Careful clinical examination and laboratory confirmation should be done to differentiate knee tuberculosis from PVNS. The aim of treatment is to obtained maximum joint function and to delay the related complications.
Dr. Akshay Jadhav, Department of Orthopaedics, Dr. Shankarrao Chavan Government Medical College, Nanded, Maharashtra, India. E-mail: akshayjadhav7337.aj@gmail.com
Introduction: Extra pulmonary Tuberculosis (TB) May mimic other diseases in clinical presentation which might be difficult to differentiate and diagnose. Pigmented villonodular synovitis (PVNS) may closely resemble tuberculosis of the knee joint. In younger patients, without any other co-morbid conditions TB of knee joint and PVNS in the knee might present with involvement of the isolated joint, with swelling which is painful for long duration with restriction in the range of motion. Treatment of both the conditions differs vastly and delay in the treatment can result in permanent disfiguration of the joint.
Case Report: A male 35 years old having a right knee painful swelling since last 6 months. The thorough physical examination, radiographs, and MRI suggest PVNS but an altogether different diagnosis is made after confirmatory investigations, i.e. Histopathological examination.
Conclusion: Clinical and radiological presentation of TB and PVNS can mimic each other . Therefore TB should be suspected specially in the like India (endemic). For confirmation of diagnosis hisptopathological and mycobacterial results are important.
Keywords: Tuberculosis, knee, Pigmented villonodular synovitis
Tuberculosis is disease can resemble many other diseases, clinical presentations can often be misleading. Tuberculosis mimics pose a challenge in diagnosis of TB, particularly extra pulmonary TB [1]. The diagnosis of extra pulmonary TB was usually delayed due to its varied clinical presentations, lack of familiarity, and long course of the illness [2]. Tuberculous arthritis of the knee can present very similar to pigmented villonodular synovitis. Both TB arthritis and pigmented villonodular synovitis in the knee can present as a painful swelling of long standing duration (usually several months to years) and with restricted motion. In MRI, TB and PVNS, show proliferation of synovium, oedema of marrow, and erosion of the bony cortices. Delayed treatment of any one can result in severe articular cartilage or joint destruction. [2 3]. PVNS has two characteristic forms: Localized and Diffuse. [4] Though it is a benign condition, PVNS can cause bony destruction and infiltrate nearby tissue if not treated in time[5]. The basis of treatment for TB arthritis and PVNS vary by great extent[3]. Hence, early diagnosis and differentiating the two diseases is important for improved prognosis. This report describes a patient with TB arthritis, in whom the clinic-radiological findings were mimicing that of PVNS.
A 35 years old male presented with a painful swelling at the right knee since 6 months. The swelling was increasing in size gradually. There was aggravation of pain during joint movement. The patient was given a course of NSAIDS by a local practitioner. Patient had past history of being operated for Koch’s granuloma for which laminectomy was formed 17 years back. Patient went to multiple clinics where knee aspiration was done and had temporary relief after knee aspiration followed by increasing in size of swelling and pain. At one of the clinics, patient knee aspiration was done and sample was sent for investigation and tubercular bacilli were found. Patient was started on AKT. There was improvement in symptoms after treatment but symptoms did not subside completely, and he was given reference of our hospital for further evaluation of symptoms. Initial physical examination reveals slight soft tissue swelling and was associated with pain at the knee joint, without local rise of temperature and redness. His range of motion was 30-70 degree. There was slight increase in blood leucocyte count. Radiological investigation of right knee joint (anteroposterior & lateral view) showed mild soft tissue enlargement without anybony involvement (MRI examination shows heterogeneous lesions Their was foci of synovial thickening with irregularity in suprapatellar area of knee. The lesion was also seen along posterior cruciate ligament and popliteal tendon which points to the diagnosis of PVNS. Local USG shows slight joint effusion in suprapatellar region with moderate collection in suprapatellar bursa. On the basis of examination and radiological investigations, initially patient was diagnosed with PVNS. Open synovectomy and debridement was done by an orthopaedic surgeon and sample was sent for investigation hich revealed inflammatory lesion with clusters of polymorphs and lymphocytes with synovial proliferation with granuloma formation with Langhans cells. Intraoperatively bony nodules were revealed at femoral surface and posterior surface of patella with joint capsule fibrosis and cartilage destruction open biopsy samples examination of taken sample shows chronic granulomatous inflammation which coincides with tuberculosis process, so the patient was advised to continue AKT drugs for 18 months. Four months after surgery, the pain was minimal with adequate active ROM (0-70) of knee At 12 months later, the patient was able to perform active ROM of (0 –100) of the knee with no signs of recurrence.
