Lipoma arborescens are one of the rare benign causes of knee swelling which can be missed with various other common causes of knee swelling, but have to treated as can lead to arthritis and affects individuals activity of daily living and cannot be left alone.
Dr. Amol C Patel, Department of Orthopaedics, Haria Rotary Hospital, Vapi, Gujarat, India. E-mail: dramol1978@yahoo.com
Introduction: Lipoma Arborescens is a chronic, slow growing intra articular lesion of benign nature which is commonly seen in the supra patellar region of the knee joint. It is characterised by villous proliferation of the synovium, with the replacement of the subsynovial connective tissue with fat cells. It is not a neoplasm but non-specific reactive response to chronic synovial irritation, due to mechanical or inflammatory insults. We highlight this condition to raise awareness to be kept as a differential diagnosis in knee joint affected by various slow, progressive chronic inflammatory conditions.
Case Report: We present case of 51-year female with severe knee swelling since 3 to 4 years with episodes of remission and regression on and off. She was diagnosed with lipoma arborescens after magnetic resonance imaging and confirmed after post operative histology.
Conclusion: We in this case study highlight this rare condition with its imaging characteristics and arthroscopic treatment. Keeping in mind that lipoma arborescens though benign in nature and as one of the rare causes for knee swelling, has to be treated to get an optimal outcome.
Keywords: Lipoma Arborescens, synovial membrane, Magnetic Resonance, Arthroscopy
Lipoma arborescens also referred as villous lipomatous proliferation of the synovial membrane, diffuse lipoma of the joint or diffuse synovial lipoma, is a rare benign intra-articular lesion is characterized by villous proliferation of the synovium [1, 2]. The villous proliferation of the synovium has the subsynovial connective tissue replaced with mature fat cells [3]. Albert Hoffa, a German surgeon, made the first description of lipoma arborescens in 1904. Lipoma arborescens typically affects adults. It most commonly involves the knee, but other locations have also been described (shoulder, ankle, hip, wrist, elbow). Bilateral affection of the knee is also described [2, 4]. Furthermore, extra-articular location like tendon sheath and periarticular bursa can also be seen affected by it [4, 5]. Lipoma arborescens is usually diagnosed with magnetic resonance imaging (MRI) and early diagnosis help in differentiating it from other intra-articular lesion and chronic inflammatory condition.
A female patient 50 years old presented with the right knee swelling since 4 years. The swelling was gradually increasing since past 1 year. Initially, the swelling used to increase and decrease on its own. Pain was mild and not affecting activities of daily living. No night pains. No complains of fever, multiple joint pain, bleeding tendencies, loss of weight, and trauma. Conservative treatment was taken at multiple places in form of medication, physiotherapy, knee aspiration, and also local kenacort injection given. Clinical examination revealed massive joint swelling (Fig. 1) with terminal range of motion restricted and painful. No signs of inflammation were noted. Test for meniscus, collateral, and cruciate ligament was negative. X-ray showed early osteoarthritis changes with area of dense soft-tissue opacity in the supra patellar region. Blood investigation showed increase in erythrocyte sedimentation rate: 66 mm and C-reactive protein: 23 mg/dl levels, with normal anti-cyclic citrullinated peptide, S. uric acid, ANA, Rheumatoid factor, bleeding time, clotting time, and blood counts. MRI showed large effusion distending the suprapatellar and infrapatellar region with frond like fatty area seen in peri condylar and joint cavity. Synovial thickening and hypertrophy noted F/S/O Lipoma arborescens. Associated medial compartment degeneration was noted (Fig. 2). Arthroscopic synovectomy was planned. Before arthroscopy knee was aspirated yielding 350 cc of citrulline colored fluid. In arthroscopy, we could visualize diffuse synovitis with frond like masses (Fig. 3) throughout the joint more in the supra patellar and infrapatellar area. The villous type synovitis showed yellow-colored nodules within it. Complete arthroscopic synovectomy (Fig. 4) was done using anterior medial, anterolateral, suprapatellar portals, and posterior medial portal. Post-surgical physiotherapy was started immediately with passive knee bending and weight bearing as tolerated with knee brace. Static Quadricep exercise and ice fomentation were given. Brace was removed within 2 weeks. Cycling was also encouraged after 2 weeks. Post-operative histological studies showed synovial hyperplasia and hypertrophy with distinct lobules of mature adipocytes replacing a significant portion of subsynovial tissue, in keeping with the diagnosis of lipoma arborescens.
