Although lipoma arborescens rarely occurs in the shoulder joints, it causes severe pain and it should be one of the differential diagnoses.
Dr. Masanori Nakayama, Department of Orthopaedic Surgery, School of Medicine, International University of Health and Welfare, 852, Hatakeda, Narita, Chiba, 286-8520, Japan. E-mail: masanorinkym@yahoo.co.jp
Introduction:Lipoma arborescens is a tumor-like lesion that occurs inside joints and synovial bursae, especially in knee joints. It rarely occurs in the shoulder joints and this disease usually causes severe shoulder pain. This study aims to report a rare case of lipoma arborescens occurring in the subdeltoid bursa with severe shoulder pain.
Case Report: A 59-year-old woman with severe pain and restriction of range of motion (ROM) for her right shoulder consisting for 2 months was referred to our hospital. Magnetic resonance imaging (MRI) findings revealed that a tumor-like lesion exists in the subdeltoid bursa in her right shoulder and blood examinations revealed no abnormal findings. Surgical resection of the tumor-like lesion was performed and the rotator cuff was repaired because this tumor-like lesion invaded the rotator cuff partially. Pathology examination of the resected tissues was consistent with lipoma arborescens. One year after surgery, the patient’s shoulder pain was diminished and its ROM recovered. There was no significant difficulty in activities of daily living.
Conclusion: Lipoma arborescens should be considered when patients present with complaints of severe shoulder pain. Even if their physical findings do not suggest rotator cuff injuries, MRI should be performed to rule out lipoma arborescens.
Keywords: Lipoma arborescens, shoulder, subdeltoid bursa.
Lipoma arborescens is a relatively rare disease occurring in joints and bursae that was first reported in 1904 [1]. In recent years, however, it has been found that this disease is not a true neoplastic disease but is likely to be a reactive change in synovial and adipose tissue followed by chronic inflammation and physical irritation [1]. Moreover, since dendritic or papillary synovial hyperplasia did not occur in some cases, it is also called “synovial lipomatosis” [1, 2]. The most common area affected by this disease is the knee joints [1], but it rarely occurs in shoulder joints. To the best of our knowledge, there have been only several reports of lipoma arborescens occurring in the subdeltoid bursa of shoulder joints [2, 3, 4, 5, 6, 7, 8, 9, 10]. This is a case report of a middle-aged female patient with lipoma arborescens which occurred in the right subdeltoid bursa and caused severe shoulder pain and limited motion of the shoulder joint, and surgical resection relieved her pain and the shoulder range of motion (ROM) was recovered.
A 59-year-old woman who was working as a desk worker, with a 2-month history of severe pain in the right shoulder. She consulted her primary clinic and she received the diagnosis of shoulder periarthritis and she was administered oral painkillers for 4 months and an intraarticular injection of corticosteroid was also administered for a month for 4 months. However, the shoulder pain was not relieved and she was referred to our hospital for further assessment of her severe shoulder pain. At our first medical examination, the patient had marked pain in her right shoulder joint, and the active ROM of the joint was extremely restricted; its flexion and abduction were 80° and 70°, respectively. The blood test was normal, including matrix metalloproteinase 3, anti-cyclic citrullinated peptides antibody, and rheumatoid factor. X-rays showed no remarkable findings except mild degeneration of the humeral head. Ultrasonography imaging using the color doppler method showed a mass like a cyst with blood flow in the subdeltoid bursa. Needle aspiration to the mass was attempted but no fluid was aspirated. Magnetic resonance imaging (MRI) revealed a tumor-like mass enclosing lobulated structures invaginating into the subdeltoid bursa with a high signal intensity on both T1-weighted and T2-weighted images, and with suppression on the fat suppression images (Fig. 1).
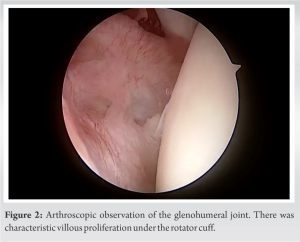

Lipoma arborescens mostly occurs in knee joints and it rarely occurs in shoulder joints. Although knee joint cases involved little or no pain, most of the shoulder cases were reported with severe pain [4, 5, 6, 7, 8, 9, 10], similar to ours. There are reported to be several causes for the pain. One was the rotator cuff injury or tear in most cases [3, 6, 8, 9]. A second possibility is that there is also bursitis, synovitis, or swelling of the joint capsule [1, 7]. In our case, the patient felt severe shoulder pain, and the pain was not diminished by the conservative treatment for 4 months. The shoulder pain with the lipoma arborescens might be severer than that of a shoulder periarthritis, which was one of the important findings to suspect this disease. There are several diseases as differential diagnoses for this disease, such as pigmented villonodular synovitis (PVNS), synovial chondroma, and RA [11]. MRI was reported to be useful for the differentiation of these diseases, especially in PVNS and synovial chondroma [11]. In the typical MRI findings of lipoma arborescens, joint fluid was found with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, and synovial and villous lobular structures with equal signal intensity to subcutaneous fat on T1-weighted, T2-weighted, and fat-suppression images [1, 12]. PVNS has low signal intensity on both T1-weighted and T2-weighted images and usually has a gadolinium contrast effect [13]. Regarding synovial chondroma, there are frequently loose bodies in the X-ray findings, whereas lipoma arborescens usually does not include hard tissues [6]. It is difficult to differentiate lipoma arborescens from RA because its MRI findings are similar to those of lipoma arborescens [12]. In MRI findings of typical RA joints, there is/are sometimes a tumor-like lesion(s), a so-called rheumatoid nodule, which has mixed structure with similar signal intensity to joint fluid and equal to subcutaneous fat, like the MRI findings of lipoma arborescens. One of the specific MRI findings for RA is scattered lesions with only mildly low-signal intensity areas on both T1-weighted and T2-weighted images, indicative of fibrous pannus [12]. Therefore, it is difficult to determine a differential diagnosis between RA and lipoma arborescens only with image findings, and a blood test is necessary. Interestingly, some previous reports showed that serological findings about RA became positive later during the postoperative observations despite the first negative serological findings [1, 14]. Although all pre-operative serological findings regarding RA were negative in this case, careful observation for whether or not RA develops thereafter might be necessary. Since lipoma arborescens is sometimes difficult to differentiate from other diseases, it is important to make intra-articular observations during the surgery. Arthroscopic observation for the glenohumeral joint is less invasive than an open procedure, and observation of characteristic villous proliferation of the synovium would help differentiate lipoma arborescens from RA [5, 6, 8, 10]. In our case, characteristic villous proliferation was observed but it was not consistent with a typical RA inflammatory synovitis. This finding supported our differential diagnosis. While, arthroscopy for the subacromial joints in this disease might not be preferable because the arthroscope or other devices could penetrate the tumor-like lesion during the procedure, and we have avoided inserting the arthroscope into subacromial space in this case.
