Patients and doctors should be aware of the recurrence chances in giant cell tumor of distal radius, realizing it as an important complication and taking the required steps for the same
Dr. Amar Kamat, Department of Orthopedic Oncology, HealthCare Global, Bengaluru, Karnataka, India. E-mail: dramar.kamat@gmail.com
Introduction: Distal radius is known to have high percentage of recurrences in giant cell tumor (GCT) despite best efforts. We would like to present a case where the recurrence unusually occurred in the graft and the complications associated with it.
Case Report: A 45-year-old woman, who had previously undergone curettage of GCT distal radius, presented with recurrence of lesion which was managed initially with resection and non-vascularized fibular autograft reconstruction. Tumor again recurred in the autografted fibula which was managed by curettage and cementing. Due to progressive collapse of the carpus, resection of the autograft and wrist arthrodesis was carried out.
Conclusion: Recurrence of GCT is a challenging problem. Wide resections may not always avoid recurrences. Patients should be made aware of the extend of recurrence that can happen in spite of the best efforts.
Keywords: Giant cell tumour, fibula, recurrence.
Giant cell tumor (GCT) of bone is an aggressive primary skeletal lesion accounting for almost 5% of all primary tumors of bone in adults. GCT is histologically a benign neoplastic lesion consisting of three cell types: Multinucleated giant cells that resemble osteoclasts, neoplastic stromal cells, and mononuclear histiocytic cells [1]. On plain X-ray film, the tumors appear as lytic lesions without matrix calcification. Tumors generally arise in the metaepiphyseal region of long bones, mostly commonly around knee, followed by distal radius. Clinically, GCT presents as a benign entity but it is most often very aggressive lesion with a tendency toward local recurrence. It is managed by many ways depending on the site and nature of the lesion. Intralesional curettage is most commonly done in metaphyseal lesions. The residual cavity may be treated with adjuvants and void filling may be done with cement or bone graft. For large lesions with significant joint involvement, wide resection with reconstruction is carried out. Reconstruction options are prosthetic replacement, allograft or autograft, and fusion. For distal radius resections, proximal fibula autograft reconstruction has been widely reported with good outcomes [2]. Depending on the local presentation of tumor and type of treatment, recurrence rates range from 0% to 65% [3, 4]. Even though aggressive nature and recurrence have been reported extensively, recurrence in an auto-grafted fibula has not been reported.
In 2010, a 45-year-old female had presented to us with recurrent right wrist fullness and pain managed surgically once 3 years before presentation to us. She had undergone curettage and bone grafting from ipsilateral iliac crest back then, but details of adjuvant treatment given to the cavity were not available. On examination, she had fullness of her right distal forearm; there was no tenderness and range of motion (ROM) of wrist was restricted. The radiograph showed expansile lytic lesion with thinned out cortices (Fig. 1). Chest computed tomography was done to rule out pulmonary metastasis. Different options of reconstruction were offered to the patient. Considering the recurrent nature of the lesion and patients desire to maintain a mobile wrist joint, a plan was made to reconstruct the distal radius with ipsilateral fibula non vascularized autograft. In late 2010, she underwent en bloc resection of the right distal radius, followed by proximal fibula harvest. Proximal fibula autograft was fixed to the remnant of the radius with a 7 hole DCP and contralateral iliac crest grafting was done at the fibuloradial junction. Wrist ligaments were reconstructed and a wrist transfixing K-wire was put for immobilization to facilitate healing of ligaments (Fig. 2).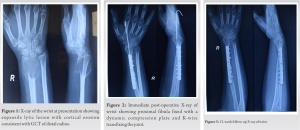

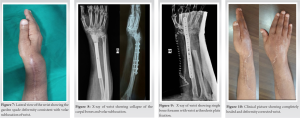
