Paget’s disease although is a rare incidental finding in cases of trauma cases, early fixation can yield a better clinical outcome in cases of acetabular fractures.
Dr. Niranjan Sunil Ghag, Department of Orthopaedics, Dr. Shankarrao Chavan Government Medical College, Nanded, Maharashtra, India. E- mail: drrkambulgekar@gmail.com; niranjanghag95@gmail.com
Introduction: Acetabular injuries are uncommon, with a reported yearly incidence of three cases per 100,000 people. Paget’s disease of the bones is a frequent condition marked by accelerated yet disordered bone remodeling. Some people have no symptoms, but others have bone discomfort or other consequences, including fractures and deformities.
Case Report: We are presenting the case of a 38-year-old man with Paget’s disease who had a right roof, anterior wall, and posterior wall fracture of the acetabulum with an inferior pubic rami fracture, which was treated surgically with a plate and screw followed by physiotherapy and resulted in a favorable clinical outcome.
Conclusion: Paget’s disease may be asymptomatic initially but may present with pathological fractures. Acetabular fractures in these patients have a good clinical outcome if they are repaired, but increased bone remodeling can lead to arthritic changes.
Keywords: Acetabulum fracture, Paget’s disease, fixation of acetabular fracture, arthritis.
Acetabular fractures are uncommon, with just three documented cases per 100,000 people each year [1]. The presence of associated hip dislocation and neurovascular compromise demands urgent fixation of acetabular fractures. Poor bone quality, frequent fractures, non-union, and secondary arthritis are all complications of Paget’s disease. Sir James Paget, a British physician, first identified Paget disease of bone (PDB) in 1877, naming the ailment “osteitis deformans” since he felt the disease was caused by persistent inflammation. It is an osseous dysplasia that affects persons in their forties and fifties [2]. It is distinguished by a focused modification in bone remodeling, resulting in a bone with an abnormal structure and altered mechanical characteristics, which are linked to discomfort, early arthritis, and pathological fractures [2]. The diagnosis of PDB is often suspected by the finding of an elevated serum alkaline phosphatase (ALP) in patients who have otherwise normal liver function or on the basis of the typical X-ray findings of osteosclerosis and osteolysis disrupting the normal trabecular pattern in the affected bone, cortical thickening, and bone expansion [3, 4], with involvement of the pelvis in 70% of cases [4, 5]. Initially, lytic activity predominates, resulting in localized osteolytic lesions. Sclerosis develops later, resulting in the distinctive presentations of mixed sclerotic and lytic regions, thicker trabecula, bone growth, deformity, and cortical thickening. The radiographic presentations are typically characteristic; however, the differential diagnosis of lytic or sclerotic metastases must be considered on occasion [6]. Complete immobilization of pagetic bone should be avoided because the intercurrent osteopenia of immobilization further imperils the structural integrity of bone already weakened by Paget’s disease. Internal fixation in Paget’s disease is often necessary for managing pagetic complications [7].
A 38-year-old male was brought to our tertiary care center following a high-velocity trauma (skid of a two-wheeler). After the trauma, the patient could not stand or walk without support. The primary assessment in the emergency department found a hemodynamically stable patient. with blunt trauma to the right hip and the underlying suspicion of a fracture of the hip or proximal femur due to the chief complaints of pain and an inability to bear weight, which led to pelvic radiographs and computed tomography (CT) scans. Trauma series X-rays (pelvis with both hips and Judet views) (Fig. 1-6) and The CT scans show communited displaced right acetabulum fracture involving the roof, anterior, and posterior wall of the right acetabulum extending superiorly to involve part of the iliac wing with a right linear displaced fracture of the inferior pubic rami with diffuse osteopenia of bone, giving Judet and Letournel classification of the associated fracture: Anterior column and posterior A thorough secondary examination revealed no further lesions, and both the motor and sensory components of the sciatic nerve were both clinically intact. The patient had tenderness over the anterior groin region and restriction in hip movements (active movements were impossible due to acute pain at the time of admission, but the patient’s hip movements remained restricted after adequate analgesia). The patient had bilateral bowing of the upper and lower limbs in the cortex and between the areas of sclerosis with Coarsening of the trabeculae, kyphoscoliotic deformity at the spine, and bilateral protrusion of the acetabuli. Plain pelvic films with the pelvic brace removed, as well as Judet views, were taken. This confirmed the CT findings of a comminuted displaced fracture of the right acetabulum involving the roof, anterior, and posterior walls of the right acetabulum and extending superiorly to involve part of the iliac wing with a right linear displaced fracture of the inferior pubic rami with bilateral protrusio-acetabuli and arthritic changes with diffuse osteopenia of bone, giving Judet and Letournel the classification of an associated fracture: Anterior column and posterior hemitransverse type. The patient has Paget’s disease and had normal values for all routine work-ups, including blood levels of ca2+: 12.3, sr ALP: 180 IU/L, and radiographic findings supporting the diagnosis. After preanesthetic evaluation and workup, the patient was posted for elective surgery for fixation of the acetabulum with a reconstruction plate and screw. The patient was kept supine, and a modified Stoppas approach was used. 10 cm Pfannenstiel incision taken 2 cm above the pubic symphysis soft-tissue dissection is done. The urinary bladder was retracted using a Deaver retractor. The corona mortis was identified, clipped using vascular clips, and ligated with vicryl. The iliopectineal fascia was cut along the inner border of the pelvic brim using a Cobb’s elevator, deep blunt dissection was performed, and the fracture site was identified and reduced using a ball spike. 12 hole recon plate contoured according to the patient’s template plate Two screws are inserted beneath the fracture site and two are inserted above the fracture site. Bone wax is applied to the exposed comminuted fracture site.
