In septic arthritis cases, cultures dictate the proper treatment; hence, microbiological examination is of utmost importance, since it may reveal unusual organisms for which empirical treatment may prove insufficient.
Dr. Christos Koutserimpas, Department of Orthopaedics and Traumatology, “251” Hellenic Air Force General Hospital, Kanellopoulou Av, Athens 115 25, Greece. E-mail: chrisku91@hotmail.com
Introduction: Septic arthritis usually affects native joints and represents an invasion of the joint space by a wide variety of microorganisms, most commonly bacteria, such as Staphylococci, Streptococci, and Gram-negative rods. An extremely rare case of septic knee arthritis caused by Pantoea agglomerans in a 67-year-old male is presented.
Case Presentation: The patient was initially treated with arthroscopic debridement, but due to persistent symptomatology open surgical debridement 3 days after initial surgery was also performed. Cultures yielded P. agglomerans and Streptococcus agalactiae. He was commenced on causative antimicrobial treatment including intravenous linezolid, ciprofloxacin, and clindamycin. He was discharged 10 days later, on oral linezolid and ciprofloxacin for 3 months.
Conclusions: Delayed diagnosis in septic arthritis cases and inadequate control of the infection may lead to insufficient treatment and devastating consequences for the patient. The treatment includes surgical debridement and proper antimicrobial agents. Cultures dictate the proper treatment; hence, microbiological examination is of utmost importance, since it may reveal unusual organisms for which empirical treatment may prove insufficient.
Keywords: Native joint infection, knee infection, septic knee, synovitis, arthroscopic treatment, Pantoea agglomerans.
Septic arthritis is usually an acute monoarthritis of native joints and represents an invasion of the joint space by a wide variety of microorganisms, most commonly bacteria [1] . Septic arthritis requires urgent surgical and medical management, since it may have severe consequences, affecting the patient’s quality of life by destroying the articular surfaces of the affected joint [1]. Prompt diagnosis as well as treatment are of paramount importance for limiting the infection’s devastating results [1, 2]. The most common causative pathogens of septic arthritis are Staphylococci (56%), Streptococci (16%), and Gram-negative rods (15%). These bacteria possess highly destructive nature; therefore, bacterial septic arthritis maintains significant rates of morbidity and mortality even after immediate diagnosis and appropriate treatment [1, 2]. Pantoea agglomerans is an environmental Gram-negative aerobic bacillus of the family of Enterobacteriaceae. This pathogen may cause opportunistic wound and hospital-acquired infections in humans, while is most commonly isolated from plants and animals [3]. Septic arthritis due to P. agglomerans represents an extremely rare clinical entity, since only a few cases have been reported so far in the literature. In the present paper, an extremely rare case of knee septic arthritis due to P. agglomerans is presented. Furthermore, a thorough literature review is provided.
A 67-year-old male presented to the Emergency Department suffering painful right knee. His medical history was remarkable for diabetes mellitus, chronic kidney disease, and rheumatoid arthritis. On physical examination, the patient was hemodynamically stable (heart rate [HR]=75 beats per min (bpm), blood pressure [BP]=130/80 mmHg), and febrile (38℃).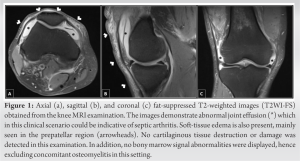 The right knee was swollen and warm, while skin lacerations were evident above the knee joint. of motion (ROM) was significantly restricted due to pain (flexion= 45°, extension=10°, and internal rotation=0°). After detailed medical history, the patient appeared to have recently performed agricultural activity where his lower limbs were widely exposed. Laboratory investigation revealed leukocyte count=15.500/cm2 with 89.5% neutrophils and C-reactive protein (CRP)=273 mg/dL. At that point, arthrocentesis of the knee joint was performed. Abundant yellow opaque fluid was aspirated and sent for urgent laboratory examination. Laboratory examination of the fluid showed 175.000 leukocytes/μL and 92% neutrophils, while Gram stain was positive for a Gram-positive pathogen. Magnetic resonance imaging (MRI) was then performed showing signs of knee joint infection (Fig. 1). At that point in time, urgent arthroscopic