slab removed after 4 weeks, aggressive wrist physiotherapy initiated. The patient was regularly followed up and he regained near-normal full range of motions at the wrist by the term of 5months (Fig. 3) and neither revealed recurrence of the dislocation nor early signs of avascular necrosis or osteoarthritis (Fig. 4). At 6 months his DASH and PRWE scores are 8.3/100 and 20/100, respectively, and further follow-up was unable as patient went to his workplace abroad.
The patient underwent heterotrophic mass excision through a bra strap approach for the right shoulder. A combined dorsal (between third and fourth extensor compartment) and volar approach was utilized for the left wrist, intraoperatively, the lunate was found to be dislocated from the fossa with volar lunotriquetral ligament severed with its intact dorsal counterpart. Palmaris longus tendon graft was harvested utilizing the volar access, perilunate dislocation was reduced, graft was incorporated from triquetrum to lunate, suture tied after pilot hole drilled lateral to medial through and through, stabilized by a K wire through triquetro-capitate and capitolunate junction, confirmed by C arm, dorsal capsule tightly closed, and joint immobilized in below elbow slab (Fig. 2). Immediate post-operative X-rays showed satisfactory reduction, sutures removed after 2 weeks, K wire and slab removed after 4 weeks, aggressive wrist physiotherapy initiated. The patient was regularly followed up and he regained near-normal full range of motions at the wrist by the term of 5months (Fig. 3) and neither revealed recurrence of the dislocation nor early signs of avascular necrosis or osteoarthritis (Fig. 4). At 6 months his DASH and PRWE scores are 8.3/100 and 20/100, respectively, and further follow-up was unable as patient went to his workplace abroad.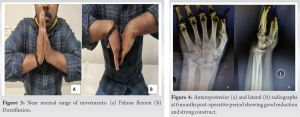
Perilunate injuries are rare, complex, and high velocity trauma associated injuries occurring in <10% of trauma around the wrist joint. Volar peri-lunate dislocations (VPLDs) account for <3% of perilunate injuries [1,2]. Up to 25% of perilunate injuries are diagnosed later on, either due to time lag in presentation, poor quality of radiographs, or due to associated injuries that require more indefeasible attention [3]. Literature basically suggests two mechanism resulting in VPLDs. Aitken and Nalebuff proposes, the most common mechanism of having a VPLD injury is, fall onto a hyperextended wrist with or without the forearm in supination, on the counterpart, by Green and O’briens theory explained a fall onto a hyper-extended wrist with the forearm supinated led to a pure dislocation, whereas, without forearm supination caused a fracture dislocation [4,5]. They explicated this inference from a dissected carpus of one of the patients who had died as a result of other injuries in their study. Literature deny support on any published evidence that conservative treatment, which consists of closed reduction maneuvers along with cast immobilization, is optimal for managing perilunate dislocation [6]. Some studies proves chances of dislocation recurs in about 59% of patients managed conservatively [ 7 ]. Misdiagnosed perilunate dislocation carries various complications; predominantly among these are intraoperatively due to essential fibrosis and scarring, uncertainty of full range of function post reduction, and possibility of evolving avascular necrosis of the reduced lunate postoperatively. There is always a chance for mid-carpal arthritis as well as median nerve injury found to occur in late cases [8]. Early identification of these injuries can be warranted by proper clinical history associated with anticipatory physical examination. Deliberate scrutiny of radiographs is mandatory with importance to the Gilula’s arc of the carpal joints, scapholunate interval, scaphocapitate, and capitolunate angles. The classical radiographic appearances of a perilunate dislocation present breakage of the proximal and distal configuration of the proximal carpal rows. On the lateral view, the lunate do not articulate with the head of the capitate, but displays volarly rotated, the characteristic “spilled teapot sign.” Computed tomography (CT) scan with 3D reconstruction films is helpful in validating the diagnosis. Bagheri et al. found early surgical correction of these injuries results in a better functional yield as matched to conservative line of management in their study [9]. Widely been advocated for the management of these injuries are the combined dorsal and volar surgical approach to the wrist joint [10]. Our approach helped us to visualize the lunate bone completely within the fossa from both aspects as well as, were able t0 harvest the palmaris longus graft within same incision for tying the graft to stabilize the triquetro-lunate construct further stabilized by a k wire compared to other various implants such as compression screws and cerclage wires after reduction. Adequate periodic follow-up is important to prevent reoccurrence of carpal instability and other complications mentioned previously. Our patient had a significantly improved DASH and PRWE scores on regular follow-up at 6 months.
Perilunate injuries should therefore be focused and ruled out while examining a patient complaining wrist pain after high-energy accidents. An apt radiograph taken incorrect technique supplemented with 3D CT scan films adds to the confirmation. The best results can be achieved with open reduction, meticulous ligament reconstruction, and internal fixation with K-wires through a combined approach by ample visualization of the carpus thereby creating a rigid construct in cases of delayed presentation.
Diagnosing perilunate injuries are of utmost importance in a high velocity injury patient. Even though often missed, delayed presentation of such cases can be well treated with our methodology of surgical practice followed in this case.
References
- 1.Dobyns JH, Linschield RL. Fractures in Adults. 2nd ed. Philadelphia, PA: JB Lippincott; 1984. p. 411-509. [Google Scholar]
- 2.Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res 1987;214:136-47. [Google Scholar]
- 3.Kailu L, Zhou X, Fuguo H. Chronic perilunate dislocations treated with open reduction and internal fixation: Results of medium-term follow-up. Int Orthop 2010;34:1315-20. [Google Scholar]
- 4.Aitken AP, Nalebuff EA. Volar transnavicular perilunar dislocation of the carpus. J Bone Joint Surg Am 1960;42-A:1051-7. [Google Scholar]
- 5.Niazi TB. Volar perilunate dislocation of the carpus: A case report and elucidation of its mechanism of occurrence. Injury 1996;27:209-11. [Google Scholar]
- 6.Apergis E, Maris J, Theodoratos G, Pavlakis D, Antoniou N. Perilunate dislocations and fracture-dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand Suppl 1997;275:55-9. [Google Scholar]
- 7.Adkison JW, Chapman MW. Treatment of acute lunate and perilunate dislocations. Clin Orthop Relat Res 1982;164:199-207. [Google Scholar]
- 8.Dhillon MS, Prabhakar S, Bali K, Chouhan D, Kumar V. Functional outcome of neglected perilunate dislocations treated with open reduction and internal fixation. Indian J Orthop 2011;45:427-31. [Google Scholar]
- 9.Bagheri F, Taraz-Jamshidi MH, Birjandinejad A, Sharifi-Daloei SR, Mirkazemi M, Choghadeh MF, et al. Trans-scaphoid perilunate fracture-dislocation and isolated perilunate dislocations; Surgical versus non surgical treatment. Arch Bone Jt Surg 2013;1:74-7. [Google Scholar]
- 10.Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am 2004;29:412-7. [Google Scholar]