Total hip arthroplasty in presence of an ipsilateral knee arthrodesis can be safely performed through a direct anterior approach.
Dr. Louis Follet, Department of Orthopaedics, Resident UZ Leuven, Belgium. E-mail: follet.lf@gmail.com
Introduction: We present a case report of a total hip arthroplasty (THA) in a patient with ipsilateral knee arthrodesis. The direct anterior approach (DAA) was used, and to our knowledge, this has never been described previously in the literature. The purpose of this report is to highlight pre-, per-, and post-operative challenges using the DAA in these rare cases.
Case Report: This case report presents the case of a 77 year old female patient with degenerative hip disease in the presence of an ipsilateral arthrodesis of the knee. The patient was operated using the DAA. No complications were found and the patient had an excellent follow-up with a forgotten joint score of 93.75 at 1 year. The difficulty in this case consists in finding the correct stem anteversion with the altered knee anatomy. Using pre-operative templating on X-rays, intraoperative fluoroscopy and the posterior femoral neck the hip biomechanics could be restored.
Conclusion: We believe that THA in presence of an ipsilateral knee arthrodesis can be safely performed through a DAA.
Keywords: THA, DAA, knee arthrodesis.
Total hip arthroplasty (THA) with ipsilateral knee arthrodesis is a rare combination [1]. Especially as knee arthrodesis is less frequently performed. An arthrodesis of the knee alters the gait and the biomechanics of the hip. Walking speed is affected, and range of motion (ROM) reduced (especially the extension moment of the hip) [2]. The presence of a fused knee impacts the intraoperative positioning during a THA. When performing a DAA THA on a standard operating table, some degree of flexion of the knee is used to obtain a figure of four positions and to determine the intended anteversion of the femoral stem [3]. Of course, with a fused knee, the figure of four positions is not possible, and therefore, the question rose at our department if it is at all feasible and safe to perform this kind of surgery through the DAA. By our knowledge, this was not previously described in the literature to date. The importance of a well-positioned femoral component cannot be underestimated. It has been well demonstrated that a mal positioned femoral component leads to higher rates of dislocations, wear, and impingement. It is also associated with decreased ROM [4, 5]. The next question for us was, if we could reliably determine the correct anteversion of the femoral stem in the DAA, given the impossibility to perform the usual figure of four positioning.
A 77-year-old lady presented with progressive left groin pain, due to degenerative hip osteoarthritis. In the ipsilateral leg, she had a previous knee arthrodesis, as a result of a traffic accident during childhood (Fig. 1). She presented with a leg length discrepancy at the expense of the left leg of 8.5 cm, corrected by an orthopedic shoe. Clinically, there was no Trendelenburg limp. Log roll and rotation with the hip in flexion (and knee in extension) were painful, with a limited rotation. Radiographs of the pelvis and the left hip showed left hip osteoarthritis (Fig. 2).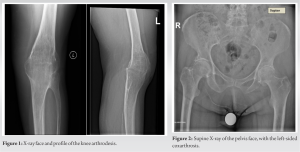
Surgical technique
The surgery was performed by an experienced, fellowship-trained anterior hip surgeon (KL). The patient was positioned supine on a regular operation room (OR) table. An extra padded cushion was placed at the contralateral side just above the ankle, and a side support was placed at the contralateral trochanteric region. Both legs were completely disinfected and draped, so a transepicondylar Steinmann pin could be drilled when needed. A 9 cm longitudinal incision was made two fingerbreadths distal and three lateral from the anterior superior iliac spine, aiming for the fibular head. Subcutaneous dissection was performed on the tensor fascia latae muscle. The fascia was incised in the muscular zone (red zone), medial from the perforating vessels, and lateral from the lateral cutaneous femoral nerve. Next, the plane between tensor fascia latae muscle laterally, and sartorius and rectus femoris muscle medially was bluntly dissected. The innominate fascia was split in line with the incision and the ascending branches of the lateral femoral circumflex artery were coagulated. After capsular exposure, an inverted T-shaped capsulotomy was performed and the retractors were placed intracapsular. The femoral neck cut was made according to the digital templating (Orthoview® – Materialize UK, Southampton, UK). Subsequently, an uncemented cup with a neutral polyethylene liner was implanted. Next, femoral releases were performed until adequate femoral access was achieved. As a classic figure of four positions of the leg was impossible due to the knee arthrodesis, the femoral was more extensive than for a standard primary THA. First, the inferomedial release was performed down to the lesser trochanter and followed by the superior release up to the external obturator tendon [7, 8, 9]. A retractor was placed between the gluteal musculature and the greater trochanter. With a bone hook, the femur was lifted and pulled anteriorly and laterally. The ipsilateral leg was moved in adduction and