Paediatric Agricultural Polytrauma Injuries are challenging and are better managed at a tertiary care center through multidisciplinary approach; In facial avulsion injuries, the surgical airway is safest and in the presence of compound tibia fracture with extensive degloving, the orthoplastic approach reduces the number of unnecessary interventions and improves outcomes.
Dr. Vivek M Sodhai, Department of Paediatric Orthopaedics, King Edward Memorial Hospital and Research Centre, Pune - 411 011, Maharashtra, India. E-mail: vivek.sodhai89@gmail.com
Introduction: Agricultural polytrauma injuries in children are rare. Rotating blades of a tractor can cause devastating injuries.
Case Report: An 11-year-old male child presented with severe facial avulsion injuries, degloving injury of left lower limb, grade IIIB compound left tibia shaft fracture with a large butterfly fragment, and closed right tibia shaft fracture. General anesthesia through tracheostomy intubation was given. Simultaneous surgical intervention for the face and limbs was performed by a team of experts. The facial injury was debrided and repaired. After thorough debridement, compound left tibia fracture fixation was performed with two interfragmentary screws and neutralizing ankle-spanning external fixator. The closed right tibia shaft fracture was treated with closed elastic intramedullary nailing. Simultaneous debridement of degloving injuries over both thighs was performed and wound closure was done. Subsequently, the patient underwent debridement of wounds and vacuum-assisted closure 3 times with split skin grafting for the left leg. All fractures healed well at 6 months and the child was able to do all activities without any functional limitations.
Conclusion: Agricultural injuries in Children can be devastating and should be managed using a multidisciplinary approach at a tertiary care center. A tracheostomy is a viable option for securing the airway in severe facial avulsion injuries. In a hemodynamically stable child, definitive fixation can be performed in a polytrauma situation and an external fixator can be used as a definitive implant in an open long bone fracture.
Keywords: Agricultural injury, compound fracture, external fixation, facial avulsion injury, orthoplastic approach, pediatric polytrauma.
Agricultural injuries are an important cause of morbidity and mortality in the pediatric population. Most of these injuries occur in children not actively involved in farm work. Many of these injuries occur due to by standing or an extra rider on an agricultural vehicle. The use of agricultural mechanical machinery has increased all over the world to get more production and reduce labor costs. This has also increased the incidence of lethal accidents in agriculture leading to increased morbidity and mortality [1, 2]. The reasons are sharp and rotating parts of the machines, untrained machine operators, limited safety and professional knowledge, addictions like smoking and alcohol consumption at work, carelessness, etc. [1, 2]. The commonly used agriculture machines are rotavators, wheat/maize threshers, fodder choppers, and sugarcane juice extractors. The rotating blades are the common culprit leading to fractures, degloving injuries, bleeding, and amputations often leading to a critically ill patient or even death. Such poly-traumatized patients should receive appropriate and timely care at a tertiary care center. Agricultural injuries are common in males above 40 years of age with lower extremities getting affected commonly followed by upper extremities, torso, face, and head [1]. Agriculture-induced polytrauma injuries are rare in children but not unknown. A multidisciplinary team involving experts from various fields of medicine trained in treating these injuries should work together for the best outcome. We report a case of an 11-year-old child caught in the blades of a rotavator leading to a polytrauma injury involving facial avulsion, bilateral tibial fractures, and degloving injuries over both lower limbs. We intend to highlight the management challenges involved in this case. The patient was informed that the case would be published and written informed consent was taken.
An 11-year-old male child weighing 30 kg was brought to our emergency medicine department with a history of entanglement in the blades of the rotavator 8 h ago. There was no history of loss of consciousness or vomiting after the accident. Pediatric advanced life support protocol was utilized and a primary survey was conducted. There was no derangement in the airway, breathing, or circulation. He was conscious, oriented, and following commands with a Glasgow coma score of 15/15. He has hemodynamically stable on general examination. On the secondary survey, facial avulsion injuries, bilateral tibial fractures, and degloving injuries to both lower limbs were noted. Injuries are detailed further in the text. The child had complete avulsion injury of the nasal bones and nasal septum from the glabella in the anterior 1/3 continuing with an inferiorly based flap to upper lips and both the cheeks, the cartilaginous septum was separated from the white perpendicular plate of the ethmoid, the left medial canthus ligament was torn shifting it downward, degloving injury of the face (Fig. 1). A contaminated lacerated wound (CLW) over the right lower quadrant measuring 8 × 2 cm was noted. CLWs over the right inguinal region and right lower leg measuring 15 × 4 cm and 5 × 4 cm respectively were noted (Fig. 2a). Multiple extensive degloving injuries were noted over the left groin, thigh, leg, and foot (Fig. 2b and c).