debridement under general anesthesia was performed and samples were acquired and sent for microbiological examination. Consequently, the patient was commenced on empirical antimicrobial treatment including intravenous (iv) vancomycin and ciprofloxacin. The patient remained febrile (37.5℃) the first 2 days following surgery with slight improvement of knee ROM. Peripheral blood leukocytes were 13.800/μL and CRP=220 mg/dL. Cultures revealed a vancomycin sensitive Streptococcus agalactiae. On the 3rd post-operative day, the patient’s general condition deteriorated becoming hemodynamically unstable (HR=110 bpm, BP=180 mmHg) and febrile (38.6℃), while the knee was warm, swollen, and tender. At that point, CRP reached 330mg/dL and leukocytes=16.300/μL. Open surgical debridement of the joint was then proposed and performed. Under general anesthesia, midline longitudinal skin incision followed by medial parapatellar arthrotomy was used to expose the joint. Meticulous debridement was performed and tissue specimens were sent for microbiological examination. Subsequently, lavage with 15 liters of normal saline concluded the procedure. The treatment with iv vancomycin and ciprofloxacin was continued. Two days after the 2nd surgery, the patient had regained most range of joint motion, was afebrile, while inflammatory laboratory profile was significantly improved (CRP=130 mg/dL and leukocytes=12.400/μL). In addition to the previously isolated S. agalactiae, tissue cultures yielded . agglomerans, resistant to cefoxitin, and fosfomycin. Antimicrobial treatment was switched accordingly, to iv linezolid, ciprofloxacin, and clindamycin. The patient remained in the hospital for 10 additional days, receiving iv antimicrobial treatment. On discharge, the affected knee had regained full ROM, without local signs of inflammation. CRP at that point was 30 mg/dL. The patient was discharged on linezolid and ciprofloxacin per os for 3 months. The patient is followed up for 12 months now. Oral antimicrobial treatment was discontinued 3 months after discharge. On final follow-up, the patient looks healthy without any signs or symptoms of an infection.
The right knee was swollen and warm, while skin lacerations were evident above the knee joint. of motion (ROM) was significantly restricted due to pain (flexion= 45°, extension=10°, and internal rotation=0°). After detailed medical history, the patient appeared to have recently performed agricultural activity where his lower limbs were widely exposed. Laboratory investigation revealed leukocyte count=15.500/cm2 with 89.5% neutrophils and C-reactive protein (CRP)=273 mg/dL. At that point, arthrocentesis of the knee joint was performed. Abundant yellow opaque fluid was aspirated and sent for urgent laboratory examination. Laboratory examination of the fluid showed 175.000 leukocytes/μL and 92% neutrophils, while Gram stain was positive for a Gram-positive pathogen. Magnetic resonance imaging (MRI) was then performed showing signs of knee joint infection (Fig. 1). At that point in time, urgent arthroscopic debridement under general anesthesia was performed and samples were acquired and sent for microbiological examination. Consequently, the patient was commenced on empirical antimicrobial treatment including intravenous (iv) vancomycin and ciprofloxacin. The patient remained febrile (37.5℃) the first 2 days following surgery with slight improvement of knee ROM. Peripheral blood leukocytes were 13.800/μL and CRP=220 mg/dL. Cultures revealed a vancomycin sensitive Streptococcus agalactiae. On the 3rd post-operative day, the patient’s general condition deteriorated becoming hemodynamically unstable (HR=110 bpm, BP=180 mmHg) and febrile (38.6℃), while the knee was warm, swollen, and tender. At that point, CRP reached 330mg/dL and leukocytes=16.300/μL. Open surgical debridement of the joint was then proposed and performed. Under general anesthesia, midline longitudinal skin incision followed by medial parapatellar arthrotomy was used to expose the joint. Meticulous debridement was performed and tissue specimens were sent for microbiological examination. Subsequently, lavage with 15 liters of normal saline concluded the procedure. The treatment with iv vancomycin and ciprofloxacin was continued. Two days after the 2nd surgery, the patient had regained most range of joint motion, was afebrile, while inflammatory laboratory profile was significantly improved (CRP=130 mg/dL and leukocytes=12.400/μL). In addition to