Rearticulation with total hip arthroplasty can significantly improve the patients’ quality of life even many decades after excision arthroplasty (Girdlestone).
Dr. Prof. Dr. med. Dr. phil. Dipl.-Ing. (FH) Andrej M. Nowakowski, Head of Department for Orthopaedics and Traumatology, Kantonsspital Baselland, 4101 Bruderholz, Switzerland. E-mail: andrej.nowakowski@ksbl.ch
Introduction: Tuberculous coxitis accounts for about 15% of all osteoarticular tuberculosis cases and is the second most common after spinal tuberculosis. In extensive cases, Girdlestone resection arthroplasty is an option for primary surgical treatment followed in the course of time, with total hip arthroplasty (THR) to increase function. However, the remaining bone stock is generally poor. In these cases, the Wagner cone stem offers good pre-conditions for bone restoration even seven decades after Girdlestone, as presented here.
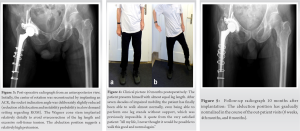
Case Report: A 76-year-old male patient was admitted to our department with a painful hip, who had previously been treated with Girdlestone at the age of 5 years after being diagnosed with tuberculous coxitis. After an intensive and very detailed evaluation of treatment options, the decision fell on rearticulating with a THR, even though primary surgery lay seven decades back. Since it was not possible to insert an appropriate non-cemented pressfit-cup, an acetabular reinforcement ring and a PE low profile cup were inserted, cemented with less inclination to avoid or reduce hip instability. A fissure around the implant (Wagner cone stem) was secured with numerous cerclages. Surgery was performed by the senior author (A.M.N.) postoperatively, the patient suffered a prolonged delirium. Ten months after surgery, the patient was satisfied with the result and reported a meaningful improvement in his daily quality of life. His mobility increased significantly and represented by his ability to climb stairs without being in pain or needing walking aids. Today, 2 ½ years after THR surgery, the patient still reports being satisfied and pain free.
Conclusion: Despite transient complications postoperatively, we are happy to report a very satisfactory clinical and radiologic outcome after 10 months. The today 79-year-old patient reports having a higher quality of life since rearticulation of his Girdlestone situation. However, the long-term effects and survival rate of this procedure need to be observed furthermore.
Keywords: Rearticulation, excision arthroplasty (girdlestone), tuberculous coxitis in childhood, wagner cone stem
Tuberculous coxitis accounts for about 15% of all osteoarticular tuberculosis cases and is the second most common after spinal tuberculosis [1, 2]. Girdlestone resection arthroplasty is an option for surgical treatment of these patients [3, 4, 5, 6]. In the course of time, rearticualtion with a total hip arthroplasty (THR) can be considered to regain some function. However, these patients often show a poor bone stock, making THR surgery technically demanding for the surgeon and the chosen implant. In these cases, with significant bone stock loss, the Wagner cone stem offers good preconditions for bone restoration [7, 8, 9]. To the best of our knowledge, there are no previous data examining the assessment and outcome of rearticulation using a prosthesis more than seven decades after Girdlestone.
A 76-year-old male patient was admitted to our department with a painful Girdlestone situation after tube rculous coxitis in his childhood (at 5 years of age). The patient had persistent pain with no significant response to pain therapy. This stigmatized the patient throughout his life and he could not live a normal life. Clinically, there was an approximately 5–7 cm leg length reduction of the right leg in a standing position. Shortening of the limb resulted in permanent knee flexion of 30° on the healthy side (Fig. 1). Pelvis, hip X-ray, and computer tomography were applied as diagnostic tools (Fig. 2).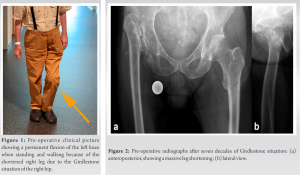
Rearticulation of a Girdlestone-situation requires an individualized treatment and is recommended to reduce pain and improve the quality of life. However, one needs to be aware of the difficult situation interms of the remaining bone stock. The literature shows very good clinical, radiographic, and functional outcomes of the Wagner cone at midterm follow-up in patients with abnormal proximal femoral morphology and previous hip surgery [9]. So far however, we are aware that there are successful clinical results for rearticulation performed up to 6.5 (±4) years after Girdlestone resection arthroplasty, but not after more than seven decades [10]. Nonetheless rearticulation with the Wagner cane stem for this patient was thought justifiable. Alternatively, an arthrodesis could have been considered. However, it would have been a technically challenging surgery due to the missing femoral head-and-neck and existing leg length difference. Ideal candidates for hip arthrodesis are young adults with severe monoarticular disease, especially posttraumatic, with high activity demands and without preexisting lumbar disease or ipsilateral knee or contralateral hip arthritis [11]. When regarding the pre-operative radiographs (Fig. 2) today, the pre-operative situation seems comparable to CROWE Type IV developmental dysplasia of the hip. These cases have been treated with the following unpublished schemata developed by the senior-author (A.M.N.):
• Restoring the center of rotation of the hip using an ACR
• Cementing a PE low profile cup with less inclination (to avoid dislocation) if range of motion (ROM) requirement is low such as in elderly patients
• Alternatively cementing a Double Mobility Cup into the ACR if high ROM is needed such as in young patients (normally 20–40 y)
• Partial release of the iliopsoas major and adductor muscles (if needed) to achieve a leg-lengthening of maximum 4 cm (to avoid a painful hip and sciatic nerve symptoms)
• No release of the Gluteal group (this would have the potential for early abduction of the limb postoperatively, however, decreasing over time)
• Deep positioning of the Wagner cone stem with partial resection of the anteromedial cortical bone close to the lesser trochanter respecting the planned antetorsion (leading to a relatively high greater trochanter).