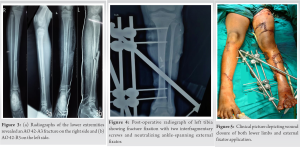
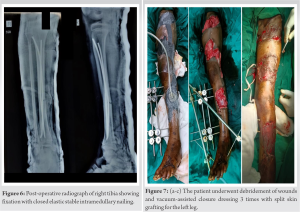
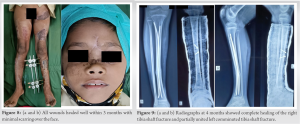
Maxillofacial injuries in polytrauma patients are very challenging due to the high vascularity of the face. The proximity and injuries of the upper airway, cranium, cervical structures, and spine can make it complicated [3]. An accurate initial assessment is very important for the management of airway, hemorrhage, and visual loss and should follow ATLS guidelines [4, 5]. The injuries in the middle third of the face can compromise the airway significantly due to fractures of the paranasal sinuses, zygoma leading to intraoral tissue injuries and bleeding, breaking of teeth, foreign bodies in the oral cavity, tissue edema, glottic edema, and aspiration leading to airway obstruction [3, 4]. The look, listen, and feel strategy helps to judge airway obstruction and anticipate airway complications [3]. Nowadays, a variety of different techniques are available for securing airways none being definitive. Hence, it should be tailor-made according to the situation. Please re-phrase this sentence and mention the different techniques in detail. High-volume suction should be available to keep the mouth and airway clear [3]. In our case, there were certain challenges related to anesthesia and the management of musculoskeletal injuries. First, there was complete avulsion injury of nasal bones and septum in the anterior 1/3 and the segment of the nose with the face was moving in synchronization with the movements of the jaw. Second, due to the difficulty in the examination of the oral cavity, there were no details of any intraoral injuries, swallowed blood, or intraoral edema. In this situation, inserting a nasogastric tube and nasotracheal intubation was impossible. Therefore, the patient had to be treated as a full stomach patient and a decision of surgical airway through tracheostomy was taken. In facial avulsion injuries, orotracheal intubation is challenging and the surgical airway is preferred [3]. Pediatric polytrauma injuries are rare and the care provided should be catered to by giving special consideration to the developing physiology of the child. In presence of severe open fractures, the child should be managed at a center, with the provision of a pediatric orthopedic surgeon and plastic surgeon working together to give an orthoplastic approach. This approach reduces the number of unnecessary interventions and improves outcomes [6]. Compared to adults, pediatric patients have a significant capacity to heal faster from severe musculoskeletal injuries. Hence, they should be treated with the consideration that the child will recover completely and walk without any deformation or functional limitation. Unacceptable reduction and inadequate stability should not be justified by a polytrauma scenario [7]. The optimal timing of fracture fixation in the pediatric population is not well defined. However, several studies in pediatric patients have shown that definitive stabilization within 3 days of injury has improved outcomes and reduces hospital stays [7, 8]. External fixation has a documented role in open tibial fractures [9], whereas elastic intramedullary nailing can be used in selected Grade II and IIIA open tibial fractures with limited contamination [10]. Our patient had a Gustilo-Anderson grade IIIB multi-fragmentary fracture of the left tibia-fibula with multiple extensive CLW from groin to toe and a closed transverse fracture of the right tibia with a clean lacerated wound over distal shin not communicating with the fracture and a CLW over the right groin. Thorough irrigation and debridement of the compound left tibia fracture and foot wound was performed with 6 liters of normal saline, diluted betadine, and hydrogen peroxide. Fractured ends were thoroughly cleaned. There is no ideal implant in presence of an open wound and a large butterfly fragment. Using the AO guidelines, we decided to perform fixation with two interfragmentary screws for the butterfly fragment neutralized with a biplanar ankle-spanning external fixator. Simultaneous debridement of degloving injuries over both thighs was performed with 6 liters of normal saline, diluted betadine, and hydrogen peroxide. After the fixation by the orthopedic specialist, wound closure was done by the plastic surgeon. The right tibia shaft transverse fracture was treated with closed elastic intramedullary nailing. Definitive fixation was performed for all fractures in a single stage. Because of early intervention, intravenous antibiotics, and thorough debridement, we were able to avoid infection in our case. The compound fracture healed well with an external fixator without any requirement for an additional procedure for definitive fixation. We believe that our case is unique in terms of the mechanism and pattern of injuries. It highlights the challenges that can manifest in a child with agricultural injury. Decision-making in such injuries is important. Taking a multidisciplinary approach including an orthoplastic approach goes a long way in saving a child’s life. Since there are no definitive strategies for managing agricultural polytrauma injuries in children, our case can add to the existing literature and allow us to formulate a definitive strategy.