the previously isolated S. agalactiae, tissue cultures yielded . agglomerans, resistant to cefoxitin, and fosfomycin. Antimicrobial treatment was switched accordingly, to iv linezolid, ciprofloxacin, and clindamycin. The patient remained in the hospital for 10 additional days, receiving iv antimicrobial treatment. On discharge, the affected knee had regained full ROM, without local signs of inflammation. CRP at that point was 30 mg/dL. The patient was discharged on linezolid and ciprofloxacin per os for 3 months. The patient is followed up for 12 months now. Oral antimicrobial treatment was discontinued 3 months after discharge. On final follow-up, the patient looks healthy without any signs or symptoms of an infection.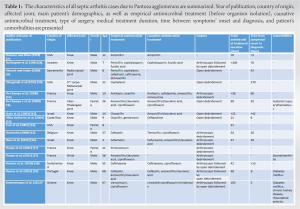
arthritis is a clinical entity requiring prompt diagnosis and management, as it may result in disability, affecting the patient’s quality of life, or even death [1]. Bacteremia seems to be the most usual cause, but this infection may also, occasionally, be the result of penetrating trauma, such as animal bites, plant thorns, and/or iatrogenic causes [1]. Microbiological examination is of paramount importance for definite diagnosis, while clinical examination plays major role in identifying these cases. The most common isolated causative pathogens include methicillin-sensitive Staphylococcus aureus (42%) and methicillin-resistant S. aureus (10%), as well as Streptococcal spp (16%) and Gram-negative rods (15%), while fungus may also cause septic arthritis in rare cases [1, 2, 4]. Such infections due to P. agglomerans are rare. The present study reports in detail such a case, while it provides a thorough literature review of all similar cases, evaluating their epidemiological characteristics, their diagnosis and therapeutic management, offering valuable insight for this rare infection. The treatment of this infection requires combination of surgical debridement and proper antimicrobial agents according to sensitivity microbiological examination. In most cases, due to the severity of the disease, empirical treatment including anti-staphylococcal drugs is required until the cultures’ results [1, 2]. P. agglomerans is a Gram-negative bacterium that belongs to the family of Erwiniaceae and is part of a highly versatile group of approximately 20 different Pantoea spp [4]. There is not yet clear discrimination between pathogenic and not- pathogenic Pantoea spp to humans [4, 5, 6]. P. agglomerans represents an opportunistic, slow-growing human pathogen. It is rarely reported to cause septic arthritis, while it is usually related to vegetation and less likely to soil, water and animal feces. Infections are typically acquired through skin penetration from plant components, such as plant thorns and wooden splinters during agricultural activities or in more rare cases through contaminated intravenous fluids and blood products during hospitalization [5]. P. agglomerans is reported to cause various infections, such as endophthalmitis, endocarditis, periostitis, peritonitis following peritoneal dialysis, liver abscesses, and spondylodiscitis. It is of note that immunosuppressed hosts are more susceptible to P. agglomerans septicemia [5]. A thorough electronic literature review, including the PubMed and EMBASE databases was also conducted for all septic arthritis cases caused by P. agglomerans. A total of 15 additional cases are identified. Table 1 highlights the main characteristics of these cases. Including the reported case, a total of 16 septic arthritis cases exist in the literature (Table 1) [7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19]. The age of the patients ranged from 4 to 68 years with mean age=30.5 years (standard deviation [SD]=24), while most patients were male (81.25%). Most commonly affected joint was the knee (12 cases; 75%), followed by the radiocarpal, carpometacarpal, interphalangeal, and wrist joint (1 case each; 6.25%). Furthermore, penetrating trauma or skin laceration by a thorn plant was mentioned in the majority of the cases (14 cases; 87.5%), while in 6 (37.5 %), inoculated plant material, most commonly thorn debris, was identified during the surgical intervention [18]. present case was also male and was involved in agricultural activities before symptoms’ onset. It is of note that in this case, no thorn debris was found during surgery. Nevertheless, he had evident skin lacerations over the knee joint. According to the available literature, definite