Stacked plating can successfully be used as an alternative to treat peri-implant proximal humerus fractures.
Dr. Daniel T DeGenova, Department of Orthopedics, OhioHealth/Doctors Hospital, Columbus, Ohio, United States. E-mail: ddegenova22@gmail.com
Introduction: A peri-implant proximal humerus fracture is a rare complication after open reduction and internal fixation (ORIF) and poses a surgical dilemma.
Case Report: A 56-year-old male sustained a peri-implant proximal humerus fracture after undergoing ORIF. We present a stacked plating method for fixation of this injury. This construct allows for decreased operative time, less soft-tissue dissection, and the ability to leave previous intact hardware in place.
Conclusion: We describe the rare case of a peri-implant proximal humerus treated with stacked plating.
Keywords: Peri-implant proximal humerus fracture, ORIF proximal humerus, stacked plating, proximal humerus fixation.
Proximal humerus fractures account for approximately 6% of all fractures and are the third most common fractures in adults [1]. The incidence of proximal humerus fractures is approximately 82/100,000 person and increases with age [2]. Most proximal humerus fractures occur in older populations after low-energy trauma, with the most common mechanism being a fall from standing height producing minimally displaced osteoporotic fractures [2]. However, these injuries also occur after high energy mechanisms producing more complex fracture patterns [3]. The optimal treatment of proximal humerus fractures remains controversial. Many are treated with non-operative management and have good functional and radiographic outcomes with few complications [4]. Indications for operative treatment vary in the literature. Open reduction and internal fixation (ORIF) is often indicated for the treatment of 2-part, 3-part, and some 4-part fractures in younger, active patients [5, 6]. One rare complication of ORIF of proximal humerus fractures is a peri-implant fracture just distal to the implant. Most hardware-related proximal humerus fractures reported in the literature are periprosthetic fractures related to hemiarthroplasty, anatomic, or reverse shoulder arthroplasty [7]. We are currently unaware of any previous reports of peri-implant proximal humerus fractures. In addition, the use of stacked plating for fracture fixation is also limited [8, 9]. Stacked plating is the concept of placing one plate on top of another to link constructs. This allows for the lengthening of a construct and increased additional fixation. We describe a case of a peri-implant proximal humerus fracture treated with stacked plating.
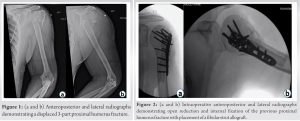
A 56-year-old male with a past medical history of alcohol substance abuse with seizures, hypertension, and tobacco abuse presented to our urban Level I trauma center after falling from a ladder. He presented with left shoulder, elbow, and chest pain. Radiographs demonstrated displaced 3-part proximal humerus fracture (Fig. 1a and b). In addition, the patient was found to have a non-displaced ipsilateral radial neck fracture and ipsilateral non-displaced 4th–9th rib fractures.
Surgical procedure 1
Operative management of the injury occurred the following day. An anterolateral deltoid splitting approach was used, and the fracture was identified and reduced. A fibular strut allograft (LifeNet Health, Virginia Beach, VA.) was inserted into the humeral canal to augment the fixation. Fracture fixation was performed with a DePuy Synthes (West Chester, PA) 3.5 mm locking compression plate (LCP) proximal humerus plate (Fig. 2a and b). The greater and lesser tuberosities and associated rotator cuff muscles were sutured down to the plate using large non-absorbable suture. Total operative time was 75 min, and the estimated blood loss was minimal. The patient was then transferred to the post anesthesia care unit (PACU). There were no perioperative complications.
Post-operative course 1
The patient was immobilized with a sling and instructed to be non-weight bearing. The patient was able to be range of motion as tolerated to his left upper extremity. The additional injuries were treated nonoperatively. The patient was discharged on post-operative day 5. On post-operative day 11, the patient presented again to our trauma center after a fall down multiple stairs while intoxicated. The patient presented with the left shoulder pain, back pain, and left chest wall pain. The previous surgical incision showed routine healing. Radiographs demonstrated a displaced peri-implant proximal humerus fracture just distal to his original fracture fixation (Fig. 3a and b). In addition, the patient was found to have multiple vertebral superior endplate fractures.