Using this technique, additional shortening osteotomies can be avoided. The “Mickey Mouse ear-like» greater trochanter (Fig. 5) needs getting used to when looking at the radiographs; however, it shows a good functional outcome and up to date, no trochanter fractures have been observed. The numerous complications which the patient suffered from intraoperatively and during the course of recovery should be looked at critically and taken seriously. The intraoperative femoral fissure around the femoral stem is a potential complication since the bone had been free of significant load for 72 years. The prolonged delirium which the patient had experienced made us has doubts whether it was the right decision to perform this surgery. However, this is an aspect one needs to consider for every surgery needing general anesthesia especially in elderly patients, regardless of the surgical indication.
Despite transient complications postoperatively, clinical and radiologic outcome at 2 ½ years after THR is satisfying. The today 79-year-old patient reported that THR surgery optimized his quality of life enormously. We are thus convinced that we helped the patient in regaining a normal daily life. This case report suggests that the Wagner cone stem can be used for complex THR after a long-term Girdlestone situation. However, it is important to counsel the patient about the possible complications associated with this surgery and long-term outcome as well as survival rate of this procedure needs to be observed further.
This case report intends to raise awareness that rearticulation after more than seven decades after Girdlestone (in this case 72 years) could significantly improve the patients’ quality of life. The Wagner cone stem could be used for complex THR after long-term Girdlestone-situation. However, it is important o counsel the patient about the possible severity and complications associated with this surgery.
References
- 1.Tiwari A, Karkhur Y, Maini L. Total hip replacement in tuberculosis of hip: A systematic review. J Clin Orthop Trauma 2018;9:54-7. [Google Scholar]
- 2.Netval M, Tawa N, Chocholác D. Total hip replacement after tuberculous coxitis. Twenty-seven-year experience (1980-2007). Acta Chir Orthop Traumatol Cech 2008;75:446-50. [Google Scholar]
- 3.Barfod K, Broeng L, Meyer CN. Tuberculous coxitis in the hips 55 years after primary tuberculosis. Ugeskr Laeger 2011;173:1653-4. [Google Scholar]
- 4.Eltorai IJ. The Girdlestone procedure in spinal cord injured patients: A ten year experience. Am Paraplegia Soc 1983;6:85-6. [Google Scholar]
- 5.Cordero-Ampuero J. Girdlestone procedure: When and why. Hip Int 2012;22:S36-9. [Google Scholar]
- 6.Purushotham VJ, Ranganath BT. Total hip arthroplasty in a girdlestone hip following a failed hemiarthroplasty. J Orthop Case Rep 2015;5:47-9. [Google Scholar]
- 7.Parry MC, Vioreanu MH, Garbuz DS, Masri BA, Clive P Duncan CP. The wagner cone stem for the management of the challenging femur in primary hip arthroplasty. J Arthroplasty 2016;31:1767-72. [Google Scholar]
- 8.Schuh A, Schraml A, Hohenberger G. Long-term results of the Wagner cone prosthesis. Int Orthop 2007;33:53-8. [Google Scholar]
- 9.Krenn P, Gehmert S, Krieg AH, Nowakowski AM. Challenging implantation of hip prosthesis in a 32-year-old patient with kniest syndrome. J Orthop Case Rep 2019;9:62-4. [Google Scholar]
- 10.Schröder J, Saris D, Besselaar PP, Marti RK. Comparison of the results of the Girdlestone pseudarthrosis with reimplantation of a total hip replacement. Int Orthop1998;22:215-8. [Google Scholar]
- 11.Beaulé PE, Matta JM Mast JW. Hip arthrodesis: Current indications and techniques. J Am Acad Orthop Surg 2002;10:249-58. [Google Scholar]