Lipoma arborescens should be considered when patients present with complaints of severe shoulder pain that is highly resistant to conservative treatment. Even if their physical findings do not suggest rotator cuff injuries, MRI should be performed to rule out lipoma arborescens. In this case, MRI findings supported the diagnosis, and the surgical excision of the tumor-like lesion and the rotator cuff repair were performed, relieving the patient’s severe shoulder pain and recovering its ROM.
Lipoma arborescens should be considered when patients present with complaints of severe shoulder pain, and MRI should be performed to rule out lipoma arborescens even if their physical findings do not suggest rotator cuff injuries.
References
- 1.Hallel T, Lew S, Bansal M. Villous lipomatous proliferation of the synovial membrane (lipoma arborescens). J Bone Joint Surg Am 1988;70:264-70. [Google Scholar]
- 2.Teusink M, El-Khoury G, Buckwalter J. Lipoma arborescens of the subdeltoid bursa: A case report. Iowa Orthop J 2010;30:177-8. [Google Scholar]
- 3.Dawson JS, Dowling F, Preston BJ, Neumann L. Case report: Lipoma arborescens of the sub-deltoid bursa. Br J Radiol 1995;68:197-9. [Google Scholar]
- 4.Nisolle JF, Blouard E, Baudrez V, Boutsen Y, De Cloedt P, Esselinckx W. Subacromial-subdeltoid lipoma arborescens associated with a rotator cuff tear. Skeletal Radiol 1999;28:283-5. [Google Scholar]
- 5.Pandey T, Alkhulaifi Y. Bilateral lipoma arborescens of the subdeltoid bursa. Australas Radiol 2006;50:487-9. [Google Scholar]
- 6.Kim MH, Chung SW, Yoon JP, Kim SH Oh JH. Subdeltoid lipoma arborescens combined with rotator cuff tears. Orthopedics 2013;36:e1103-7. [Google Scholar]
- 7.Kim RS, Kim YT, Choi JM, Shin SH, Kim YJ, Kim L. Lipoma arborescens associated with osseous/chondroid differentiation in subdeltoid bursa. Int J Shoulder Surg 2013;7:116-9. [Google Scholar]
- 8.Benegas E, Neto AA, Teodoro DS, da Silva MV, de Oliveira AM, Filippi RZ, et al. Lipoma arborescens: Rare case of rotator cuff tear associated with the presence of lipoma arborescens in the subacromial-subdeltoid and glenohumeral bursa. Rev Bras Ortop 2015;47:517-20. [Google Scholar]
- 9.Lim MC, See PL, Wang SY, Wee AT, Tee UL. Unusual case of lipoma arborescens in the subacromial-subdeltoid bursa. Med J Malaysia 2018;73:400-2. [Google Scholar]
- 10.Elamin M, Yeluri V, Khatir H, O’Grady P, Bennani F. Subacromial impingement by a lipoma arborescens. SICOT J 2021;7:12. [Google Scholar]
- 11.Sheldon PJ, Forrester DM, Learch TJ. Imaging of intraarticular masses. Radiographics 2005;25:105-19. [Google Scholar]
- 12.Vilanova JC, Barceló J, Villalón M, Aldomà J, Delgado E, Zapater I. MR imaging of lipoma arborescens and the associated lesions. Skeletal Radiol 2003;32:504-9. [Google Scholar]
- 13.Sailhan F, Hautefort P, Coulomb A, Mary P, Damsin JP. Bilateral lipoma arborescens of the knee: A case report. J Bone Joint Surg Am 2011;93:195-8. [Google Scholar]
- 14.Jonathan P, Bruce D, Bernrd C, Daughters TC. Lipoma arborescens of the knees in a patient with rheumatoid arthritis. Radiographics 2011;31:333-7. [Google Scholar]