TB of joints typically involves weight bearing joints. Diagnosis of TB is missed due to its nonspecific presentation and atypical findings. A patient with long standing monoarticular involvement of knee should be suspected to be of tuberculous origin to avoid misdiagnosing patients with similar clinico-radiological characteristics, such as PVNS. Diagnosis of tuberculous arthritis at early stage is required to preserve the joint function. Early confirmation of diagnosis, specific and required treatment can have good prognosis [6]. In the early stages, there is inflamed synovium with oedema, initially, clinically there is joint swelling, muscle spasm, and decreased range of motion. An misdiagnosis may be due to nonspecific presentation, nonspecific diagnostic tools, empirical use of antibiotics, and most important of all, the clinician not including tuberculous arthritis in differential diagnosis due to its rare incidence . A study of patients with TB arthritis of knee, preoperatively diagnosed with examination, radiological investigations, and PCR assay, found that only 20% had correctly been diagnosed at the time of admission. Whereas remaining 80% were preoperatively misdiagnosed with gout, rheumatic or osteoarthritis [3]. The patient mentioned here was suspected of PVNS due to the clinical presentation, x-ray, and MRI characteristics. Both tuberculous knee arthritis and PVNS in young present with monoarticular involvement with long standing painful swelling and limited ROM.(Fig. 1).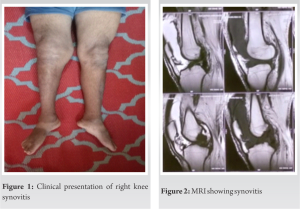 The MRI features of PVNS include joint effusion, marrow oedema, nodular proliferation of synovial membrane and articular cartilage destruction(Fig. 2). Clustering of deposits of hemosiderin show hypointensity on T1 and T2 weighted images which signifies PVNS. MRI plays an important role in making the diagnosis of PVNS [7]. A biopsy is needed for confirming the diagnosis of TB knee or PVNS. A definitive diagnosis of tuberculous involvement depends on culture findings (80% positive rate) [4,8]; But culture requires a long duration (up to 8 weeks). Thus, the histological finding of proliferative synovium and granuloma (Fig. 3) are taken into consideration for making the diagnosis. The aim of treatment of TB arthritis are to obtain a painless joint, removal of infection and restoring joint function[9], the role of surgery in treating TB arthritis is still controversial. Surgery is reserved for establishing the diagnosis or to treat complications. The surgical indications include nonresponse to AKT after 4 to 5 months of therapy, severe joint involvement, joint destruction and deformity, abscess formation , neurological compromise, and painful ankylosis. The surgical procedures that can be carried out include synovectomy, abscess drainage, and joint fusion and Total Knee Arthroplasty if the TB has remained inactive for a long duration (>/=10 years)[10]. The case discussed above had been advised surgery and intraoperative fibrosis(Fig. 4) was seen at knee joint capsule with destruction of the femoral cartilage. Surgical intervention was planned to achieve better functional outcomes, to detect pathology and have improved ROM at the knee joint with less pain ultimately having good prognosis.
