Should have strong suspicion of atypical stress fractures in any patient who presents with hip pain with any history of bisphosphonate use.
Dr. Arshan J. Dadrewalla, Imperial College Healthcare Trust, St Mary’s Hospital, Praed St, London W2 1NY. Email: arshan.dadrewalla@nhs.net
Introduction: Long-term bisphosphonate use has been linked to an increased risk of pathological neck of femur fractures.
Case Presentation: We write concerning a patient who presented with left hip pain following a low impact fall, which was diagnosed as a pathological left neck of femur fracture. This was a subtrochanteric stress fracture most frequently seen in patients who take bisphosphonate medications. A key point of difference in our patient is the length of time of bisphosphonate use. A further interesting point was the method of imaging used to diagnose this fracture whereby plain radiographs and computerized tomography imaging both did not show any acute fracture whereas only a magnetic resonance imaging (MRI) hip demonstrated this fracture. Surgical insertion of a prophylactic intramedullary nail was done to stabilize the fracture and reduce the risk of progression to a complete fracture.
Conclusion: This case brings up multiple key points not reviewed previously such as the fact a fracture developed only 1 month after bisphosphonate use rather than months or years. These points suggest that there should be a low threshold for investigation (including MRI scanning) into potential pathological fractures and that bisphosphonate use should be a red flag to initiate these investigations regardless of length of use.
Keywords: Atypical stress fractures, bisphosphonate use, magnetic resonance imaging.
We write about this case to raise awareness of an atypical subtrochanteric stress fracture found in our patient. This is a type of fracture seen in patients who are users of bisphosphonate drugs for common conditions such as osteoporosis to rarer conditions such as multiple myeloma. A key point of difference in our patient was the length of time of bisphosphonate use. This type of fracture is usually seen with long-term bisphosphonate use covering years [1] whereas our patient admitted to bisphosphonate use for only 1 month. Due to this atypical presentation, along with no acute fractures seen on imaging, there was a level of uncertainty around the patient’s diagnosis and how it should best be managed, which shall raise awareness for future similar cases.
Our patient presented to hospital with left hip pain following a low impact mechanical fall after slipping. The patient reported having left hip pain leading to reduced mobility post-fall. Before the onset of pain, they reported that they were normally independently mobile with regular activities of daily living. There was no bony pain or any neurological pain noted and no other systemic symptoms such as fever or weight loss. On examination, they were unable to fully flex the left hip due to pain and were tender on palpation on the left lateral hip.
They currently suffer from multiple myeloma, diagnosed in 2016 which is being managed conservatively and with symptom control as per their oncology team. A DEXA scan done in 2018 by the oncology team showed the T-score for the left neck of femur as −0.1, suggesting that bone density was normal. The T-score for the lumbar spine was thus compatible with low bone density.
Medical history also included breast cancer in 2007 which was treated with surgery and chemotherapy and that has been discharged to follow-up. They also suffer from heart failure, hypertension, high cholesterol, and osteopenia. The patient reports often having bony type pains which occur bilaterally in the anterior thigh femoral region over the previous years which are known to the oncology team and managed using opioids.
Interestingly, our patient initially declined taking bisphosphonates, though they did identify a drug named Fosamax (a brand name for Alendronic Acid) which was bought overseas and used once a week for a total of 1 month before being stopped due to unpleasant side effects.
Outpatient X-ray of the hip showed changes of myeloma and thus they were advised to attend A and E.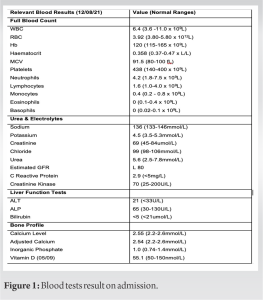
On admission, a full set of blood tests were done including full blood count, urea and electrolytes, liver function tests, and bone profile (Fig. 1).
Inpatient X-ray of the pelvis and left femur (Fig. 2) was inconclusive showing no acute fractures or lytic lesions but just moderate degenerative change. A computerized tomography (CT) hip (Fig. 3) similarly showed no acute fractures but just degenerative changes bilaterally. To further help with diagnosing the problem, a magnetic resonance imaging (MRI) of the hip (Fig. 4) was done. It was this scan that reported an atypical stress fracture to the lateral wall of the left femur.
