We report the first vectored transmission of Lactococcus garvieae from a bovine reservoir causing a TKA PJI. Careful investigation of a patient’s exposure to the host reservoir(s) of an unusual microbe is essential before dismissing the organism as a contaminant result.
Dr. Madhav Chowdhry, Department of Orthopaedic Surgery, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. E-mail: madhav.chowdhry@gmail.com
Introduction: Periprosthetic joint infection (PJI) remains a challenging complication of joint replacement surgery. With the more frequent use of immune modifying drugs and dietary changes in human populations, the resultant blunting of immune defenses allows for infections with less common organisms.
Case Report: Lactococcus garvieae is an anaerobic, gram-positive coccus with reservoirs in fish and domesticated farm animals. Only two prior cases of PJI due to L. garvieae have been reported, both with reported marine transmission. We report a case of L. garvieae associated PJI in a cattle rancher with the first reported case of transmission from a bovine reservoir. The PJI was associated with intra-articular rice body formation, and the diagnosis confirmed with the aid of next generation DNA sequencing. A successful two stage exchange was performed. We propose a novel transmission mechanism with microbe entry via direct hematogenous inoculation during the patient’s duties as a rancher.
Conclusion: When an unusual organism is detected in a PJI, the treatment team should research the host reservoir(s) of the organism and correlate with the patient’s exposure risk. While contamination of cultures is possible, a thorough investigation should be performed prior to that assumption. This reinforces the basic concept that a careful history remains vital when treating an unusual infection presentation. Next generation DNA sequencing is a useful confirmatory tool in establishing the offending organism. Lastly, the identification of rice bodies should raise suspicion for infection. Although not always associated with infection, efforts should be redoubled to identify or rule out a causative micro-organism(s).
Keywords: Lactococcus garvieae, Periprosthetic Joint Infection, PJI, Total Knee Arthroplasty, TKA, Next Generation DNA Sequencing, Rice Bodies.
Periprosthetic joint infection (PJI) is the most dreaded complication of total joint arthroplasty (TJA). With the increasing volume of TJA’s being performed worldwide, the number of PJI cases is rising concomitantly [1] . Chronic PJI management requires an aggressive exchange protocol with Staphylococcus species and other common skin flora making up the majority of causative organisms [2]. However, with more frequent use of immune modifying medications and dietary changes within human populations, the resultant blunting of immune host defenses allows for alternative microorganisms to become pathogenic contributors in PJI. Polymicrobial infections are on the rise and infections with less common organisms are being observed [3].
Lactococcus garvieae is an anaerobic, gram-positive, and catalase-negative coccus. It is a known saltwater and freshwater fish pathogen, and frequently associated in aquaculture outbreaks [4]. Moreover, its host range includes domestic farm animal populations, especially ruminants, with reported outbreaks in dairy farms [5, 6]. Infections in humans are rare, with less than 100 infections reported in the literature. Existing cases include prosthetic heart valve endocarditis, pacemaker hardware and catheter-associated infections [7-9]. Arthroplasty infections are the rarest, with only two cases reported in the literature, both with suspected transmission via contaminated fish consumption [10, 11]. In this manuscript, we report the first case of a bovine transmitted L. garvieae PJI in a cattle rancher with a TKA, and propose a novel transmission vector.