Agricultural injuries in children can be devastating and should be managed using a multidisciplinary approach at a tertiary care center. A tracheostomy is a viable option for securing the airway in severe facial avulsion injuries. In a hemodynamically stable child, definitive fixation can be performed in a polytrauma situation and an external fixator can be a definitive treatment modality in open tibia shaft fractures.
In facial avulsion injuries, the surgical airway is safest. Nasal septal repair with bilateral internal nasal splints helps in healing without intranasal adhesions. In presence of compound tibia fracture with extensive degloving, the orthoplastic approach reduces the number of unnecessary interventions and improves outcomes. Furthermore, an external fixator can be used as a definitive fixation method in compound tibia fractures.
References
- 1.Paschos KA, Boulas K, Bogiatzis I, Chatzigeorgiadis A. Perineal and lower extremity severe injuries in accident with agricultural machinery-a case report. ARC J Clin Case Rep 2018;4:12-5. [Google Scholar]
- 2.Lodhi MF, Yaqoob M, Pervaiz K, Irfan S, Akram M, Durechaman, et al. Agricultural machine injuries-a significant cause of morbidity. Pak J Med Health Sci 2015;9:685-8. [Google Scholar]
- 3.Jose A, Nagori SA, Agarwal B, Bhutia O, Roychoudhury A. Management of maxillofacial trauma in emergency: An update of challenges and controversies. J Emerg Trauma Shock 2016;9:73-80. [Google Scholar]
- 4.Arslan ED, Solakoglu AG, Komut E, Kavalci C, Yilmaz F, Karakilic E, et al. Assessment of maxillofacial trauma in emergency department. World J Emerg Surg 2014;9:13. [Google Scholar]
- 5.Tuckett J, Warnke P, Lynham A. Maxillofacial trauma. Aust Fam Physician 2012;41:172-80. [Google Scholar]
- 6.Peterson N, James L. Polytrauma in children. Surgery (Oxford) 2020;38:560-6. [Google Scholar]
- 7.Jakob H, Lustenberger T, Schneidmuller D, Sander AL, Walcher F, Marzi I. Pediatric polytrauma management. Eur J Trauma Emerg Surg 2010;36:325-38. [Google Scholar]
- 8.Pandya NK, Upasani VV, Kulkarni VA. The pediatric polytrauma patient: Current concepts. J Am Acad Orthop Surg 2013;21:170-9. [Google Scholar]
- 9.Nandra RS, Wu F, Gaffey A, Bache CE. The management of open tibial fractures in children: A retrospective case series of eight years’ experience of 61 cases at a paediatric specialist centre. Bone Joint J 2017;99B:544-53. [Google Scholar]
- 10.Hong P, Rai S, Tang X, Liu R, Li J. External fixation versus elastic stable intramedullary nailing in the treatment of open tibial shaft fractures in children. J Orthop Surg Res 2021;16:528. [Google Scholar]