The MRI features of PVNS include joint effusion, marrow oedema, nodular proliferation of synovial membrane and articular cartilage destruction(Fig. 2). Clustering of deposits of hemosiderin show hypointensity on T1 and T2 weighted images which signifies PVNS. MRI plays an important role in making the diagnosis of PVNS [7]. A biopsy is needed for confirming the diagnosis of TB knee or PVNS. A definitive diagnosis of tuberculous involvement depends on culture findings (80% positive rate) [4,8]; But culture requires a long duration (up to 8 weeks). Thus, the histological finding of proliferative synovium and granuloma (Fig. 3) are taken into consideration for making the diagnosis. The aim of treatment of TB arthritis are to obtain a painless joint, removal of infection and restoring joint function[9], the role of surgery in treating TB arthritis is still controversial. Surgery is reserved for establishing the diagnosis or to treat complications. The surgical indications include nonresponse to AKT after 4 to 5 months of therapy, severe joint involvement, joint destruction and deformity, abscess formation , neurological compromise, and painful ankylosis. The surgical procedures that can be carried out include synovectomy, abscess drainage, and joint fusion and Total Knee Arthroplasty if the TB has remained inactive for a long duration (>/=10 years)[10]. The case discussed above had been advised surgery and intraoperative fibrosis(Fig. 4) was seen at knee joint capsule with destruction of the femoral cartilage. Surgical intervention was planned to achieve better functional outcomes, to detect pathology and have improved ROM at the knee joint with less pain ultimately having good prognosis.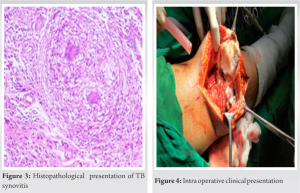
On the basis clinical presentation and radiologic findings TB knee and PVNS are difficult, to differentiate. Therefore, TB knee should be highly suspected, especially in endemic areas. Mycobacterial culture and Histopathological results are necessary to determine the diagnosis.
Clinical presentation of tuberculosis and PVNS are almost similar. Detailed history with examination should be done. Appropriate and timely investigations like MRI, biopsy, histopathology report, etc. should be advised. The main stay of treatment is to start anti TB drugs as soon as possible and to maintain joint mobility and function by prevention joint destruction. If needed surgical intervention should be done.
References
- 1.H. Erdem, O. Baylan, I. Simsek, A. Dinc, S. Pay, M. Kocaoglu, Delayed diagnosis of tuberculous arthritis Jpn. J. Infect. Dis., 58 (2005), pp. 373-375. [Google Scholar]
- 2.7)X.G. Cheng, Y.H. You, W. Liu, T. Zhao, H. Qu . MRI features of pigmented villonodular synovitis (PVNS) Clin. Rheumatol., 23 (2004), pp. 31-34, 10.1007/s10067-003-0827-x. [Google Scholar]
- 3.D.-H. Lee, D.-K. Lee, S.-H. Lee, J.-H. Park, C.-H. Kim, S.-B. Han. Tuberculous arthritis of the knee joint mimicking pigmented villonodular synovitis. Knee Surg. Sports Traumatol. Arthrosc., 20 (2012), pp. 937-940, 10.1007/s00167-011-1662-2. [Google Scholar]
- 4.Dines JS, deberardino TM, Wells JL, et al.: Long-term follow-up of surgically treated localized pigmented villonodular synovitis of the knee. Arthroscopy. 2007, 23:930–937. 10.1016/j.arthro.2007.03.012. [Google Scholar]
- 5.L. Zhao, K. Zhou, Y. Hua, Y. Li, D. Mu. Multifocal pigmented villonodular synovitis in a child: a case report Medicine (Baltimore), 95 (2016), Article e4572, 10.1097/MD.0000000000004572. [Google Scholar]
- 6.C. Tseng. Tuberculosis arthritis: epidemiology, diagnosis, treatment Clin. Res. Foot Ankle., 02 (2014), 10.4172/2329-910X.1000131. [Google Scholar]
- 7.V.Y. Jo, C.D.M. Fletcher. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition Pathology, 46 (2014), pp. 95-104, 10.1097/PAT.0000000000000050. [Google Scholar]
- 8.I. Procopie, E.L. Popescu, V. Huplea, R.M. Pleșea, Ș.M. Ghelase, G.A. Stoica, R.F. Mureșan, V. Onțică, I.E. Pleșea, D.N. Anușca. Osteoraticular tuberculosis-brief review of clinical morphological and therapeutic profiles Curr. Heal. Sci. J., 43 (2017), pp. 171-190, 0.12865/CHSJ.43.03.01. [Google Scholar]
- 9.E.B. Hoffman, J. Allin, J.A.B. Campbell, F.M. Leisegang Tuberculosis of the knee Clin. Orthop. Relat. Res. (2002), pp. 100-106, 10.1097/00003086-200205000-00014. [Google Scholar]
- 10.Muhammad Phetrus Johan, Imeldy Prihatni Purnama, Iswahyudi Nurdin, Ahmad Perdana Asy 'arie et al. "Tuberculosis of the knee masquerading as pigmented villonodular synovitis: Report of two cases". [Google Scholar]