Arthroscopic synovectomy was planned. Before arthroscopy knee was aspirated yielding 350 cc of citrulline colored fluid. In arthroscopy, we could visualize diffuse synovitis with frond like masses (Fig. 3) throughout the joint more in the supra patellar and infrapatellar area. The villous type synovitis showed yellow-colored nodules within it. Complete arthroscopic synovectomy (Fig. 4) was done using anterior medial, anterolateral, suprapatellar portals, and posterior medial portal. Post-surgical physiotherapy was started immediately with passive knee bending and weight bearing as tolerated with knee brace. Static Quadricep exercise and ice fomentation were given. Brace was removed within 2 weeks. Cycling was also encouraged after 2 weeks. Post-operative histological studies showed synovial hyperplasia and hypertrophy with distinct lobules of mature adipocytes replacing a significant portion of subsynovial tissue, in keeping with the diagnosis of lipoma arborescens.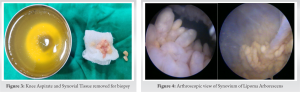
Lipoma arborescens is a rare pathology which is described from the early 20th century, it has been consolidated as a disorder related to slowing evolving, recurrent, and generally painless monoarthritis and progresses with articular effusion and decreased range of motion [6]. Although first described by Hoffa in 1904, more detailed description was done by Arzimanoglu in 1957 [2, 7]. The term lipoma is misleading as lesion does not show any features of lipoma and do Hallel et al. suggested that lipomatous proliferation of the synovial membrane would be an appropriate term [3]. The term arborescens comes from the word Arbor (Latin for tree) and describes macroscopic tree like morphology of lipomatous villous proliferation [2]. There are two etiological types of lipoma arborescens primary and secondary depending on age of onset and underlying pathology. The more common secondary type is associated with underlying chronic irritation such as degenerative disease, trauma, and meniscal injury and seen in old people [4, 8]. The less common primary type is idiopathic and occurs in patient of younger age group between second and third decade [4]. Lipoma arborescens should be considered in the differential diagnosis of monoarthritis with effusion and synovial thickening, such as progressive villonodular synovitis, synovial lipoma, synovial osteochondromatosis, tubercular arthritis, rheumatoid arthritis, and gouty arthropathy [4, 6]. Sometimes, chronic inflammatory conditions are itself associated with lipoma arborescens [9]. The diagnosis of lipoma arborescens is based on typical findings on MRI and is considered as the gold standard [4, 10]. Other tests such as laboratory investigation, joint fluid aspirate, and X-rays can be used to rule out other causes of monoarthritis with effusion [2, 3]. The MRI features of lipoma arborescens have frond like mass arising from the synovium. Second, the mass has fat equivalent signal on all pulse sequences. The lipoma arborescens shows high signal intensity villous or nodular foci on both T1-and T2-weighted images that are suppressed on short tau inversion recovery (STIR) or fat saturation sequences similar to that of any subcutaneous fat. The remaining non-fatty component of hypertrophied synovium in the condition displays heterogeneous high signal intensity on T2 or STIR sequences and intermediate-to-low signal intensity on T1- weighted sequences. Third, there is no enhancement on contrast administration of the subsynovial tissue, but synovial fluid and synovium shows enhancement. Fourth feature is of effusion of varying degree [2, 4]. And finally, there is an absence of magnetic susceptibility effects from hemosiderin which helps it to differentiate from closely mimicking pigmented villonodular synovitis [11]. Other features such as synovial cyst, degenerative changes, meniscal lesion, and bony erosions can be also noted. The subsynovial fatty proliferation in lipoma arborescens usually attains one of three morphological patterns: (a) diffuse villous form, involving the entire hypertrophied synovium; (b) focal nodular frond-like form; or (c) a mixed form of the two aforementioned patterns [12]. Our patient had diffuse villous form with early degenerative and meniscal lesion. Broadly, lipoma arborescens has to be distinguished from intra-articular masses which are broadly classified as non-infectious synovial proliferative lesion, infectious granulomatous lesion, depositional joint disease, neoplastic lesion, and vascular malformation [4]. Among these, synovial osteochondromatosis, PVNS, rheumatoid arthritis, tuberculous arthritis, gouty arthropathy, and intra-articular lipoma are the most common differential diagnoses for this condition, which may pose a diagnostic dilemma, even on imaging [12]. Macroscopically, lipoma arborescens appears as a yellowish synovial proliferation, with broad villous projections of fatty tissue arranged in an arborescent pattern, usually filling the suprapatellar pouch and both gutters. Histologically, massive infiltration of the synovium by mature adipose cells is characteristic for lipoma arborescens. Enlarged hyperemic capillaries and focal chronic inflammatory infiltration are usually observed [13]. Clinically, our case had initially suspicion on rheumatoid arthritis but the lab investigation where not in favor. The X-ray did not show any obvious multiple calcified loose body, so synovial chondromatoisis was ruled out. The patient did not have any clinically sign for tuberculous infection, and also, the laboratory reports were normal. MRI helped us to rule out pigmented villous nodular synovitis and any other intra-articular tumor. Lipoma arborescens was diagnosed on MRI with associated arthritic changes suggested of secondary lipoma arborescens. We wanted to highlight this condition to be kept in mind as differential diagnosis clinically also. It has also been noted that osteoarthritic changes are secondary to the presence of lipoma arborescens. Natera even concludes in his retrospective review that progressive joint degeneration could be prevented or at least delayed, if prompt synovectomy is performed [14, 15]. So even being a benign lesion, it has to be addressed by open or arthroscopic synovectomy, though intra-articular steroids and conservative treatment can give temporary relief [3]. Arthroscopic synovectomy is preferred as is minimally invasive and able to facilitate early post-operative recovery [4]. Furthermore, complete synovectomy can be done with arthroscopy as compared to open as posterior compartment is also visualized. The reported outcomes of an arthroscopic resection have favorable results. Recurrence after synovectomy is very rare [15] except Afonso [16] in his paper showed recurrence at 1-year follow-up. We did not have recurrence until 8 months postoperatively. The choice of one technique over the other mainly depends on the extent of involvement in the joint and on the personal experience of the surgeon [2].