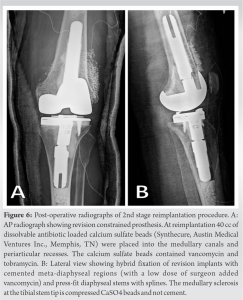
A 65-year-old male was referred to our institution for the second stage reconstruction of a chronic PJI of his left TKA. The patient owned and actively worked on a cattle ranch in Southern California. His past medical history included atrial fibrillation, gastroesophageal reflux disease, and a history of renal cell cancer that was successfully treated. He underwent primary left TKA in September 2016 for non-inflammatory gonarthrosis [Fig. 1a-c]. 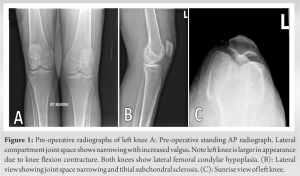
In August 2018, (2 years post-operatively), Lactococcus garvieae was isolated from a knee aspiration culture. The positive culture was appraised as a contaminant, and antimicrobial therapy was not initiated. In April 2019, a left knee aspiration was performed in a consultation exam with additional analysis that included next generation microbial DNA sequencing. L. garvieae was identified on culture, and confirmed with next generation DNA analysis. The patient underwent a diagnostic arthroscopic synovial biopsy in June 2019. Preoperative radiographs are shown in Fig. 2a-c. During this procedure, numerous (>600) 4-10 mm sized rice bodies were encountered and removed [Fig. 3].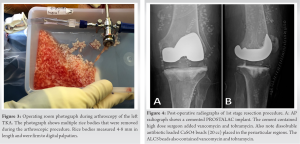
At the patient’s first visit at our center, 2 weeks post-operative, he reported feeling better. His undulating fevers, nighttime chills, and knee pain resolved. He presented weight-bearing as tolerated on his Prostalac implant (Fig. 4a-b), with his knee in a controlled motion brace. Knee range measured 0-75.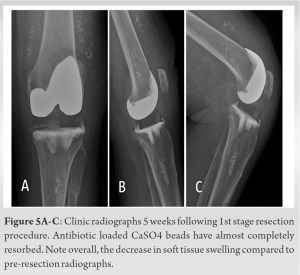
The patient was monitored with serial exams and laboratory testing for inflammatory biomarkers. He was treated with 6 weeks of IV ceftriaxone, followed by an additional 4 weeks of oral ampicillin. His Prostalac implants remained stable [Figs. 5a-c]. After 4 weeks free of antibiotics, the patient had two serial knee aspirations with all samples sent for culture, Synovasure® (CD Diagnostics, Baltimore, USA), alpha defensin and next generation DNA microbial sequencing (MicroGenDX, Lubbock, USA). All aspiration studies were negative, and his serum inflammatory markers were all within normal limits.
Four months after his resection arthroplasty, his knee was reimplanted. His knee was reconstructed with a constrained revision prosthesis [Fig. 6a-b]. He was discharged home on post-operative day four with a 2-week course of oral ampicillin. His hospital admission course was uneventful. His six intraoperative culture specimens were all negative at final report. At his most recent clinic visit, now 2 years post-operatively, he was doing well. He reports no pain from his left knee, and walks with a normal stride and cadence without assistive devices. His left knee range is 0-122° with no extensor lag. Radiographs reveal stable implant fixation with good mechanical alignment [Fig. 7a-c]. He has returned to work as a rancher, although he refrains from some of the more physical manual labor at our recommendation.
PJI remains a problematic complication of joint replacement surgery. The incidence of PJI in hip and knee arthroplasty has remained relatively steady in the last two decades [12]. We believe the persistent incidence of PJI reflects the adaptive mechanisms of microbiota to environmental stresses and host vulnerability to infection [3]. Treatment with systemic immune inhibitors for a wide variety of conditions is advancing rapidly [13]. Prevalent medical comorbidities that include diabetes and tobacco dependence, along with alterations in gut microbiome from modern diets adversely affect host immunity. As a result, a wider variety of causative organisms are noted in PJI [3].
L. garvieae is a facultatively anaerobic, gram-positive, catalase-negative coccus. Previously known as Streptococcus garvieae, it was reclassified to the new genus Lactococcus in 1985 [15]. Device related human infections are rare. Moreover, in our thorough literature review, we identified only two case reports of PJI infections, one involving a total hip arthroplasty (THA) and one involving a TKA.
In their 2011 case report, Aubin et al. describe the case of a 71-year-old woman in France who presented complaining of left hip pain for approximately 1 year [10]. Her medical history included obesity, hypertension, diabetes mellitus, hemochromatosis, ischemic heart disease, chronic alcoholism and a left THA 7 years prior. Aspiration revealed purulent fluid and gram-positive cocci in pairs. She underwent a two-stage exchange procedure, with implant removal and insertion of a gentamicin-impregnated cement spacer for six weeks. Seven out of eight perioperative samples grew L. garvieae. She was treated with IV ceftriaxone and subsequent oral levofloxacin for an antibiotic duration of 3 months. The transmission source was not confirmed, but it was thought to result from contaminated fish consumption or handling, supported by her occupation as a fishmonger. The authors suggest that, while rare, L. garvieae is a potential source of infection in patients exposed to fish, especially in those that are immunosuppressed or have multiple medical co-morbidities.
In 2016, Neagoe et al. reported a patient in Germany, who presented with 5 days of rapid onset right knee pain, redness and swelling, 17 years after undergoing right TKA [11]. The patient was a 79-year-old male, with a medical history including atrial fibrillation, obesity, obstructive sleep apnea and poorly controlled type 2 diabetes. Knee aspiration revealed L. garvieae. The patient was initially treated with a 6-day course of IV cefazolin, followed by arthroscopic I&D. Intraoperative cultures and tissue samples grew L. garvieae. The patient underwent three subsequent open I&D’s, with implant retention, during his 44-day admission. He was discharged after 44 days of treatment without signs of infection and was clinically asymptomatic 6-weeks after discharge. From this report, there is no subsequent follow-up. The proposed source of L. garvieae was consumption of freshwater Nile perch (Lates niloticus). Similar to the previous case, this patient had significant medical comorbidities, highlighting the increased risk for PJI [14].
