Bicondylar tibial plateau fractures and associated ACL rupture can be treated simultaneously with open reduction internal fixation and iliotibial band ACL reconstruction under a single anesthetic event.
Dr. Benjamin Wilson, Department of Orthopaedic Surgery and Sports Medicine, University of Kentucky, Lexington, Kentucky. E-mail: wilso.ben@uky.edu
Introduction: Tibial plateau fractures are frequently associated with associated soft-tissue injuries. Typical treatment algorithms prioritize bony stabilization followed by delayed soft-tissue reconstruction. However, when the soft-tissue injury needs urgent intervention to optimize patient outcome, early soft-tissue reconstruction may be indicated.
Case Report: This case report features a high-energy tibia plateau fracture-dislocation with associated anterior cruciate ligament (ACL) and bucket-handle lateral meniscus tear sustained after a fall. The treatment of both bony and soft-tissue injury took place during a single anesthetic event by utilizing a novel application of a previously described technique for ACL reconstruction with iliotibial band (ITB) autograft.
Conclusion: The ITB ACL reconstruction technique can be used in adults with concomitant ACL rupture and tibial plateau fracture. This allows patients to undergo a single anesthetic event for treatment of both bony and soft-tissue injuries.
Keywords: Tibial plateau, anterior cruciate ligament reconstruction, iliotibial band anterior cruciate ligament reconstruction, bucket-handle meniscal tear.
Tibial plateau fractures are often associated with soft-tissue injuries about the knee including meniscal tears, ligament ruptures, and chondral injuries [1]. Typical treatment algorithms prioritize fracture fixation followed by delayed soft-tissue reconstruction after the bony healing [2]. However, on occasion, the intra-articular soft-tissue injury necessitates acute intervention. In the case of a bucket-handle tear of the meniscus in association with an anterior cruciate ligament (ACL) tear, the surgeon is left with a conundrum. The displaced meniscus tear cannot be left until the second stage without risk of irreparable damage to the meniscal tissue, which would degrade the long-term outcome of the knee joint. However, reducing and repairing the meniscus, while leaving the ACL disrupted, runs the risk of repeated pivoting injuries, potentially injuring the meniscus further [3]. Ideally, the surgeon could perform meniscal repair in the same setting of ligament reconstruction; however, in a combined injury with tibial plateau fracture, screw traffic within the tibia prevents tunnel drilling which is needed for traditional ACL reconstruction. In this case report, we describe a novel method for combined tibial plateau fixation with concomitant meniscal repair and ACL reconstruction utilizing intra- and extra-articular reconstruction with the iliotibial band, without the need for bone tunnels.
A healthy active 25-year-old female presented to our level one trauma center after a fall from height while rock climbing, sustaining a bicondylar tibial plateau fracture-dislocation (Fig. 1). 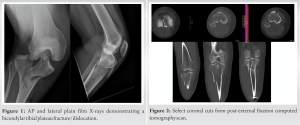
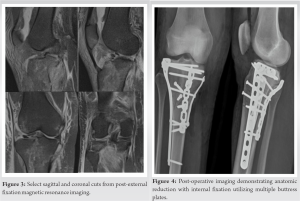

High-energy tibial plateau fractures are associated with concomitant intra-articular soft-tissue pathology. Gardner et al. prospectively reviewed 103 patients with acute, operatively treated tibial plateau fractures, and found a 77% incidence of collateral or cruciate ligament disruption, a 91% incidence of lateral meniscus injury, a 44% incidence of medial meniscus injury, and a 68% incidence of posterolateral corner injury [5]. Wang et al. reviewed 54 acute tibial plateau fractures with pre-operative MRI and found Schatzker IV and V fractures to have a higher likelihood of having a soft-tissue injury in association with their bony injury [6]. The patient in our case report sustained a bicondylar tibial plateau fracture that required multiple buttress plates for bony fixation, thus preventing the use of typical bone tunnels for ligament reconstruction. Given the limited uninvolved bone present in the proximal tibia after tibial plateau fixation, treating the ACL injury with standard reconstruction techniques was not possible. For this reason, an ITB autograft reconstruction was performed. ACL treatment in pediatric patients requires recognition of the distal femoral and proximal tibial physes and the potential implications that ACL reconstruction can have on the child’s growth. There are both “physeal sparing” and “physeal respecting” ACL reconstruction techniques that allow the orthopedic surgeon to reconstruct an ACL without compromising physeal function [7], one of which, the intra-articular extraphyseal reconstruction with ITB, avoids the use of bone tunnels entirely. This technique was first developed by Micheli et al. at Boston Children’s Hospital as a modification of a historical lateral extra-articular tenodesis, with application to the skeletally immature child [8,9]. The ITB ACLR technique has undergone multiple clinical and biomechanical reviews documenting its efficacy [10]. It is important to note that, in this case, we modified the original description of the procedure by Kocher et al. [10,11]. To our knowledge, this is the first description of its use in the adult trauma population. Also, we modified the way in which the graft was fixed to the tibia. For pediatric patients, the tibial side of the graft is sutured into the periosteum that is typically present in younger children. In the adult patient, the periosteum is not as robust, and in the case of high-energy trauma and significant soft-tissue injury, the surgeon cannot count on the strength of the periosteum alone. In this case, we utilized suture anchors placed in the anteromedial tibia to fix our ACL graft. The primary downside to performing acute ACL reconstruction is arthrofibrosis, a complication that occurs in 4–38% of ACL reconstructions [12]. Typically, ACL reconstruction is delayed until full range of motion is obtained. In the setting of a bucket-handle meniscal tear, soft-tissue surgery becomes more urgent to prevent long-term degenerative changes to the articular cartilage [12]. Acute repair of the patient’s meniscal pathology was indicated in this clinical setting, and performing an ACL reconstruction acutely helps provide additional stability to the knee to protect the meniscal repair. Korpershoek et al. performed a systematic review demonstrating level two evidence that ACL reconstruction at the same time as meniscal repair was protective compared to delayed ACL reconstruction [13]. In a retrospective cohort study, Wasserstein et al. reviewed meniscal repairs with and without ACL reconstruction. About 9.7% in the combined cohort underwent meniscal reoperation, while 16.7% in the meniscal repair alone group required reoperation [14]. Although she did develop arthrofibrosis requiring a return to the operating room, performing the ITB ACLR acutely protected her meniscal repair, which was found to be intact at the time of her second operation. The consequence of arthrofibrosis was treated successfully with lysis of adhesions, manipulation under anesthesia, and therapy.