external rotation and was carefully positioned on the cushion under the contralateral leg (Fig. 3). Although the use of a Steinmann pin through the distal femur was anticipated, this was not necessary as manual manipulation was sufficient. The calcar was exposed by placing a retractor medially. As the proximal femoral anatomy was normal, the posterior border of the femoral neck, the lesser trochanter, and calcar were used as a guide for the femoral anteversion. Furthermore, the remnant epicondyles of the knee were palpable and could also function as extra landmarks for the femoral anteversion. The targeted anteversion was 10°. A trial reduction with a high offset neck and a short head yielded a good ROM and a stable hip joint in all directions. Fluoroscopy was used to check offset, leg length, and femoral stem sizing and positioning. The leg was lengthened by 2 cm, but remained 6.5cm short compared to the contralateral side. Even if it would have been possible, attention would have been paid not to have an equal leg length, which could lead to difficulties during the swing phase as result of the knee arthrodesis (Fig. 4) Finally, a flat tapered wedge cemented stem (Taperloc® – ZimmerBiomet, Inc, Warshaw, IN), with a 32 mm ceramic head (Biolox Delta®, CeramTec, Germany). After thorough lavage standard wound closure was performed including capsular closure included and intradermal skin closure. Postoperatively, the patient was mobilized out of bed the same day, with full weight-bearing with two crutches, according to our institutional Rapid Recovery® protocol. Post-operative X-rays showed satisfactory position of the hybrid hip replacement (Fig. 5). She was discharged on day 3 postoperatively, after meeting the discharge criteria: dry wound dressings, adequate pain control and able to do transfers, and climbing a few stairs. She was seen at the outpatient clinic at 1 month, 4 months, and 1 year postoperatively. The groin pain had completely disappeared, and she had a normal gait. The patient was very satisfied with a forgotten joint score of 93.75 out of 100 at 1 year follow-up [10, 11].
This case demonstrates that THA in patients with ipsilateral knee arthrodesis is possible using a DAA on a regular OR table, with only small adjustments to the standard operative technique. Furthermore, we can demonstrate that the technique proved to be safe in this case, yielding an excellent result without complications. In the only case series that we have found about the combination of THA and ipsilateral knee arthrodesis, Bourne et al. [1] describe no intraoperative complications in their series of eight patients in which the arthroplasty was performed after the knee arthrodesis. They used mainly lateral or posterior approaches, but no anterior approach was used. The biggest technical difficulty was the dislocation of the femoral head, due to the difficult manipulation of the long lever arm of the leg. Therefore, they suggested cutting the femoral neck before dislocation. In the DAA, the neck cut is always done first, before removing the femoral head. Therefore, with the DAA, we can eliminate the most important technical difficulty that was described in their series. In this case, the main difficulty was indeed the intraoperative positioning of the leg, which needed to be slightly modified. Mainly the figure of four positioning needed to be replaced by manual manipulation of the extended leg. We were prepared for placement of an optional transepicondylar Steinmann pin for manipulation and visual orientation, as the femoral anteversion could not be relied on a flexed knee during broaching of the femur. Eventually, the Steinmann pin was not necessary. In our opinion, the key was the extensive capsular release of the proximal femur, to achieve easy femoral access without increasing the stress on the distal femur and knee arthrodesis. This release is routinely performed in all our difficult cases, to minimize stress on the femur while broaching. We performed an inferomedial release from the calcar down to the lesser trochanter and a superior release (conjoined tendon and piriformis) as described in the literature [7, 8, 9]. After this release, gentle positioning of the extended leg was rather easy. An extended approach like it is used in anterior revision surgery was not necessary in this case. This option was considered as the next step, in case that capsular release would not have been sufficient [12]. Apart from the technical challenges and risk of intraoperative complications, we were concerned about the risk of post-operative dislocation. In contrast to the well-established higher dislocation risk in patients with lumbar spine fusion [13], we do not know if there is a higher risk in knee arthrodesis patients. Although Bourne et al. [1] report no dislocations in their series, the number of patients was very low to make hard conclusions. Theoretically, one could suggest that with a stiff knee, it is very difficult to achieve an extreme flexion and internal rotation moment of the hip, and therefore, the risk of posterior hip dislocation could possibly be lower. One of the advantages of the DAA is the very low dislocation rate [14]. In this case, we used a DAA on a regular OR table, with the patient in supine position and both legs draped. With this technique, leg