Patients with pre-operative neurologic symptoms of multilevel spinal stenosis may be prone to post-operative urinary retention and require a careful and sensitive surgical approach
Dr. Hiromitsu Takaoka, 1-8-1 Inohana, Chuo-Ku, Chiba 260-8670, Japan. E-mail: highhilllight@yahoo.co.jp
Introduction: Post-operative urinary retention is a common complication of posterior spine surgery for lumbar spinal stenosis. However, it can result in considerable difficulty for the patient, especially when it is severe, as in cases of complete retention. Therefore, it is crucial to consider its risk factors. This report provides a retrospective review of cases with severe post-operative urinary retention with the aim of elucidating its possible risk factors.
Case Presentation: Data of five patients with post-operative urinary retention after posterior spine surgery for lumbar spinal stenosis, operated in our facility from 2013 to 2020, were analyzed. Their age, preoperative Japanese Orthopaedic Association ( JOA) score, presence of pre-operative bladder and bowel disorders (BBD), presence of pre-operative muscle weakness, the mean number of vertebral levels operated on, complications such as intraoperative dural tear and hematoma, operative time, estimated blood loss, JOA score in the early post-operative period, and the recovery period for the urinary retention symptoms were examined. The mean pre-operative JOA score was 8.4, and the mean number of operated levels was 2.8. The incidence of pre-operative BBD, pre-operative muscle weakness, intraoperative dural tears, and post-operative hematoma was two each. The mean operative time was 242 min, mean estimated blood loss was 352 g, and the mean JOA score in the early post-operative period was 5.8. The recovery period for urinary retention ranged from 4 days to 9 months postoperatively; one patient also had cervical and thoracic spinal stenosis and underwent decompression of all stenotic levels for relief from complete urinary retention.
Conclusion: In our retrospective review of cases with severe post-operative urinary retention after lumbar spinal stenosis surgery, all patients had severe pre-operative symptoms and spinal stenosis at multiple levels. An awareness of potential risk factors and carefully and gently performing the intraoperative procedures can facilitate lesser damage to the spinal nerve.
Keywords: Urinary retention, severe preoperative symptoms, hematoma, dural tear, multiple spinal stenosis.
Post-operative urinary retention is a common complication of lumbar spinal stenosis surgeries, with the incidence ranging from 5.6% to 38% [1]. Once it occurs, however, post-operative recovery is sometimes difficult, with a low rate of postoperative satisfaction [2], especially when the retention is severe and/or complete. Therefore, it is crucial to understand the possible risk factors for severe urinary retention, including the complete type. The purpose of the present study was to explore the possible risk factors for severe and/or post-operative urinary retention after lumbar spinal stenosis surgery by reviewing five clinical cases operated on at our institution, which has rarely been focused on in the current literature.
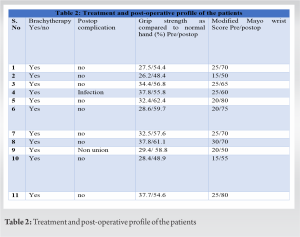
The present study is a case series of patients who developed severe urinary retention after posterior spine surgery for lumbar spinal stenosis. Patients who underwent lumbar spinal stenosis surgery and had post-operative urinary retention were studied. Variables such as age, preoperative Japanese Orthopaedic Association (JOA) score, presence of preoperative bladder and bowel disorders (BBD), presence of severe preoperative neurological disorders such as muscle weakness, the mean number of vertebral levels operated on, presence of perioperative complications such as intraoperative dural tears and post-operative hematoma, operative time, estimated blood loss (EBL), JOA score in the early post-operative period, and recovery period of the urinary retention symptoms from the time of the operation were examined. Five patients who met the inclusion criteria were included and their details are provided in Table 1.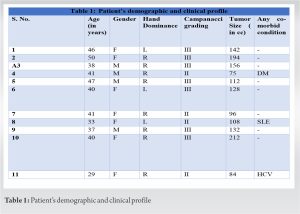
Case 1
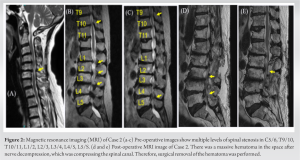
An 84-year-old man underwent L2-3-4-5 partial laminectomy for lumbar spinal stenosis (Fig. 1a). The dura mater was injured intraoperatively and the area around the injured area was fully expanded and sutured with dural sutures.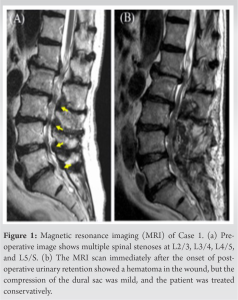
Case 2