GCT is a benign bone lesion known for its very aggressive nature and recurrence. Some treatment options are available for GCT in bone, which include denosumab, radiation therapy, serial embolization, interferon, and surgical treatment [5]. Serial embolization, radiation therapy, and interferon therapy are recommended by the NCCN guidelines for the treating GCT. Besides those treatments, surgery remains the main treatment for GCT. Tumor character and the management method have been widely studied to achieve a control of recurrence. Becker et al. had found that the presence of soft-tissue component might influence the risk of local recurrence [6]. In another study, O’Donnell et al. reported that pathologic fractures at presentation were associated with higher recurrence rate [7] From management perspective, wide resections were associated with a lower risk of recurrence than intralesional curettage [8]. In intralesional curettage procedures, local adjuvants (polymethyl methacrylate, cryotherapy, hydrogen peroxide, and phenol) have been reported to improve tumor control [9]. Polymethylmethacrylate bone cement may decrease the risk of local recurrence as it can exert thermal and toxic effects on tumor cells [10]. Polymethylmethacrylate may give additional stability and hence allow for more aggressive curettage without the risk of collapse. Wide resections have been associated with lower risk of recurrence than intralesional surgery. In the present case report, recurrence was seen in spite of wide local resection and reconstruction with a fibular graft. The morbidity that such repeated surgeries cause on the mental and physical ability of a patient can not be quantified. Patient education is paramount for success of such complicated cases. Morbidity of a carpal collapse due to repeated surgeries that destabilized the ligamentous reinforcement was unanticipated. In spite of many challenges, this patient continues to have good function of her limb.
Recurrence of GCT is a challenging problem. Wide resections may not always avoid recurrences. Patients should be made aware of the extent of recurrence that can happen in spite of the best efforts.
Clinicians should be aware of these complications and methods to tackle them. A thorough curettage can avoid recurrence in such set ups.
References
- 1.Werner M. Giant cell tumour of bone : Morphological, biological and histogenetical aspects. Int Orthop 2006;30:484-9. [Google Scholar]
- 2.Saini R, Bali K, Bachhal V, Mootha AK, Dhillon MS, Gill SS. En bloc excision and autogenous fibular reconstruction for aggressive giant cell tumor of distal radius: A report of 12 cases and review of literature. J Orthop Surg Res 2011;6:14. [Google Scholar]
- 3.Balke M, Schremper L, Gebert C, Ahrens H, Streitbuerger A, Koehler G, et al. Giant cell tumor of bone: Treatment and outcome of 214 cases. J Cancer Res Clin Oncol 2008;134:969-78. [Google Scholar]
- 4.Blackley HR, Wunder JS, Davis AM, White LM, Kandel R, Bell RS. Treatment of giant-cell tumors of long bones with curettage and bone-grafting. J Bone Joint Surg Am 1999;81:811-20. [Google Scholar]
- 5.Zheng K, Wang Z, Wu SJ, Ye ZM, Xu SF, Xu M, et al. Giant cell tumor of the pelvis: A systematic review. Orthop Surg 2015;7:102-7. [Google Scholar]
- 6.Arbeitsgemeinschaft Knochentumoren; Becker WT, Dohle J, Bernd L, Braun A, Cserhati M, et al. Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy. J Bone Joint Surg Am 2008;90:1060-7. [Google Scholar]
- 7.O’Donnell RJ, Springfield DS, Motwani HK, Ready JE, Gebhardt MC, Mankin HJ. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am 1994;76:1827-33. [Google Scholar]
- 8.Errani C, Ruggieri P, Asenzio MA, Toscano A, Colangeli S, Rimondi E, et al. Giant cell tumor of the extremity: A review of 349 cases from a single institution. Cancer Treat Rev 2010;36:1-7. [Google Scholar]
- 9.Durr HR, Maier M, Jansson V, Baur A, Refior HJ. Phenol as an adjuvant for local control in the treatment of giant cell tumour of the bone. Eur J Surg Oncol 1999;25:610-8. [Google Scholar]
- 10.Kivioja AH, Blomqvist C, Hietaniemi K, Trovik C, Walloe A, Bauer HC, et al. Cement is recommended in intralesional surgery of giant cell tumors: A Scandinavian Sarcoma Group study of 294 patients followed for a median time of 5 years. Acta Orthop 2008;79:86-93. [Google Scholar]










