Hemangioma presenting as painful scoliosis is a rare entity and should be considered one of the differential diagnoses when encountering a case of painful scoliosis in an adolescent. We recommend management of aggressive hemangiomas with neurologic deficit by following a multidisciplinary approach with surgery, pre-operative embolization, and post-operative radiotherapy
Dr. Sathish Muthu, Department of Orthopaedics, Government Medical College, Dindigul, Tamil Nadu, India. E-mail: drsathishmuthu@gmail.com
Introduction: : Spinal hemangioma is the most common benign lesion of the spine with an incidence of 10–12%. Aggressive hemangioma presents with back pain, deformity, or neurologic deficit. Aggressive hemangioma presenting as painful scoliosis is very rare and literature reporting them is very limited.
Case Report: We present the case of a boy in his second decade who presented with back pain for 1 month radiating to his right chest with a deformity in his back. MRI showed a hyperintense lesion involving the sixth dorsal vertebra in the T2-weighted image and a hypointense lesion with striations in STIR images suggestive of hemangioma. Pre-operative embolization was done using micro platinum coils. The patient underwent a decompressive laminectomy and vertebral body decompression. The patient also underwent 12 cycles of adiotherapy. The patient had complete resolution of the deformity without any recurrence at 2 years.
Conclusion: Management of aggressive hemangiomas with neurologic deficit needs a multidisciplinary approach with surgery, pre-operative embolization, and post-operative radiotherapy.
Keywords: Adolescent scoliosis, spinal hemangioma, laminectomy, embolization, scoliosis
Spinal hemangioma is the most common benign lesion of the spine with an incidence of 10–12% [1]. Hemangiomas are mostly asymptomatic. Aggressive hemangioma involves 0.9–1.2% of hemangioma cases and presents with back pain, deformity, neurologic deficit, or myelopathy [2]. Management of hemangioma depends on the clinical symptoms and Enneking staging of the tumor [3]. Bone tumors presenting with painful scoliosis are most commonly seen in osteoid osteoma and osteoblastoma. Aggressive hemangioma presenting as painful scoliosis is a very rare presentation and is rarely described in the literature [4].
A boy in his second decade presented with complaints of mid-back pain for the past 1 month. He complained of radiating pain to his right chest and progressive deformity of his back. There was no history of trauma, fever, loss of weight and appetite, or chronic cough. No history of weakness, numbness, or bowel/bladder disturbances. On examination, there was tenderness over the dorsal spine region without any neurologic deficit, and with normal reflexes. Scoliosis to the right with the right shoulder at a higher level was noted.
Investigations
Radiographic evaluation with plain radiograph demonstrated right thoracic scoliosis as shown in Fig. 1. Further imaging with MRI showed a hyperintense lesion involving the sixth dorsal vertebral body and the pedicle in the T2-weighted image and which appeared hypointense with striations in STIR images as shown in Fig. 1. A mild collapse of the vertebral body was also seen. We noted spinal cord compression from anterior soft tissues as shown in the axial sections of the MRI as shown in Fig. 1.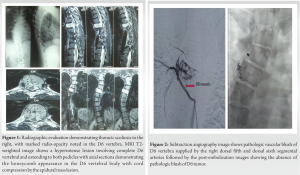
Differential diagnosis
Although the MRI features we more in favor of hemangioma of the spine, we also had differential diagnoses such as aneurysmal bone cyst, Paget’s disease, and osteosarcoma of the spine considering the presenting features.
Treatment
A provisional diagnosis of aggressive hemangioma of the spine was arrived on excluding other differential diagnoses given the MRI features. The patient was planned for pre-operative embolization followed by decompression surgery. We performed a digital subtraction angiography that showed a pathologic vascular blush at the D6 vertebra which was supplied by the right fifth and sixth dorsal segmental arteries as shown in Fig. 2. Pre-operative embolization was done using micro platinum coils. Post-embolization injection showed a minimal blush with gross devascularization of the D6 tumor as shown in Fig. 2. The patient was taken for surgery the following day. The lesion was approached via the posterior approach. Intraoperative neuromonitoring was used to monitor collateral damage to the cord from the thermal ablation of tumor tissue. Intraoperatively, a reddish-pink vascular tissue was seen compressing the cord forming a mesh around it as shown in Fig. 3. We noticed the left D6 root to be thinned out which was ligated and transacted for tumor clearance. The tumor was located in the epidural space encasing the cord. We have done D6 decompressive laminectomy, left facetectomy, pediculectomy, and body decompression as shown in Fig. 3. Following decompression, we stabilized the spine with pedicle screws from D5 to D7, and posterolateral fusion was done as shown in Figs. 3 and 4. The intraoperative frozen section of the lesion demonstrated foamy macrophages suggestive of hemangioma. The total blood loss was around 250 ml. Outcome and follow-up The patient was mobilized from the 2nd post-operative day. Histopathology reports were consistent with hemangioma showing thin-walled blood-filled vascular spaces lined by flat endothelial cells with bland nuclei as shown in Fig. 5.