A 74-year-old woman with cervical spondylotic myelopathy, thoracic spondylotic myelopathy, and lumbar spinal stenosis underwent C5/6 anterior cervical discectomy and fusion (ACDF) and L2/3, 3/4, 4/5 posterior partial laminectomy due to severe myelopathy combined with cauda equina symptoms (Fig. 2a-c). The operative time was 325 min, and EBL was 180 g. On the 2nd post-operative day, complete urinary retention was noticed after removal of the urethral catheter. Based on the post-operative MRI that showed a massive epidural hematoma (Fig. 2d and e), L2/3, 3/4, 4/5 hematoma removal was performed on the 14th post-operative day, but no change in retention occurred. The repeat MRI detected a massive, as-yet-unrecognized, T9-11 ossification of the ligamentum flavum compressing the spinal cord. The patient therefore underwent T9-11 thoracic posterior decompression and fusion. After the second reoperation, the patient was finally able to urinate on her own, and the urinary function recovered completely 5 months after the first surgery (Fig. 2f).
Risk factors for postoperative urinary retention Pre-operative risk factors for post-operative urinary retention are reportedly advanced age, male sex, history of urinary retention, and prostatic hypertrophy. Intraoperative and post-operative factors include dural tear, exposure of the cauda equina, post-operative hematoma, and prolonged surgery [1, 3, 4, 5]. In our study, the age at surgery was over 65 years in all patients. In addition, two patients had dural tear, and the other two had post-operative hematoma requiring a reoperation. Regarding the operative time, Altschul et al. reported that the mean operative time for patients who developed post-operative urinary retention was more than 210 min, which was significantly longer than that for patients with no post-operative urinary retention [6]. All our cases had an operative duration of over 350 min, which could have been one of the risk factors. As for intraoperative complications, Oshina et al. reported that intraoperative dural tear and exposure of the cauda equina were risk factors for post-operative urinary retention, and that urinary retention was significantly more likely to occur in patients with dural tears [4]. Our study also indicated that intraoperative and post-operative factors, including direct compression of the cauda equina and post-operative hematoma, could cause mechanical stimulation of the cauda equina resulting in urinary retention. Possibility of the relationship between pre-operative neurological vulnerability and mechanical damage In addition to the risk factors mentioned above, there were similarities in the pre-operative physical and imaging findings of our patients. In some cases, BBD and muscle weakness were observed as pre-operative physical findings. In general, BBD and muscle weakness are considered to be symptoms of severe lumbar spinal stenosis [7]. The spinal nerve or cauda equina may have been vulnerable in our patients, and therefore predisposed to post-operative urinary retention triggered by a hematoma or intraoperative mechanical damage to the vulnerable cauda equina [8]. In the present study, we found that most patients with postoperative urinary retention had more than two levels of vertebral spinal stenosis and severe pre-operative clinical symptoms. This indicates that urinary retention may be more likely to occur after surgery for multiple levels of vertebral spinal stenosis, due to the possibility of nerve vulnerability. Therefore, surgeons should take special care in these patients with caudal nerve fragility and perform the procedure gently to prevent intraoperative and post-operative mechanical damage and consequent post-operative urinary retention. Post-operative urinary retention associated with postural change It has been reported that patients with cervical myelopathy due to spinal stenosis may experience worsening of myelopathy during postural change if the stenosis is severe [9, 10]. In Case 2, the myelopathy at the thoracic level could have worsened during post-operative postural change from the prone to supine position during the period between cervical ACDF and posterior lumbar decompression, which may have resulted in her post-operative urinary retention. Duration of improvement in post-operative urinary retention There have been only a few reports on the course of improvement after the onset of post-operative urinary retention. Duncan et al. reported that post-operative urinary retention occurred in 8% of patients who underwent spinal nerve decompression surgery, and that most of the symptoms resolved within 2 weeks to 9 months. However, some patients reportedly require surgical interventions for prostatic enlargement or bladder prolapse [11]. In the present series, the duration of improvement in urinary function seems to have been similar to the previous reports; one case required treatment for bladder prolapse, which can significantly affect the quality of life.