length can be measured accurately, and hip stability can be tested during surgery, in all directions. Together with the reported low dislocation risk, we feel that this technique gives the surgeon a lot of control and confidence during surgery. Moreover, using fluoroscopy, we can confirm cup position and the anatomical reconstruction of length and lateral offset. Another important factor that adds to the stability of the hip prosthesis is the position of the femoral component, more specifically the version. A low combined anteversion is associated with posterior dislocation, whereas a high combined anteversion is associated with anterior dislocation [15]. Due to the ipsilateral knee arthrodesis, a “classic” figure of four positioning of the leg was not possible. This could possibly complicate the intraoperative definition of the correct femoral anteversion. In their case report, Patii et al. describe a Kocher Langenbeck approach for a cemented hemiarthroplasty [6]. The confirmation of the femoral anteversion was based on the goniometric angle made between a horizontal flat patella and the disappearance of the lesser trochanter on fluoroscopy of the contralateral leg. This angle was copied to the ipsilateral leg by drilling a Steinmann pin into the fused knee when the lesser trochanter disappeared on fluoroscopy. In our opinion, we think that their method was quite complex, and we are concerned about the accuracy and reproducibility of this technique. In the presence of the knee arthrodesis, an estimation of the transepicondylar axis must be made by palpating the knee. In this case, both the femoral epicondyles were palpable and were also still visible on a pre-operative radiograph. On the other hand, as a figure of four was not possible due to the knee arthrodesis, a visual estimation of the anteversion was still more difficult. This axis could possibly have been visualized better using a transepicondylar Steinmann pin, but we felt that in this case, it would not add more value. Moreover, it could possibly create a stress riser in the metaphyseal bone, with higher risk for perioperative fracture around the knee. In case that the normal anatomy of the knee is changed, and thus, the transepicondylar axis is less obviously defined, the femoral version should preferably be identified based on other landmarks. With the DAA, this is perfectly possible based on the proximal femoral anatomy. In this case, the proximal femoral anatomy proved to be normal, both preoperatively radiographically, as during surgery. Therefore, the posterior border of the femoral neck cut, the lesser trochanter, and the calcar were helpful as landmarks for the version of the implanted stem, as described by Mohamed et al. and Yun et al. [16, 17]. When using an uncemented femoral stem, the femoral version is mainly determined by proximal femoral canal anatomy [18, 19]. The femoral version is less adaptable than with a cemented stem. Therefore, the combined version of the acetabular and femoral component needs to be taken into account (20–50°) as described by Dorr et al. [20] Jackson et al. showed a good reliability of the femoral version using a direct anterior approach (DAA) to the hip [19]. In our case, it was decided preoperatively to use a cemented stem for two main reasons. First, a cemented stem could give us more options regarding the femoral version and leg length. Second, we wanted to anticipate possible pore bone quality as a result of different biomechanics, due to the knee arthrodesis. A pre-operative computed tomography (CT) could have given us more information about the proximal femoral anatomy. On the other hand, pre-operative radiographs showed a normal bone quality and a Dorr B proximal femur, and it was decided not to perform a CT in this case [21]. Interestingly, a pre-operative 3D CT planning with CT does not guarantee a perfect femoral version as Belzunce et al. described [22]. Finally, given the importance of an optimal functioning hip joint to compensate for the knee arthrodesis, we pursued an anatomical reconstruction of the hip joint. We believe that intraoperative fluoroscopy can be an excellent guide to restore the anatomy, especially when using a DAA. Martin et al. concluded that the anatomy is better restored in a DAA when using fluoroscopy, compared to the posterior approach [23]. Moreover, Boe et al. stated that using hip templating, restoring the anatomy and biomechanics can be achieved, and in combination with adequate soft-tissue balancing, a stable and ideal arthroplasty can be the result [24].
This case report shows that a THA using a DAA is possible in patients with an underlying ipsilateral knee arthrodesis. Extensive femoral releases may be necessary to achieve good positioning of the leg to give adequate access to the femoral canal. In the presence of a normal knee joint, the femoral anteversion is defined by the figure of four position of the lower leg during broaching. As this cannot be used in case of an ipsilateral knee arthrodesis, alternative landmarks such as the posterior neck cut, calcar, and lesser trochanter can be helpful. This case showed an excellent result, with no intraoperative or post-operative complications.
THA performed by a DAA is a possible, safe, and stable solution in patients with an ipsilateral knee arthrodesis.