L. garvieae, being rarely associated with human infection, was a factor in the delayed treatment in our case. Multiple knee aspiration cultures were negative, which may reflect limited local microbiological testing methods. Even when the pathogen was first identified, it was thought to be a contaminant. The positive culture was relegated for several reasons. First, there were multiple prior negative aspiration cultures. Secondly, the possible reservoirs of the pathogen had not been investigated by local health care personnel, and in hindsight, a review of the host reservoirs of L. garvieae may have provided earlier clarity. There are two main reservoirs for L. garvieae: fish and domestic farm animals [15, 16]. Our questioning revealed the patient had a physically demanding job in his role as a cattle rancher. He frequently incurred cuts, lacerations and bruises on his extremities in caring for his cattle. His duties frequently involved lancing oral abscesses, castration of cattle and birthing calves [Fig. 8], the latter which he admits to occasionally undertaking without gloves when a pregnant cow was in distress. We suspect that L. garvieae was directly inoculated through broken skin during one of his many physical activities on the ranch and spread via hematogenous seeding to his TKA. This case highlights the importance of obtaining a detailed history when a diagnosis is elusive and when infection is strongly considered.
Lastly, the finding of rice bodies should raise suspicion for infection. Rice bodies, (corpora oryzoidea) occur in synovial membranes that are chronically inflamed. Corpora oryzoidea (CO) are oval shaped glistening pellets that are firm to palpation and measure generally 4-10 mm in length. Histologically they have an acidophilic core with concentrically laminated fibrin, that gives the glistening appearance. CO formation has been associated most with rheumatoid arthritis, crystal disease, and infections with mycobacteria and candida species. However, it has been noted also with other chronic persistent microbial infections [17-19]. To our knowledge, this is the first report of rice body formation associated with L. garvieae. The exact mechanism of formation is not clear, but it is postulated that synovial cells respond to an inflammatory nidus, and with chronic exposure, rice body formation can occur [20). We note that in all case reports of corpora oryzoidea, there has never been a microbe identified within the rice body core.
We report the third TJA PJI due to L. garvieae, with the first reported case of suspected transmission from a bovine source. We propose a novel route of transmission due to direct mechanical inoculation through broken skin during the patient’s interactions with cattle. The organism was identified late due to its rarity. Confirmation of the organism with next generation DNA sequencing provided confidence that L. garvieae was the offending organism. Successful treatment was accomplished with a two-stage exchange protocol. When an unusual organism is detected, the treatment team should research the host reservoir(s) of the organism and correlate with the patient’s exposure risk. While contamination of cultures is possible, a thorough investigation should be performed prior to that assumption. This reinforces the basic concept that a careful history remains vital when treating an unusual infection presentation. Lastly, the identification of rice bodies should raise suspicion for infection. Although not always associated with infection, efforts should be redoubled to identify or rule out a causative micro-organism(s).
We report the first case of a Lactococcus garvieae TKA PJI transmitted from a bovine reservoir. The mechanism of reservoir transmission was hematogenous seeding via direct mechanical inoculation through a broken skin barrier. Next generation DNA sequencing was helpful in confirming the diagnosis of this rare infection. This PJI was associated with copious intra-articular rice bodies identified on arthroscopic synovial biopsy. The presence of rice bodies although not pathognomonic for infection, should serve as a clue to redouble efforts to test for a fastidious organism.