Our case series indicated that several pre-operative neurological symptoms with multiple levels of spinal stenosis can result in severe post-operative urinary retention after posterior spine surgery. Surgeons should ensure more caution and perform surgical maneuvers gently and carefully to avoid the risk of post-operative urinary retention in these patients.
Spinal stenosis patients with severe pre-operative neurological symptoms often experience poor improvement after surgery. In this study, we mentioned the possibility that such patients with severe spinal stenosis may be prone to post-operative urinary retention. In such cases, careful and delicate surgery is required.
References
- 1.Golubovsky JL, Ilyas H, Chen J, Tanenbaum JE, Mroz TE, Steinmetz MP. Risk factors and associated complications for postoperative urinary retention after lumbar surgery for lumbar spinal stenosis. Spine J 2018;18:1533-9. [Google Scholar]
- 2.Zakaria HM, Lipphardt M, Bazydlo M, Xiao S, Schultz L, Chedid M, et al. The preoperative risks and two-year sequelae of postoperative urinary retention: Analysis of the Michigan spine surgery improvement collaborative (MSSIC). World Neurosurg 2020;133:e619-26. [Google Scholar]
- 3.Cremins M, Vellanky S, McCann G, Mancini M, Sanzari L, Yannopoulos A. Considering healthcare value and associated risk factors with postoperative urinary retention after elective laminectomy. Spine J 2020;20:701-7. [Google Scholar]
- 4.Oshina M, Segawa T, Manabe N, Oshima Y, Tanaka S, Inanami H. Incidence, prognosis, and risk factors for bladder and bowel dysfunction due to incidental dural tears in lumbar microendoscopic surgery. Spine J 2020;20:688-94. [Google Scholar]
- 5.Lee S, Kim CH, Chung CK, Park SB, Yang SH, Kim SH, et al. Risk factor analysis for postoperative urinary retention after surgery for degenerative lumbar spinal stenosis. Spine J 2017;17:469-77. [Google Scholar]
- 6.Altschul D, Kobets A, Nakhla J, Jada A, Nasser R, Kinon MD, et al. Postoperative urinary retention in patients undergoing elective spinal surgery. J Neurosurg Spine 2017;26:229-34. [Google Scholar]
- 7.Watanabe K, Sekiguchi M, Yonemoto K, Nikaido T, Kato K, Otani K, et al. Bowel/bladder dysfunction and numbness in the sole of the both feet in lumbar spinal stenosis-a multicenter cross-sectional study. J Orthop Sci 2017;22:647-51. [Google Scholar]
- 8.Tomkins-Lane CC, Battié MC, Hu R, Macedo L. Pathoanatomical characteristics of clinical lumbar spinal stenosis. J Back Musculoskelet Rehabil 2014;27:223-9. [Google Scholar]
- 9.Orendácová J, Cízková D, Kafka J, Lukáčová N, Maršala M, Šulla I, et al. Cauda equina syndrome. Prog Neurobiol 2001;64:613-37. [Google Scholar]
- 10.Buchowski JM, Kebaish KM, Suk KS, Kostuik JP, Athanasou N, Wheeler K. Central cord syndrome after total hip arthroplasty: A patient report. Spine (Phila Pa 1976) 2005;30:E103-5. [Google Scholar]
- 11.Association of Perioperative Registered Nurses. Perioperative Standards and Recommended Practice 2012 Edition. United States: Association of Perioperative Registered Nurses; 2012. [Google Scholar]