On review of the MRI hip imaging by the orthopedics team and taking account of the history, an atypical stress fracture in the subtrochanteric region on the left side was identified, which is commonly reported in patients taking bisphosphonates [2]. This was identified by a feature which is associated on radiographs with atypical stress fractures known as the “dreaded black line.” This horizontal plane line denotes subtrochanteric lateral cortical thickening with surrounding proximal and distal cortical thickening of the endosteal and periosteal bone [3].
Following diagnosis, our patient was surgically treated with the insertion of an intramedullary nail to stabilize the fracture (Fig. 5), allowing it to heal as well as reducing the risk of it progressing to a complete fracture. This would be reviewed 6 weeks later in outpatient clinic.
Multiple myeloma and treatment
Multiple myeloma is a plasma cell disorder which accounts for 10–13% of hematological cancers. Bone involvement is one of the most common side effects [4].
A common treatment for multiple myeloma is the use of bisphosphonates [5] due to their mechanism of being specific inhibitors of osteoclastic activity, maintaining bone mineral density and thus reducing the risk of pathological vertebral fractures. However, despite this, bisphosphonate therapy is associated with adverse effects such as suppression of bone turnover due to osteoclast inhibition and induction of apoptosis [6]. This reduced bone quality increases the risk of developing stress fractures, commonly in long bones. As the subtrochanteric region is the area of the femur subjected to maximal bending stress, the reduced bone remodeling causes an increased risk of low-energy fractures [7].
Atypical stress fractures of the femur are well known to be an associated side effect of long-term bisphosphonate use, with patients usually on the treatment for a minimum of 3 years [1]. Another study found on a group of women that incidence of atypical femur fractures increased as period of use increased from 3 to 8 years [8].
There are not many studies looking at an association between short-term bisphosphonate use and atypical stress fractures. One study looked at 39 patients with atypical stress fractures and categorized them based length of bisphosphonate use [2]. They found that 6 out of 39 patients had taken them for <2 years, with an odds ratio of 35.1 suggesting that short-term use can also be risk factor. However, 7 patients who had no bisphosphonate treatment also developed stress fractures thus it is important to also consider other risk factors. This is still considerably longer than the length of time; our patient had used bisphosphonates for, and we question whether other risk factors such as previous cancer, female gender, age, smoking, decreased bone mineral density, decreased bone/muscle strength, and the myeloma may have expedited the development of a fracture [9].
It is important to note that although studies on the use of bisphosphonates demonstrate that risk of atypical femoral fractures can increase, there are suggestions that the absolute risk of atypical femoral facture remains very low compared with the reduction in risk of other fractures [8].
An important point to consider is that the stress fracture was found on an MRI rather than a CT. Patients with atypical femoral fractures have a thicker lateral cortex in the subtrochanteric region on CT before the fracture event and therefore that CT could be useful in early detection of atypical femoral fractures compared to plain radiographs [12]. It is important to note for the future cases how an MRI should also be requested if a CT is negative, especially when there are multiple risk factors such as low impact fall, bisphosphonate use, and background of myelomas. Further an MRI can demonstrate marrow and endosteal edema before radiographic changes of atypical stress fractures and can be useful for early detection in the absence of obvious changes on plain film radiographs [13]. As our patient had not progressed to a complete fracture, the MRI scan was perhaps the most useful in allowing the team to identify the atypical femoral fracture which was not visible on plain radiographs or CT. Thus, it is important to consider its use when there is a suspicion of atypical fracture in patients who consume bisphosphonates.
Due to the atypical nature of this stress fracture, an intramedullary nail was inserted into the bone to fix the fracture as shown in (Fig. 5). This provides greater stability and reduces the risk of complete fracture.
In incomplete stress fractures without pain, conservative management can often be attempted [10]. However, multiple studies have highlighted the benefit of using an IM nail in patients discovered to have an atypical femoral stress fracture and inhibiting its progress to a complete femoral fracture which could cause more harm and require further operative treatment and increased length of hospital stay [3, 11].
Equally, it is important to weigh up risks of surgery in all patients in post-operative outcomes. Although our patient had a medical history of heart failure, hypertension, and osteopenia, it was concluded that the risks of operating and inserting an IM nail were lower than the risk of the fracture progressing to a complete fracture.