References
- 1.Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23(7):984-91. [Google Scholar]
- 2.Tan TL, Kheir MM, Shohat N, Tan DD, Kheir M, Chen C, et al. Culture-Negative Periprosthetic Joint Infection: An Update on What to Expect. JB JS Open Access. 2018;3(3):e0060. [Google Scholar]
- 3.Hamad C, Chowdhry M, Sindeldecker D, Bernthal NM, Stoodley P, McPherson EJ. Adaptive antimicrobial resistance, a description of microbial variants, and their relevance to periprosthetic joint infection. The Bone & Joint Journal. 2022;104-B(5):575-80. [Google Scholar]
- 4.Soltani M, Baldisserotto B, Hosseini Shekarabi SP, Shafiei S, Bashiri M. Lactococcosis a Re-Emerging Disease in Aquaculture: Disease Significant and Phytotherapy. Vet Sci. 2021;8(9). [Google Scholar]
- 5.Foschino R, Nucera D, Volponi G, Picozzi C, Ortoffi M, Bottero MT. Comparison of Lactococcus garvieae strains isolated in northern Italy from dairy products and fishes through molecular typing. J Appl Microbiol. 2008;105(3):652-62. [Google Scholar]
- 6.Eraclio G, Ricci G, Moroni P, Santisteban C, Plumed-Ferrer C, Bennett J, et al. Sand bedding as a reservoir for Lactococcus garvieae dissemination in dairy farms. Can J Microbiol. 2019;65(1):84-9. [Google Scholar]
- 7.Chan JF, Woo PC, Teng JL, Lau SK, Leung SS, Tam FC, et al. Primary infective spondylodiscitis caused by Lactococcus garvieae and a review of human L. garvieae infections. Infection. 2011;39(3):259-64. [Google Scholar]
- 8.Lim FH, Jenkins DR. Native valve endocarditis caused by Lactococcus garvieae: an emerging human pathogen. BMJ Case Rep. 2017;2017. [Google Scholar]
- 9.Rosch RM, Buschmann K, Brendel L, Schwanz T, Vahl CF. Lactococcus garvieae Endocarditis in a Prosthetic Aortic Valve: A Case Report and Literature Review. J Investig Med High Impact Case Rep. 2019;7:2324709619832052. [Google Scholar]
- 10.Aubin GG, Bemer P, Guillouzouic A, Cremet L, Touchais S, Fraquet N, et al. First report of a hip prosthetic and joint infection caused by Lactococcus garvieae in a woman fishmonger. J Clin Microbiol. 2011;49(5):2074-6. [Google Scholar]
- 11.Neagoe VI, Zytoun S, Neuhaus HJ. First Case Report of a Late Onset Knee Periprosthetic Joint Infection Caused by Lactococcus garvieae. Case Reports in Orthopedics. 2016;2016:5053640. [Google Scholar]
- 12.Xu C, Goswami K, Li WT, Tan TL, Yayac M, Wang SH, et al. Is Treatment of Periprosthetic Joint Infection Improving Over Time? J Arthroplasty. 2020;35(6):1696-702 e1. [Google Scholar]
- 13.Goodman SM, Springer B, Guyatt G, Abdel MP, Dasa V, George M, et al. 2017 American College of Rheumatology/American Association of Hip and Knee Surgeons Guideline for the Perioperative Management of Antirheumatic Medication in Patients With Rheumatic Diseases Undergoing Elective Total Hip or Total Knee Arthroplasty. Arthritis Rheumatol. 2017;69(8):1538-51. [Google Scholar]
- 14.McPherson EJ, Tontz W, Jr., Patzakis M, Woodsome C, Holtom P, Norris L, et al. Outcome of infected total knee utilizing a staging system for prosthetic joint infection. Am J Orthop (Belle Mead NJ). 1999;28(3):161-5. [Google Scholar]
- 15.Kim JH, Go J, Cho CR, Kim JI, Lee MS, Park SC. First report of human acute acalculous cholecystitis caused by the fish pathogen Lactococcus garvieae. J Clin Microbiol. 2013;51(2):712-4. [Google Scholar]
- 16.Ricci G, Ferrario C, Borgo F, Eraclio G, Fortina MG. Genome Sequences of Two Lactococcus garvieae Strains Isolated from Meat. Genome Announc. 2013;1(1). [Google Scholar]
- 17.Berg E, Wainwright R, Barton B, Puchtler H, McDonald T. On the nature of rheumatoid rice bodies: an immunologic, histochemical, and electron microscope study. Arthritis Rheum. 1977;20(7):1343-9. [Google Scholar]
- 18.Popert AJ, Scott DL, Wainwright AC, Walton KW, Williamson N, Chapman JH. Frequency of occurrence, mode of development, and significance or rice bodies in rheumatoid joints. Ann Rheum Dis. 1982;41(2):109-17. [Google Scholar]
- 19.Pertea M, Veliceasa B, Velenciuc N, Terinte C, Mitrea M, Ciobanu P, et al. Idiopathic tenosynovitis with rice bodies. Rom J Morphol Embryol. 2020;61(2):457-63. [Google Scholar]
- 20.Cheung HS, Ryan LM, Kozin F, McCarty DJ. Synovial origins of Rice bodies in joint fluid. Arthritis Rheum. 1980;23(1):72-6. [Google Scholar]