The management of an aneurysmal bone cyst complicated by a pathologic fracture in a growing adolescent can be done using hydroxyapatite granules as bone graft substitute to avoid damaging growing bone involved in autogenous bone grafting along with dynamic hip screw and plate for fracture stabilization, with a favorable outcome.
Dr. Aashay Sonkusale, Department of Orthopaedics, Indira Gandhi Government Medical College and Hospital, Nagpur, Maharashtra, India. E-mail: aashay49@gmail.com
Introduction: Aneurysmal bone cysts (ABCs) are a group of benign, expansile, locally aggressive lesion characterized by fluid-filled cysts usually in the metaphyseal end of long bones. They usually affect children and young adults, with an atypical etiology and uncommon presentation. Treatment modalities include en bloc resection and curettage with or without bone graft or bone substitute augmentation with instrumentation, sclerosing agents, arterial embolization, and adjuvant radiotherapy.
Case Report: We report a rare case of ABC with pathological fracture in the proximal femur of a 13-year-old male patient, who presented to the emergency department with severe pain in the right hip and inability to walk following trivial fall while playing. Curettage with open biopsy was performed followed by implantation with modified hydroxyapatite granules and internal fixation for the subtrochanteric fracture with pediatric dynamic hip screw and four hole plate, with a favorable outcome.
Conclusion: There is a lack of a standard guideline for the management on account of uniqueness of these cases; curettage with bone graft or bone substitutes in conjunction with internal fixation of associated pathologic fracture yields bony union with adequate clinical results.
Keywords: Aneurysmal bone cyst, pathological fracture, proximal femur.
Aneurysmal bone cysts (ABCs) are benign, osteolytic, locally destructive lesions with potential to metastasize and are characterized by expansile blood-filled, multiloculated cystic structures separated by fibrous septae. Most studies estimate the incidence of ABCs to be 0.14/100,000 people accounting for 1–6% of all primary bone tumors with 80% presenting within the first two decades of life and a median age of 13–15 years. It is most commonly located in the metaphyseal end of long bone with the highest incidence in the proximal end of femur [1]. The etiology and pathogenesis of this bony lesion are poorly understood, with some theories suggesting it to arise from vascular malformations, trauma, and genetics [2]. Primary ABCs have been shown to be true neoplasms linked with chromosomal fusion that may affect osteoblastic maturation [3]. Secondary ABC can also arise from other lesions such as chondroblastomas, osteosarcoma, osteoblastoma, non-ossifying fibroma, and giant cell tumors [4]. Histologically, it is classified as conventional/vascular type, solid type, and mixed type. Treatment modalities include curettage with or without bone grafting or bone substitutes, intralesional injections, arterial embolization, adjuvant radiotherapy, demineralized matrix application, and en bloc resection [5]. This is a case report of an ABC in the proximal metaphysis of femur complicated by a subtrochanteric pathologic fracture following trivial trauma, managed with curettage, bone substitute implantation, and internal fixation with pediatric dynamic hip screw (DHS).
This is a case of a 13-year-old boy who presented to the emergency department with pain in the right groin and inability to bear weight for 2 days following a trivial fall while playing a contact sport (Kabaddi). He gave a history of dull aching pain in the right groin for 2 months, exacerbated on movements but was able to ambulate till his fall. He had no other constitutional symptoms; his family and medical history were otherwise unremarkable. On physical examination, the right lower limb was externally rotated with diffuse swelling and tenderness on deep palpation over the right proximal thigh. Plain radiography on anteroposterior and lateral views revealed a subtrochanteric fracture with an elliptical eccentric lytic lesion with “soap bubble appearance” with septae and sclerotic margins in the proximal metaphyseal region of the right femur (Fig. 1 and 2). Pre-operative radiograph anteroposterior view of pelvis with bilateral hip (Fig. 1) and lateral view of affected right hip (Fig. 2) with open physis showing a subtrochanteric fracture and an elliptical eccentric lytic lesion with “soap bubble appearance” with septae and sclerotic margins in the proximal metaphyseal region. Under spinal anesthesia, the patient was taken in supine position under all aseptic precautions. A lateral approach to the tumor was taken. A biopsy was taken, after which a through curettage was done and hemostasis was achieved. The resultant cavity was filled with implantation of 5 units (one unit containing 10 cc of granules) of hydroxyapatite granules. The fracture was fixed with pediatric DHS and four hole DHS plate. Immediate post-operative radiograph showed stable fixation. Histopathological examination showed irregular dilated spaces lined by fibroblasts surrounding septae, also showing many osteoclasts, histiocytes, and fibroblasts surrounded by bony trabeculae. Follow-up after 5 years shows radiologic and clinical signs of fracture healing, consolidation, and complete incorporation of granules with no signs of recurrences (Figs. 3 and 4). The patient had good range of motion of hip with pain free ambulation with some residual discomfort in squatting (Fig. 5). Plain radiographs show anteroposterior view (Fig. 3) and lateral view (Fig. 4) of 5-year follow-up showing well-consolidated and healed fracture with complete incorporation of the granules.