Pre-operative embolization was done using micro platinum coils. Post-embolization injection showed a minimal blush with gross devascularization of the D6 tumor as shown in Fig. 2. The patient was taken for surgery the following day. The lesion was approached via the posterior approach. Intraoperative neuromonitoring was used to monitor collateral damage to the cord from the thermal ablation of tumor tissue. Intraoperatively, a reddish-pink vascular tissue was seen compressing the cord forming a mesh around it as shown in Fig. 3. We noticed the left D6 root to be thinned out which was ligated and transacted for tumor clearance. The tumor was located in the epidural space encasing the cord. We have done D6 decompressive laminectomy, left facetectomy, pediculectomy, and body decompression as shown in Fig. 3. Following decompression, we stabilized the spine with pedicle screws from D5 to D7, and posterolateral fusion was done as shown in Figs. 3 and 4. The intraoperative frozen section of the lesion demonstrated foamy macrophages suggestive of hemangioma. The total blood loss was around 250 ml. Outcome and follow-up The patient was mobilized from the 2nd post-operative day. Histopathology reports were consistent with hemangioma showing thin-walled blood-filled vascular spaces lined by flat endothelial cells with bland nuclei as shown in Fig. 5. 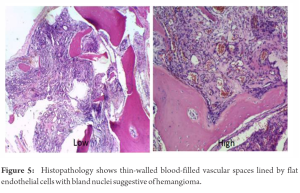 The patient was started on radiotherapy 4 weeks following surgery. The patient received 12 cycles of intensity-modulated radiotherapy. At 2-year follow-up, he is completely relieved of pain and deformity without any sign of recurrence.
The patient was started on radiotherapy 4 weeks following surgery. The patient received 12 cycles of intensity-modulated radiotherapy. At 2-year follow-up, he is completely relieved of pain and deformity without any sign of recurrence.
Vertebral hemangiomas are benign vascular malformations with abnormal venous channels, flattened endothelium, and absent smooth muscle. It is composed of slow-flowing dilated vessels and fat infiltrating the medullary cavity. Vertebral hemangiomas are mostly an asymptomatic incidental finding. Aggressive hemangioma come under Enneking Type 3 lesion with extraosseous extension that accounts for 0.9–1.2% incidence [2]. Patients with aggressive hemangioma present with back pain, radiculopathy, or myelopathy due to spinal stenosis, bone expansion, or vertebral fracture. Hemangioma presenting with deformity is rarely seen [5]. These lesions were radiographically diagnosed with characteristic thickened trabeculae and vertical striations due to fatty infiltrations
presenting as a “corduroy appearance.” CT imaging shows a “polka dot appearance” due to prominent trabeculae in the axial section. MRI shows a hyperintense lesion in T1 (fat content) and T2 (vascular component) weighted images [6]. Occasionally aggressive hemangiomas present as a hypointense lesion in T1-weighted image due to decreased fat content. Management of symptomatic lesions involves surgery, endovascular embolization, radiotherapy, chemical ablation, vertebroplasty, or kyphoplasty [7]. Surgical resection is commonly indicated for large lesions compressing the cord and in cases with neurologic deficits. Dobran et al. [8] noted good outcomes in vertebral hemangiomas managed with laminectomy and resection of epidural lesions in cases with spinal cord compression due to soft-tissue expansion into the canal. Endovascular embolization is mostly used preoperatively to decrease the vascularity of the lesion and reduce blood loss during surgery [9]. Embolization is done using particulate agents (polyethylene glycol), gel foam, coils, and liquid polymerizing agents. It involves fluoroscopic controlled endovascular blocking of blood flow to the tumor. Embolization is contraindicated if the hemangioma feeding vessel also supplies the artery of Adamkiewicz [10], Yao and Malek [11] in their study of five cases recommend pre-operative adjunct embolization for surgical resection of highly vascular tumors. Robinson et al. [12], in their study observed less bleeding in the embolized group compared to a non-embolized group and recommend embolization before surgery for symptomatic cases. Acosta et al. [3], in their study of 16 cases recommend pre-operative embolization and surgical excision for vertebral hemangiomas. Chemical ablation involves the instillation of absolute alcohol into the lesion. It is associated with higher complications such as vertebral compression fracture and neurological complications. Radiotherapy can be used as a primary modality for slow-progressing cases with pain alone [13]. Sedeño et al. [4] recommended dosage of external beam radiation of 40 Gy over 4 weeks for complete eradication of tumor and prevention of recurrence. Radiotherapy cannot be used as the first line in cases with a neurological deficit as radiation takes a long time for clinical and radiological improvement. Surgical treatment is superior to radiotherapy in those cases as surgery allows immediate decompression and provides mechanical stability [14]. Jayakumar et al. [15] in their series of 12 patients with aggressive hemangioma with a neurologic deficit were treated with pre-operative embolization, decompressive laminectomy, and adjuvant radiotherapy to have a favorable outcome and low recurrence rate. Djindjian et al. [16] in their 6-year follow-up study had complete resolution of symptoms and no recurrence in cases treated with pre-operative embolization, decompressive laminectomy, and adjuvant radiotherapy. Vasudeva et al. [17] in their study on five cases found no difference in recurrence rate between subtotal resection, gross total resection, or en bloc resection. Hence, we managed our case with preoperative embolization, decompressive laminectomy, and adjuvant radiotherapy.