The patient had tenderness over the anterior groin region and restriction in hip movements (active movements were impossible due to acute pain at the time of admission, but the patient’s hip movements remained restricted after adequate analgesia). The patient had bilateral bowing of the upper and lower limbs in the cortex and between the areas of sclerosis with Coarsening of the trabeculae, kyphoscoliotic deformity at the spine, and bilateral protrusion of the acetabuli. Plain pelvic films with the pelvic brace removed, as well as Judet views, were taken. This confirmed the CT findings of a comminuted displaced fracture of the right acetabulum involving the roof, anterior, and posterior walls of the right acetabulum and extending superiorly to involve part of the iliac wing with a right linear displaced fracture of the inferior pubic rami with bilateral protrusio-acetabuli and arthritic changes with diffuse osteopenia of bone, giving Judet and Letournel the classification of an associated fracture: Anterior column and posterior hemitransverse type. The patient has Paget’s disease and had normal values for all routine work-ups, including blood levels of ca2+: 12.3, sr ALP: 180 IU/L, and radiographic findings supporting the diagnosis. After preanesthetic evaluation and workup, the patient was posted for elective surgery for fixation of the acetabulum with a reconstruction plate and screw. The patient was kept supine, and a modified Stoppas approach was used. 10 cm Pfannenstiel incision taken 2 cm above the pubic symphysis soft-tissue dissection is done. The urinary bladder was retracted using a Deaver retractor. The corona mortis was identified, clipped using vascular clips, and ligated with vicryl. The iliopectineal fascia was cut along the inner border of the pelvic brim using a Cobb’s elevator, deep blunt dissection was performed, and the fracture site was identified and reduced using a ball spike. 12 hole recon plate contoured according to the patient’s template plate Two screws are inserted beneath the fracture site and two are inserted above the fracture site. Bone wax is applied to the exposed comminuted fracture site. Reduction and fixation checked under the c-arm, which was acceptable. (Fig. 7-11) (Fig. 17-22).
Reduction and fixation checked under the c-arm, which was acceptable. (Fig. 7-11) (Fig. 17-22).
 Intravenous antibiotics, as well as enoxaparin and analgesics, were administered for 72 h after surgery, after which the patient was shifted to oral antibiotics. The physiotherapists began CPM to attain hip flexion of 90° by the end of the initial month.
Intravenous antibiotics, as well as enoxaparin and analgesics, were administered for 72 h after surgery, after which the patient was shifted to oral antibiotics. The physiotherapists began CPM to attain hip flexion of 90° by the end of the initial month.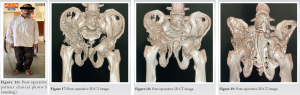 He was immobilized initially, with passive exercises for strengthening the quadriceps and hamstrings taught. By the end of 1 1/2 months, the patient was weight bearing and walking without assistance. At 3 months, follow-up radiographs revealed an uniting fracture with accompanying Brooker Grade 2 heterotopic ossification. The Harris hip score was 75.75, which indicated a fair outcome. The Oxford Hip score was 23 out of 48, and EQ-5D-5L scores were 2 for mobility, 2 for self-care, 2 for usual activities, 2 for pain or discomfort, and 1 for anxiety or depression, with a rating of 70% for overall health at 3 months post-surgery. At the 6th month, re-evaluation revealed a Harris hip score of 91.00, indicating an excellent outcome on the scale. The Oxford Hip score was 46 out of 48, indicating satisfactory joint function. He returned to his employment in the shop 4 months post-surgery. (Fig. 12-16).