An important point to consider is that the stress fracture was found on an MRI rather than a CT. Patients with atypical femoral fractures have a thicker lateral cortex in the subtrochanteric region on CT before the fracture event and therefore that CT could be useful in early detection of atypical femoral fractures compared to plain radiographs [12]. It is important to note for future cases how an MRI should also be requested if a CT is negative, especially when there are multiple risk factors such as low impact fall, bisphosphonate use, and background of myeloma. Further an MRI can demonstrate marrow and endosteal edema before radiographic changes of atypical stress fractures and can be useful for early detection in the absence of obvious changes on plain film radiographs [13]. As our patient had not progressed to a complete fracture, the MRI scan was perhaps the most useful in allowing the team to identify the atypical femoral fracture which was not visible on plain radiographs or CT. Thus, it is important to consider its use when there is a suspicion of atypical fracture in patients who consume bisphosphonates.
Our patient’s presentation provides some important learning points. It goes against normal presentation in two ways. First, that the length of bisphosphonate use is a lot shorter than normal for atypical stress fracture development. Second, the diagnosis was made using MRI as opposed to CT which is more common. This case report suggests that further studies should be carried looking at the links of short-term bisphosphonate use and the development of atypical stress fractures. Furthermore, it underlines the key learning point that there should be a strong suspicion of atypical stress fracture in any patient who presents with hip pain with any use of bisphosphonate use. Furthermore, if plain radiographs or CT are negative, there should be low threshold for using MRI imaging to diagnose or rule out a potential fracture.
Bisphosphonate-related stress fractures are largely associated with long-term use rather than short term use. A fracture pattern was very difficult to identify on X-ray and CT for our patient and it was only when taking an in-depth history which revealed that she had taken bisphosphonates for only 1 month, did the team even consider an atypical stress fracture. This then led to an MRI which helped diagnose the fracture. Therefore, the key clinical message is to have a very low threshold to consider atypical stress fractures in bisphosphonate users and this can be important in the prevention of progression to a full fracture and planning early management.
References
- 1.Ward WG Sr., Carter CJ, Wilson SC, Emory CL. Femoral stress fractures associated with long-term bisphosphonate treatment. Clin Orthop Relat Res 2012;470:759-65. [Google Scholar]
- 2.Meier RP, Perneger TV, Stern R, Rizzoli R, Peter RE. Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med 2012;172:930-6. [Google Scholar]
- 3.Ward W, Carter CJ. Bisphosphonate-associated subtrochanteric stress fractures: An emerging epidemic. Orthop Proc 2018;94:???. [Google Scholar]
- 4.Pozzi S, Raje N. The role of bisphosphonates in multiple myeloma: Mechanisms, side effects, and the future. Oncologist 2011;16:651-62. [Google Scholar]
- 5.Mhaskar R, Kumar A, Miladinovic B, Djulbegovic B. Bisphosphonates in multiple myeloma: An updated network meta-analysis. Cochrane Database Syst Rev 2017;12:CD003188. [Google Scholar]
- 6.Saita Y, Ishijima M, Kaneko K. Atypical femoral fractures and bisphosphonate use: Current evidence and clinical implications. Ther Adv Chronic Dis 2015;6:185-93. [Google Scholar]
- 7.Seraphim A, Al-Hadithy N, Mordecai SC, Al-Nammari S. Do bisphosphonates cause femoral insufficiency fractures? J Orthop Traumatol 2012;13:171-7. [Google Scholar]
- 8.Black DM, Geiger EJ, Eastell R, Vittinghoff E, Li BH, Ryan DS, et al. Atypical femur fracture risk versus fragility fracture prevention with bisphosphonates. N Engl J Med 2020;383:743-53. [Google Scholar]
- 9.Biz C, Berizzi A, Crimì A, Marcato C, Trovarelli G, Ruggieri P. Management and treatment of femoral neck stress fractures in recreational runners: A report of four cases and review of the literature. Acta Biomed 2017;88:96-106. [Google Scholar]
- 10.Lee KJ, Min BW. Surgical treatment of the atypical femoral fracture: Overcoming femoral bowing. Hip Pelvis 2018;30:202-9. [Google Scholar]
- 11.Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res 2011;469:2028-34. [Google Scholar]
- 12.Larsen MS, Schmal H. The enigma of atypical femoral fractures: A summary of current knowledge. EFORT Open Rev 2018;3:494-500. [Google Scholar]
- 13.Harborne K, Hazlehurst JM, Shanmugaratnam H, Pearson S, Doyle A, Gittoes NJ, et al. Compliance with established guidelines for the radiological reporting of atypical femoral fractures. Br J Radiol 2016;89:20150443. [Google Scholar]