Hemangioma presenting as painful scoliosis is a rare entity and should be considered one of the differential diagnoses when encountering a case of painful scoliosis in an adolescent. We recommend management of aggressive hemangiomas with neurologic deficit by following a multidisciplinary approach with surgery, pre-operative embolization, and post-operative radiotherapy.
Hemangioma although being a rare cause of painful scoliosis should be considered as one of the differential diagnoses in an adolescent. Management of such aggressive hemangiomas with neurologic deficit would necessitate a multidisciplinary approach with surgery, pre-operative embolization, and post-operative radiotherapy.
References
- 1.Tomasian A, Wallace AN, Jennings JW. Benign spine lesions: Advances in techniques for minimally invasive percutaneous treatment. AJNR Am J Neuroradiol 2017;38:852-61. [Google Scholar]
- 2.Nguyen JP, Djindjian M, Gaston A, Gherardi R, Benhaiem N, Caron JP, et al. Vertebral hemangiomas presenting with neurologic symptoms. Surg Neurol 1987;27:391-7. [Google Scholar]
- 3.Acosta FL Jr., Dowd CF, Chin C, Tihan T, Ames CP, Weinstein PR. Current treatment strategies and outcomes in the management of symptomatic vertebral hemangiomas. Neurosurgery 2006;58:287-95. [Google Scholar]
- 4.Sedeño BP, Ibarria NR, Hamdani HM, Varela TF, Arregui IS, Verde DM, et al. First reported treatment of aggressive hemangioma with intraoperative radiation therapy and kyphoplasty (Kypho-IORT). Clin Transl Radiat Oncol 2017;2:19-22. [Google Scholar]
- 5.Friedman DP. Symptomatic vertebral hemangiomas: MR findings. AJR Am J Roentgenol 1996;167:359-64. [Google Scholar]
- 6.Leeds NE, Kumar AJ, Zhou XJ, McKinnon GC. Magnetic resonance imaging of benign spinal lesions simulating metastasis: Role of diffusion-weighted imaging. Top Magn Reson Imaging 2000;11:224-34. [Google Scholar]
- 7.Cloran FJ, Pukenas BA, Loevner LA, Aquino C, Schuster J, Mohan S. Aggressive spinal haemangiomas: Imaging correlates to clinical presentation with analysis of treatment a l gorithm and c l ini c a l out come s. Br J Radiol 2015;88:20140771. [Google Scholar]
- 8.Dobran M, Mancini F, Nasi D, Gladi M, Sisti S, Scerrati M. Surgical treatment of aggressive vertebral hemangioma causing progressive paraparesis. Ann Med Surg (Lond) 2018;25:17-20. [Google Scholar]
- 9.Sedora-Roman NI, Gross BA, Reddy AS, Ogilvy CS, Thomas AJ. Intra-arterial onyx embolization of vertebral body lesions. J Cerebrovasc Endovasc Neurosurg 2013;15:320-5. [Google Scholar]
- 10.Gross CE, Hodge CH, Binet EF, Kricheff II. Relief of spinal block during embolization of a vertebral body hemangioma. Case report. J Neurosurg 1976;45:327-30. [Google Scholar]
- 11.Yao KC, Malek AM. Transpedicular N-butyl cyanoacrylate-mediated percutaneous embolization of symptomatic vertebral hemangiomas. J Neurosurg Spine 2013;18:450-5. [Google Scholar]
- 12.Robinson Y, Sheta R, Salci K, Willander J. Blood loss in surgery for aggressive vertebral haemangioma with and without embolisation. Asian Spine J 2015;9:483-91. [Google Scholar]
- 13.Aich RK, Deb AR, Banerjee A, Karim R, Gupta P. Symptomatic vertebral hemangioma: Treatment with radiotherapy. J Cancer Res Ther 2010;6:199-203. [Google Scholar]
- 14.Ogawa R, Hikata T, Mikami S, Fujita N, Iwanami A, Watanabe K, et al. Total en bloc spondylectomy for locally aggressive vertebral hemangioma causing neurological deficits. Case Rep Orthop 2015;2015:724364. [Google Scholar]
- 15.Jayakumar PN, Vasudev MK, Srikanth SG. Symptomatic vertebral haemangioma: Endovascular treatment of 12 patients. Spinal Cord 1997;35:624-8. [Google Scholar]
- 16.Djindjian M, Nguyen JP, Gaston A, Pavlovitch JM, Poirier J, Awad IA. Multiple vertebral hemangiomas with neurological signs. Case report. J Neurosurg 1992;76:1025-8. [Google Scholar]
- 17.Vasudeva VS, Chi JH, Groff MW. Surgical treatment of aggressive vertebral hemangiomas. Neurosurg Focus 2016;41:E7. [Google Scholar]