ABC is locally aggressive and expansile lesions with potential to metastasize. These tumors consist of blood-filled septate cavities lined by fibroblast and histiocytes. More than 90% are seen within the first three decades. Pathologic fractures occur in 8% of ABCs [1]. Histologically, ABCs are classified as conventional/vascular type, solid type, and a mixed type. The current case report is consistent with a primary ABC of the conventional type. 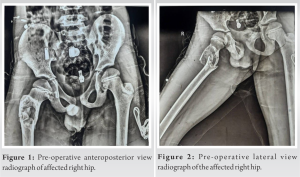
ABC is an uncommon bony lesion. However, whenever a bony lytic lesion is encountered in the first two decades of life, a differential of ABC should always be borne in mind. Curettage with management of the resultant dead space in conjunction with fixation of the associated pathologic fracture is mainstay of treatment. Further studies are warranted for a better understanding of the pathogenesis and a standard guideline for management.
This case report strives to add to the current knowledge on ABC and this management protocols, considering the rarity of this lesion and paucity of literature.
References
- 1.Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R. Aneurysmal bone cyst. A population based epidemiologic study and literature review. Clin Orthop Relat Res 1999;363:176-9. [Google Scholar]
- 2.Cottalorda J, Bourelle S. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg 2007;127:105-14. [Google Scholar]
- 3.Lau AW, Pringle LM, Quick L, Riquelme DN, Ye Y, Oliveira AM, et al. TRE17/ubiquitin-specific protease 6 (USP6) oncogene translocated in aneurysmal bone cyst blocks osteoblastic maturation via an autocrine mechanism involving bone morphogenetic protein dysregulation. J Biol Chem 2010;285:37111-20. [Google Scholar]
- 4.Rapp TB, Ward JP, Alaia MJ. Aneurysmal bone cyst. J Am Acad Orthop Surg 2012;11:233-41. [Google Scholar]
- 5.Bonakdarpour A, Levy WM, Aegerter E. Primary and secondary aneurysmal bone cyst: A radiological study of 75 cases. Radiology 1978;126:75-83. [Google Scholar]
- 6.Sajjanshetty R, Timothy J. Proximal femur pathological fracture secondary to aneurysmal bone cyst in a child. Int J Orthop Sci 2019;5:55-7. [Google Scholar]
- 7.Cole WG. Treatment of aneurysmal bone cysts in childhood. J Pediatr Orthop 1986;6:326-9. [Google Scholar]
- 8.Varshney MK, Rastogi S, Khan SA, Trikha V. Is sclerotherapy better than intralesional excision for treating aneurysmal bone cysts? Clin Orthop Relat Res 2010;468:1649-59. [Google Scholar]
- 9.Güven M, Demirel M, Ozler T, Başsorgun IC, Ipek S, Kara S. An aggressive aneurysmal bone cyst of the proximal humerus and related complications in a pediatric patient. Strategies Trauma Limb Reconstr 2012;7:51-6. [Google Scholar]
- 10.Willeumier JJ, van der Linden YM, van de Sande MA, Dijkstra PD. Treatment of pathological fractures of the long bones. EFORT Open Rev 2016;1:136-45. [Google Scholar]
- 11.Wai EK, Davis AM, Griffin A, Bell RS, Wunder JS. Pathologic fractures of the proximal femur secondary to benign bone tumors. Clin Orthop Relat Res 2001;393:279-86. [Google Scholar]