diagnosis of septic arthritis caused by P. agglomerans is often delayed [18]. Inappropriate growth media and insufficient identification methods could be responsible for the difficulty in isolation of this bacillus. Mean interval between symptoms onset and P. agglomerans identification is 44.8 days (SD=70.9). This delay may result in serious, irreversible joint damage and prolonged treatment. Therefore, diligent attention should be given to medical history with targeted questions and high index of suspicion is required in cases that agricultural activities are mentioned. In such cases, more suitable culture mediums and higher sensitivity screening methods should be considered. BACTEC Peds Plus F broth is suggested to have better results than conservative growth media, while broad spectrum 16S rDNA polymerase chain reaction may identify Pantoea species when other media have not [11, 12, 16, 19]. Various broad-spectrum medications have been used in different combinations for the initial empirical treatment of P. agglomerans septic arthritis, while β-lactam antibiotics were the most frequently used, as shown in Table 1. In most occasions (13 cases; 81.25%), a penicillin derivative with or without β-lactamase inhibitor or cephalosporin was empirically given, while gentamicin and pristinamycin were given in two cases (12.5%). Initial medical treatment may have led to temporary improvement of symptoms, but, eventually, the infection persisted and surgical intervention was mandatory. Following the identification of P. agglomerans and susceptibility testing, the treatment was not considerably modified as the bacillus seems to develop low resistance to common antimicrobials. It is of note that in four cases (25%) quinolones proved to be an effective antimicrobial agent. Total antimicrobial treatment duration ranged from 21 to 106 days with average of 52.6 days (SD=32.4). Septic arthritis requires prolonged antimicrobial treatment, until eradication of all signs and symptoms of the infection. Laboratory examination, including CRP, also plays important role not only in the initial diagnosis but also during the course of medical treatment. Definitive treatment may be very challenging due to an occult foreign body [16, 18]. In the present case, there was no sign of thorn; however, in six of the reviewed cases (37.5%), plant material was found during surgical debridement and its extraction was necessary for definitive control of the infection. Plant debris may remain entrapped and undiscovered even for months [7, 8, 10, 12]. Thus, awareness of this possibility and consequently aggressive, as well as meticulous surgical exploration of the joint is of utmost importance. In the presented case, in addition to P. agglomerans, S. agalactiae was also cultured from the synovial joint fluid and the tissue specimens. infection of a native joint with P. agglomerans and another bacterium has not been reported so far, making this case unique. It is of note that after the initial arthroscopic surgery, only S. agalactiae was yielded. However, due to persistent symptomatology, open debridement was subsequently performed, while microbiological examination then, additionally, revealed P. agglomerans leading to proper antimicrobial treatment and the infection’s eradication. It should be noted that from the nine total cases that arthroscopic debridement was performed, in four of them (44.4%), open exploration of the joint was later necessary.
Septic arthritis due to P. agglomerans is an established clinical entity and is highly associated with agricultural activity and penetrating trauma from vegetation. Accurate medical history and high index of suspicion are of paramount importance for prompt diagnosis and appropriate treatment initiation. In addition to causative antimicrobial agents, early surgical debridement with extensive search for plant material or other foreign body seems to be mandatory to succeed complete infection control and infection’s eradication.
Septic arthritis represents an urgent clinical entity requiring prompt diagnosis and treatment. Microbiological examination is of utmost importance for causative medical management, while surgical intervention is the cornerstone of management. Septic arthritis due to P. agglomerans is highly associated with agricultural activity and penetrating trauma from plants. Detailed medical history and high index of suspicion are essential for the identification and eradication of this infection.