Surgical procedure 2
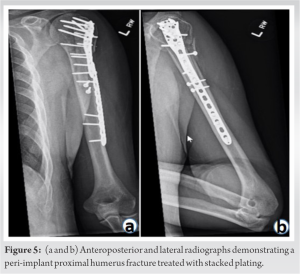
Operative management of the injury occurred the following day. The same anterolateral deltoid splitting approach was used and extended into the anterolateral approach to the humerus. The peri-implant humeral shaft fracture was first reduced and provisionally held together with two separate lag screws. Then, the distal two screws from the proximal humerus plate were removed. A DePuy synthes (West Chester, PA) 10 hole 3.5 mm LCP metaphyseal plate with a thin proximal flare was placed so that the two most proximal screws were overlapped to link the two constructs (Fig. 4a-c). The greater tuberosity fragment had displaced from the fall and was fixed with an independent lag screw and an additional heavy gauge non-absorbable suture. Two proximal screws that were loosened from the fall were also replaced (Fig. 5a and b). Total operative time was 72 min, and the estimated blood loss was minimal. The patient was then transferred to the PACU. There were no perioperative complications.
Post-operative course 2
The patient was immobilized with a sling and instructed to be non-weight-bearing. The patient was able to be range of motion as tolerated to his left upper extremity. The additional injuries were treated nonoperatively. The patient was discharged on post-operative day 1. The patient followed up at 2 weeks postoperatively with a well healing incision and no complications. The patient had full passive range of motion, decreased active range of motion secondary to pain, and was otherwise neurovascularly intact. The patient was then lost to follow-up until 13 months postoperatively when he presented for repeat clinical evaluation. Clinically, the patient had no complications with full strength and range of motion. The patient reported very minimal pain and was not using pain medication. Radiographs at this final visit demonstrated stacked plate fixation with appropriate positioning, evidence of bony union, and no signs of displacement or hardware loosening. The patient was able to return to his previous level of activity.
We present a rare case of a patient who presented with a displaced peri-implant proximal humerus fracture and underwent ORIF using a stacked plate technique. At 13 months of follow-up, fracture union was achieved, and the patient was able to return to his previous level of activity. The majority of the implant related fractures of the proximal humerus are periprosthetic fractures near shoulder hemiarthroplasty, anatomic total shoulder, or reverse shoulder arthroplasty stems [10, 11]. The prevalence of these fractures has been reported to be 0.6% in patients treated with anatomic shoulder arthroplasty [10]. Treatment options for these injuries range from non-operative management to total proximal humeral arthroplasty. The majority are often treated with ORIF using plate and screw constructs, along with the addition of cerclage wires [11]. Andersen et al. reported on 17 periprosthetic proximal humerus fractures in which all fractures achieved union at an average of 6.2 months; however, only 29.4% of these patients returned to their pre-fracture American shoulder and elbow surgeons score [12]. Conversely, the patient in the current report had equal range of motion and strength to the contralateral shoulder and was able to return to his previous level of activity. Stacked plating does not appear to be a new concept; however, there does appear to be a paucity of its use in the orthopedic literature [8, 9, 13]. Christodoulou et al. described stacked plating to treat distal one-third tibial shaft fractures that extended into the tibial plafond [13]. Radiographic union was achieved in all patients at 4.3 months without complications. This technique was described and performed before modern pre-contoured and locked plating technology was readily available. Stacked plating has been described for the use in the forearm on two occasions [8, 9]. In an open pediatric both bone forearm fracture, stacked plating was used to stabilize a segmental radial shaft fracture. The patient underwent irrigation and debridement with initial Kirschner wires (k-wire) placement to stabilize the distal radial