He was immobilized initially, with passive exercises for strengthening the quadriceps and hamstrings taught. By the end of 1 1/2 months, the patient was weight bearing and walking without assistance. At 3 months, follow-up radiographs revealed an uniting fracture with accompanying Brooker Grade 2 heterotopic ossification. The Harris hip score was 75.75, which indicated a fair outcome. The Oxford Hip score was 23 out of 48, and EQ-5D-5L scores were 2 for mobility, 2 for self-care, 2 for usual activities, 2 for pain or discomfort, and 1 for anxiety or depression, with a rating of 70% for overall health at 3 months post-surgery. At the 6th month, re-evaluation revealed a Harris hip score of 91.00, indicating an excellent outcome on the scale. The Oxford Hip score was 46 out of 48, indicating satisfactory joint function. He returned to his employment in the shop 4 months post-surgery. (Fig. 12-16).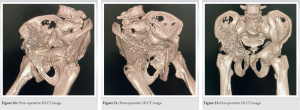
PDB, also known as osteitis deformans, is defined by a focal alteration in bone remodeling that results in a bone with an abnormal structure and altered mechanical properties, which causes pain and complications [8]. This disease may go undetected for many years and may be suspected in otherwise healthy individuals older than 55 years with an incidental finding of elevated serum ALP levels or a radiographic abnormality [9]. PDB is associated with pain, arthritis, deformities, and pathological fractures [6]. The most prevalent consequence of PDB is pathologic fracture, which may be disabling due to the high prevalence of non-union in pathological bone [6]. PDB is not very common below 55 years of age, as in this case. Isolated acetabular fractures remain an uncommon presentation as well. However, due to Paget’s disease, there are multiple difficulties during bone healing, along with early or accelerated arthritic changes already occurring in Paget’s. We did not find a specific consensus regarding the treatment of acetabular fractures due to Paget’s disease in the assessed literature. Although total hip arthroplasty would have been a good option because of protrusioacetabuli and already established arthritis, we adopted the treatment protocol for most acetabular fractures. The fracture was approached by Stoppa’s, and fixation was performed with screws and a plate with postoperatively monitored passive physiotherapy. The modified Stoppa method is an intrapelvic and extraperitoneal approach that enables for minimal invasive good reduction and fixation of displaced anterior column acetabular fractures with or without quadrilateral plate involvement, and the midterm outcomes have been favourable [10]. This resulted in a good range of motion and mobility at the hip joint, with 100–110° of flexion possible at the affected hip. However, simultaneously, due to high bone turnover and disease, and patients pre-operative arthritis and protrusioacetabuli of the hip joint, which may further deteriorate due to paget’s and eventually require arthroplasty. Uncontrolled disease activity hindered the natural union process and caused non-union in most fractures in Paget’s disease, but in this case, due to fixation, signs of union were present at the end of 3 months, along with a good clinical outcome.
Paget disease is a bone disease that can be asymptomatic at first and is discovered by chance during the evaluation of pathological fractures. Early fracture fixation with physiotherapy can result in good clinical outcomes in patients with acetabular fractures.
Although Paget’s disease is an uncommon accidental finding in trauma patients, early fixation of acetabular fractures in patients with Paget’s may improve clinical outcomes.
References
- 1.Laird A, Keating JF. Acetabular fractures: A 16-year prospective epidemiological study. J Bone Joint Surg Br 2005;87:969-73. [Google Scholar]
- 2.Eversole R, Su L, ElMofty S. Benign fibro‐osseous lesions of the craniofacial complex. A review. Head Neck Pathol 2008;2:177-202. [Google Scholar]
- 3.Selby PL, Davie MW, Ralston SH, Stone MD; Bone and Tooth Society of Great Britain; National Association for the Relief of Paget’s disease. Guidelines on the management of Paget’s disease of bone. Bone 2002;31:366-73. [Google Scholar]
- 4.Smith SE, Murphey MD, Motamedi K, Mulligan ME, Resnik CS, Gannon FH. Radiographic spectrum of Paget’s disease of bone and its complications with pathologic correlation. Radiographics 2002;22:1191-216. [Google Scholar]
- 5.Ralston SH, Langston AL, Reid IR. Pathogenesis and management of Paget’s disease of bone. Lancet 2008;372:155-63. [Google Scholar]
- 6.Shankar YU, Misra SR, Vineet DA, Baskaran P. Paget disease of bone: A classic case report. Contemp Clin Dent 2013;4:227-30. [Google Scholar]
- 7.Glaser DL, Kaplan FS. Orthopedic surgery considerations in Paget’s disease of bone. Clin Rev Bone Mineral Metab 2002;1:159-65. [Google Scholar]
- 8.Rai H, Pai SM, Dayakar A, Javagal V. A rare incident of Paget’s disease of bone in early adult life. J Oral Maxillofac Pathol 2014;18 Suppl 1:S147-50. [Google Scholar]
- 9.Ferraz-de-Souza B, Correa PH. Diagnosis and treatment of Paget’s disease of bone: A mini-review. Arq Bras Endocrinol Metabol 2013;57:577-82. [Google Scholar]
- 10.Tannast M, Keel MJ, Siebenrock KA, Bastian JD. Open reduction and internal fixation of acetabular fractures using the modified Stoppa approach. JBJS Essent Surg Tech 2019;9:e3. [Google Scholar]