References
- 1.Ross JJ. Septic arthritis of native joints. Infect Dis Clin North Am 2017;31:203-18. [Google Scholar]
- 2.Samonis G, Koutserimpas C, Vrioni G, Kampos Martinez E, Kouloumentas P, Alpantaki K, et al. Fungal septic knee arthritis caused by Aspergillus fumigatus following anterior cruciate ligament reconstruction. Diagnostics (Basel) 2021;11:1975. [Google Scholar]
- 3.Walterson AM, Stavrinides J. Pantoea: Insights into a highly versatile and diverse genus within the Enterobacteriaceae. FEMS Microbiol Rev 2015;39:968-84. [Google Scholar]
- 4.Koutserimpas C, Chamakioti I, Naoum S, Raptis K, Alpantaki K, Samonis G. Native joint infections by Aspergillus species. Diagnostics (Basel) 2021;11:2335. [Google Scholar]
- 5.Dutkiewicz J, Mackiewicz B, Kinga Lemieszek M, Golec M, Skórska C, Milanowski J, et al. Pantoea agglomerans: A mysterious bacterium of evil and good. Part III. Deleterious effects: Infections of humans, animals and plants. Ann Agric Environ Med 2016;23:197-205. [Google Scholar]
- 6.Rezzonico F, Smits TH, Montesinos E, Frey JE, Duffy B. Genotypic comparison of Pantoea agglomerans plant and clinical strains. BMC Microbiol 2009;9:204. [Google Scholar]
- 7.Flatauer FE, Khan MA. Septic arthritis caused by Enterobacter agglomerans. Arch Intern Med 1978;138:788. [Google Scholar]
- 8.Strömqvist B, Edlund E, Lidgren L. A case of blackthorn synovitis. Acta Orthop Scand 1985;56:342-3. [Google Scholar]
- 9.Vincent K, Szabo RM. Enterobacter agglomerans osteomyelitis of the hand from a rose thorn. A case report. Orthopedics 1988;11:465-7. [Google Scholar]
- 10.Olenginski TP, Bush DC, Harrington TM. Plant thorn synovitis: An uncommon cause of monoarthritis. Semin Arthritis Rheum 1991;21:40-6. [Google Scholar]
- 11.De Champs C, Le Seaux S, Dubost JJ, Boisgard S, Sauvezie B, Sirot J. Isolation of Pantoea agglomerans in two cases of septic monoarthritis after plant thorn and wood sliver injuries. J Clin Microbiol 2000;38:460-1. [Google Scholar]
- 12.Kratz A, Greenberg D, Barki Y, Cohen E, Lifshitz M. Pantoea agglomerans as a cause of septic arthritis after palm tree thorn injury; Case report and literature review. Arch Dis Child 2003;88:542-4. [Google Scholar]
- 13.Ulloa-Gutierrez R, Moya T, Avila-Aguero ML. Pantoea agglomerans and thorn-associated suppurative arthritis. Pediatr Infect Dis J 2004;23:690. [Google Scholar]
- 14.Cruz AT, Cazacu AC, Allen CH. Pantoea agglomerans, a plant pathogen causing human disease. J Clin Microbiol 2007;45:1989-92. [Google Scholar]
- 15.Duerinckx JF. Case report: Subacute synovitis of the knee after a rose thorn injury: Unusual clinical picture. Clin Orthop Relat Res 2008;466:3138-42. [Google Scholar]
- 16.Rave O, Assous MV, Hashkes PJ, Lebel E, Hadas-Halpern I, Megged O. Pantoea agglomerans foreign body-induced septic arthritis. Pediatr Infect Dis J 2012;31:1311-2. [Google Scholar]
- 17.Fianyo E, Guignard S, Economu A, Thellier N, Davidowicz K, Chevalier X. Thorn synovitis: Report of 2 cases. Rev Med Interne 2015;36:426-9. [Google Scholar]
- 18.Koester T, Kusano T, Eijer H, Escher R, Waldegg G. Septic arthritis of the knee due to Pantoea agglomerans: Look for the thorn. J Bone Jt Infect 2020;6:51-5. [Google Scholar]
- 19.Ramos JT, Barbosa N, Almeida J, Karmali S, Guerreiro R, Magalhães G. Knee septic arthritis after palm tree thorn injury: A case report. J Orthop Case Rep 2021;11:13-5. [Google Scholar]