References
- 1.Bourne MH, Fox DL, Morrey BF. Long-term evaluation of hip arthroplasty in patients with an ipsilateral knee arthrodesis. Clin Orthop Relat Res 1993;289:170-4. [Google Scholar]
- 2.Wagener N, Böhle S, Kirschberg J, Rohe S, Heinecke M, Di Fazio P, et al. Knee arthrodesis affects gait kinematics more in the ankle than in the hip joint. Medicina (Kaunas) 2022;58:696. [Google Scholar]
- 3.Mayr E, Thaler M, Williams A, De La Barrera JM, Krismer M, Nogler M. The figure-of-four axis as a reference to determine stem rotation in hip arthroplasty. What does it really measure? A cadaver study. Acta Orthop 2007;78:458-62. [Google Scholar]
- 4.Brown TD, Elkins JM, Pedersen DR, Callaghan JJ. Impingement and dislocation in total hip arthroplasty: Mechanisms and consequences. Iowa Orthop J 2014;34:1-15. [Google Scholar]
- 5.Worlicek M, Weber M, Craiovan B, Wörner M, Völlner F, Springorum HR, et al. Native femoral anteversion should not be used as reference in cementless total hip arthroplasty with a straight, tapered stem: A retrospective clinical study. BMC Musculoskelet Disord 2016;17:399. [Google Scholar]
- 6.Patii ND, Patel HB, Hussain N, Saidane K. Cemented hemiarthroplasty of the hip in a patient with ipsilateral knee arthrodesis: Surgical difficulties and techniques. J Orthop Case Rep 2018;8:75-9. [Google Scholar]
- 7.Corten K, Vanbiervliet J. Acetabular Exposure in the Efficient Direct Anterior THA International Congress for Joint Reconstruction; 2022. Available from: https://www.icjr.net/articles/acetabular-exposure-in-the-efficient-direct-anterior-tha [Last accessed on 2022 Apr 26]. [Google Scholar]
- 8.Rueckl K, Springer B, Jungwirth-Weinberger A, Bechler U, Kasparek MF, Boettner F. A standardized soft tissue release technique to lower the risk of greater trochanteric fractures for the anterior approach in total hip arthroplasty. Arch Orthop Trauma Surg 2021;142:3067-73. [Google Scholar]
- 9.Chughtai M, Samuel LT, Acuña AJ, Kamath AF. Algorithmic soft tissue femoral release in anterior approach total hip arthroplasty. Arthroplast Today 2019;5:471-6. [Google Scholar]
- 10.Shadid MB, Vinken NS, Marting LN, Wolterbeek N. The Dutch version of the forgotten joint score: Test-retesting reliability and validation. Acta Orthop Belg 2016;82:112-8. [Google Scholar]
- 11.Singh V, Bieganowski T, Huang S, Karia R, Davidovitch RI, Schwarzkopf R. The forgotten joint score patient-acceptable symptom state following primary total hip arthroplasty. Bone Jt Open 2022;3:307-13. [Google Scholar]
- 12.Ghijselings SG, Driesen R, Simon JP, Corten K. Distal extension of the anterior approach to the hip using the femoral interbundle technique: Surgical technique and case series. J Arthroplasty 2017;32:2186-90. [Google Scholar]
- 13.Malkani AL, Garber AT, Ong KL, Dimar JR, Baykal D, Glassman SD, et al. Total hip arthroplasty in patients with previous lumbar fusion surgery: Are there more dislocations and revisions? J Arthroplasty 2018;33:1189-93. [Google Scholar]
- 14.Angerame M, Dennis D. Surgical approaches for total hip arthroplasty. Ann Joint 2018;3:43-3. [Google Scholar]
- 15.van Erp JH, Snijders TE, Weinans H, Castelein RM, Schlösser TP, de Gast A. The role of the femoral component orientation on dislocations in THA: A systematic review. Arch Orthop Trauma Surg 2021;142:1253-64. [Google Scholar]
- 16.Thajudeen MZ, Merican AM, Hashim MS, Nordin A. The utility of lesser trochanter version to estimate femoral anteversion in total hip arthroplasty: A three-dimensional computed tomography study. Surg Tech Dev 2022;11:54-61. [Google Scholar]
- 17.Yun H, Yoon J, Yang J, Song S, Park S, Lee J. A validation study for estimation of femoral anteversion using the posterior lesser trochanter line: An analysis of computed tomography measurement. J Arthroplast 2013;28:1776-80. [Google Scholar]
- 18.Emerson RH Jr. Increased anteversion of press-fit femoral stems compared with anatomic femur. Clin Orthop Relat Res 2012;470:477-81. [Google Scholar]
- 19.Jackson JB, Martin JR, Christal A, Masonis JL, Springer BD, Mason JB. The direct anterior approach total hip arthroplasty reliably achieves “Safe Zones” for combined anteversion. Arthroplast Today 2020;6:651-4. [Google Scholar]
- 20.Lawrence DD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res 2019;467:119-27. [Google Scholar]
- 21.Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone 1993;14:231-42. [Google Scholar]
- 22.Belzunce MA, Henckel J, Di Laura A, Hart A. Uncemented femoral stem orientation and position in total hip arthroplasty: A CT study. J Orthop Res 2020;38:1486-96. [Google Scholar]
- 23.Martin JR, Masonis JL, Mason JB. Anatomic total hip component position is more reproducible with the direct anterior approach using intraoperative fluoroscopy. Arthroplast Today 2020;6:777-83. [Google Scholar]
- 24.Boe RH, Selemon NA, Eachempati KK, Paprosky WG, Sheth NP. Soft-tissue balancing in total hip arthroplasty. JBJS Rev 2021;9:e20.00116. [Google Scholar]