To the best of our knowledge, this is the first case report of the ITB ACLR being used in an adult trauma patient. The ITB ACLR technique can be used in the setting of ACL rupture in association with high-energy tibial plateau fracture. This technique allows the orthopedic surgeon to reconstruct the ACL with limited proximal tibial bone stock available.
Acute ITB ACLR can be used at the same time as tibial plateau fracture fixation. This is particularly useful when the patient has an urgent soft-tissue problem, such as a bucket-handle meniscal tear.
References
- 1.Mthethwa J, Chikate A. A review of the management of tibial plateau fractures. Musculoskelet Surg 2018;102:119-27. [Google Scholar]
- 2.Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke SK. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am 2006;88:1713-21. [Google Scholar]
- 3.Rodriguez AN, LaPrade RF, Geeslin AG. Combined meniscus repair and anterior cruciate ligament reconstruction. Arthroscopy 2022;38:670-2. [Google Scholar]
- 4.Bryson WN, Fischer EJ, Jennings JW, Hillen TJ, Friedman MV, Baker JC. Three-column classification system for tibial plateau fractures: What the orthopedic surgeon wants to know. Radiographics 2021;41:144-55. [Google Scholar]
- 5.Gardner MJ, Yacoubian S, Geller D, Suk M, Mintz D, Potter H, et al. The incidence of soft tissue injury in operative tibial plateau fractures: A magnetic resonance imaging analysis of 103 patients. J Orthop Trauma 2005;19:79-84. [Google Scholar]
- 6.Wang J, Wei J, Wang M. The distinct prediction standards for radiological assessments associated with soft tissue injuries in the acute tibial plateau fracture. Eur J Orthop Surg Traumatol 2015;25:913-20. [Google Scholar]
- 7.Fabricant PD, Kocher MS. Management of ACL injuries in children and adolescents. J Bone Joint Surg Am 2017;99:600-12. [Google Scholar]
- 8.Micheli LJ, Rask B, Gerberg L. Anterior cruciate ligament reconstruction in patients who are prepubescent. Clin Orthop Relat Res 1999;364:40-7. [Google Scholar]
- 9.Willimon SC, Jones CR, Herzog MM, May KH, Leake MJ, Busch MT. Micheli anterior cruciate ligament reconstruction in skeletally immature youths: A retrospective case series with a mean 3-year follow-up. Am J Sports Med 2015;43:2974-81. [Google Scholar]
- 10.Kocher MS, Heyworth BE, Fabricant PD, Tepolt FA, Micheli LJ. Outcomes of physeal-sparing ACL reconstruction with iliotibial band autograft in skeletally immature prepubescent children. J Bone Joint Surg Am 2018;100:1087-94. [Google Scholar]
- 11.Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am 2005;87:2371-9. [Google Scholar]
- 12.Ekhtiari S, Horner NS, de Sa D, Simunovic N, Hirschmann MT, Ogilvie R, et al. Arthrofibrosis after ACL reconstruction is best treated in a step-wise approach with early recognition and intervention: A systematic review. Knee Surg Sports Traumatol Arthrosc 2017;25:3929-37. [Google Scholar]
- 13.Korpershoek JV, de Windt TS, Vonk LA, Krych AJ, Saris DB. Does anterior cruciate ligament reconstruction protect the meniscus and its repair? A systematic review. Orthop J Sports Med 2020;8(7):2325967120933895 . [Google Scholar]
- 14.Wasserstein D, Dwyer T, Gandhi R, Austin PC, Mahomed N, Ogilvie-Harris D. A matched-cohort population study of reoperation after meniscal repair with and without concomitant anterior cruciate ligament reconstruction. Am J Sports Med 2013;41:349-55. [Google Scholar]