Lipoma arborescens is one of the causes of knee swelling, though rare has to keep in mind for patient with knee swelling. Mostly diagnosed with exclusion and with MRI images. Once diagnosed, it is better to treat the patient with arthroscopic debrima to relive complains and decrease the risk of osteoarthritis.
Lipoma Arborescens mostly diagnosed with MRI, must be treated with arthroscopic debrima for better clinical outcome.
References
- 1.H. W. Garner and J. M. Bestic, “Benign synovial tumors and proliferative processes,” Seminars in Musculoskeletal Radiology, vol. 17, no. 2, pp. 177–188, 2013. [Google Scholar]
- 2.Hallel T, Lew S. Bansal M. Villous lipomatous proliferation of the synovial membrane (lipoma arborescens). J Bone Joint Surg Am 1988; 70:264-70 [Google Scholar]
- 3.Sanat Kumar Sanamadra, Ken Oon Ong, CME Article Lipoma Arbroscence. Singapore Med J 2014;55(1):5-11. [Google Scholar]
- 4.M. De Vleeschhouwer,1 E. Van Den Steen et al, Case Report Lipoma Arborescens: Review of an Uncommon Cause for Swelling of the Knee. Case Reports in Orthopedics Volume 2016, Article ID 9538075, 5 pages. [Google Scholar]
- 5.Shinji Minami, Yusuke Miyake et al, Case Report Lipoma arborescens arising in the extra-articular bursa of the knee joint. SICOT J 2016, 2, 28. [Google Scholar]
- 6.Taissa Pinto de Souza, Juliana Brandao Pinto Carneiro, Monique Freire dos Reis. Case Report: Primary lipoma arborescens of the knee. European journal of rheumatology DOI: 10.5152/eurjrheum.2017.17014. [Google Scholar]
- 7.A. Arzimanoglu, “Bilateral arborescent lipoma of the knee,” The Journal of Bone & Joint Surgery—American Volume, vol. 39, no.4, pp. 976–979, 1957. [Google Scholar]
- 8.T. Hallel, S. Lew, and M. Bansal, “Villous lipomatous proliferation of the synov ial membrane (lipoma arborescens). The Journal of Bone & Joint Surgery—American Volume, vol. 70, no. 2, pp. 264–270, 1988. [Google Scholar]
- 9.Al-Ismail K, Torreggiani WC, Al-Sheikh F, Keogh C, Munk PL. Bilateral lipoma arborescens associated with early osteoarthritis. Eur Radiol 2002; 12:2799-802. [Google Scholar]
- 10.Gozde Ercan Zeybek, et al. Progressive bilateral lipoma arborescens of the knee caused by uncontrolled juvenil idiopathic arthritis . North Clin Istanb 2020;7(5):512–515. [Google Scholar]
- 11.Gozde Ercan Zeybek, et al. Progressive bilateral lipoma arborescens of the knee caused by uncontrolled juvenil idiopathic arthritis . North Clin Istanb 2020;7(5):512–515. [Google Scholar]
- 12.J. F. Feller, M. Rishi, and E. C. Hughes. Lipoma arborescens of the knee: MR demonstration. American Journal of Roentgenology, vol. 1994;163, no. 1, pp. 162–164. [Google Scholar]
- 13.Soler T, Rodríguez E, Bargiela A, Da Riba M. Lipoma arborescens of the knee: MR characteristics in 13 joints. J Comput Assist Tomogr 1998; 22:605-9. [Google Scholar]
- 14.Ioannis Tsifountoudis, Dimitrios Papoutsis , Case Report Lipoma Arborescens of the Knee: Report of Three Cases and Review of the Literature. Case Reports in Medicine Volume 2017, Article ID 3569512, 9. [Google Scholar]
- 15.K. Ikushima, T. Ueda, I. Kudawara, and H. Yoshikawa. Lipoma arborescens of the knee as a possible cause of osteoarthrosis,” Orthopedics, vol. 24, no. 6, pp. 603–605, 2001. [Google Scholar]
- 16.L. Natera, P. E.Gelber, J. I. Erquicia, and J. C.Monllau, “Primary lipoma arborescens of the knee may involve the development of early osteoarthritis if prompt synovectomy is not performed,”Journal of Orthopaedics and Traumatology, vol. 16, no. 1, pp. 47– 53, 2015. [Google Scholar]
- 17.M. Franco, J. M. Puch,M. J. Carayon, D. Bortolotti, L. Albano,and A. Lallemand, “Lipoma arborescens of the knee: report of a case managed by arthroscopic synovectomy,” Joint Bone Spine 2004; 71 (1): 73–75. [Google Scholar]
- 18.P. D. Afonso, Lipoma arborescens. Arthritis Rheum 2012;64 (6): 2054-2054. [Google Scholar]