metaphyseal fracture and a reconstruction plate was placed to reduce the diaphyseal portion. During the second operation, the k-wires were removed, and a titanium T-plate was placed to stabilize the distal radius, which overlapped the reconstruction plate. This allowed for the previous placed plate to remain in place resulting in shorter operative time and likely a cost reduction with using a shorter implant. The use of stacked plating can lead to less soft-tissue dissection when placing the second plate and avoid the increased risk of infection and non-union [8, 9, 13]. Mudgal and Ring described stacked plating for meta-diaphyseal fractures of the distal radius [9]. The authors discuss the benefits of stacked plating as extending shorter constructs and creating a stiffer construct. In the current case, stacked plating was used to extend the construct and allow for less soft-tissue dissection with the benefit of leaving the previous hardware in place. Potential risks of stacked plating have been described [8, 9]. Hoellwarth and Scannell discuss the potential risk of corrosion-related problems of stacking plates of different material [8]. In their series, titanium and stainless-steel plates were stacked in direct contact; however, they report that with modern orthopedic plating technology, it is unlikely to cause corrosion-related problems [8]. Furthermore, stacked plating leads to increased volume of the construct and potentially leads to difficulties with wound closure. While this has not been reported to lead to adverse outcomes, it should be taken into consideration if thick plates are used [9].
Peri-implant proximal humerus fractures are rare injuries. The described stacked plating technique can lead to a shorter operative time with less soft-tissue dissection and the ability to leave previous hardware in place. Stacked plating can be used to address uncommon and complex peri-implant proximal humerus fractures.
Stacked plating can successfully be used as an alternative to treat peri-implant proximal humerus fractures.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Google Scholar]
- 2.Van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone 2001;29:517-22. [Google Scholar]
- 3.Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, et al. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res 2012;98:715-9. [Google Scholar]
- 4.Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin BC, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: The PROFHER randomized clinical trial. JAMA 2015;313:1037-47. [Google Scholar]
- 5.DeFranco MJ, Brems JJ, Williams GR Jr., Iannotti JP. Evaluation and management of valgus impacted four-part proximal humerus fractures. Clin Orthop Relat Res 2006;442:109-14. [Google Scholar]
- 6.Myers DM, Triplet JJ, Warmoth PJ, Passias BJ, McGowan SP, Taylor BC. Improved outcomes using a fibular strut in proximal humerus fracture fixation. Orthopedics 2020;43:262-8. [Google Scholar]
- 7.Kurowicki J, Momoh E, Levy JC. Treatment of periprosthetic humerus fractures with open reduction and internal fixation. J Orthop Trauma 2016;30:e369-74. [Google Scholar]
- 8.Hoellwarth JS, Scannell BP. Pediatric open both-bone forearm fracture stabilized with titanium and stainless steel stacked extension internal plating: A case report. JBJS Case Connect 2020;10:e20.00325. [Google Scholar]
- 9.Mudgal CS, Ring D. Stacked plating for metadiaphyseal fractures of the distal radius: A technique report. J Orthop Trauma 2007;21:63-6. [Google Scholar]
- 10.Wright TW, Cofield RH. Humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am 1995;77:1340-6. [Google Scholar]
- 11.Steinmann SP, Cheung EV. Treatment of periprosthetic humerus fractures associated with shoulder arthroplasty. J Am Acad Orthop Surg 2008;16:199-207. [Google Scholar]
- 12.Andersen JR, Williams CD, Cain R, Mighell M, Frankle M. Surgically treated humeral shaft fractures following shoulder arthroplasty. J Bone Joint Surg Am 2013;95:9-18. [Google Scholar]
- 13.Christodoulou A, Ploumis A, Terzidis I, Givissis P, Hatzokos I, Pournaras J. Fixation of distal tibial fractures with intraarticular extension using double overlapping plates. Orthopedics 2004;27:1155-8. [Google Scholar]