Long-term use of ART drugs can lead to pathological fractures in these patients so optimal correction of metabolic abnormalities and multidisciplinary approach is necessary in treatment of such patients.
Dr. Ketan Mahesh Naik, Department of Orthopaedics, TNMC and BYL NAIR Charitable Hospital, Mumbai, Maharashtra, India. E-mail: ketanortho23593@gmail.com
Introduction: It has been noticed that human immunodeficiency virus (HIV) infection and anti-retro viral (ART) therapy, both individually lead to bone metabolic disorders, and hence, such patients have an increased propensity for fractures following trivial trauma.
Case Report: We present two cases, first a 52-year-old female with the right hip pain and inability to walk since 1 week following trivial trauma and associated dull pain in the left hip since 2 months ago. Radiographs revealed a right intertrochanteric fracture and a left unicortical fracture at level of lesser-trochanter. The patient was managed with closed proximal femoral nailing bilaterally and subsequently mobilized. Second, a 70-year-old female with bilateral leg pain and swelling following trivial trauma since 3 days . Radiographs revealed a distal one-third shaft tibia and fibula fracture bilaterally managed with closed nailing bilaterally and subsequently mobilized. Both patients had HIV infection since 10 and 14 years, respectively, and were on combination ART.
Conclusion: There should be a high index of suspicion to the possibility of fragility fractures in HIV affected patients on ART. Principles of fracture fixation and early mobilization should be followed.
Keywords: Human immunodeficiency virus, fragility fractures, anti-retroviral therapy, bilateral fractures.
There are approximately 37.7 million people living with human immunodeficiency virus (HIV) acquired-immune deficiency syndrome (AIDS) in the world of which 28.2 million people receive antiretroviral therapy (ART) [1]. ART has been noted to reduce viral load, improve immunological status, and increase the life expectancy significantly, but it also leads to long term adverse effects such as dyslipidemia, diabetes mellitus, and skeletal fragility [2, 3]. It has been noted that both HIV infection and ART individually lead to bone metabolic disorders and delay fracture healing; hence, these patients have an increased propensity for fractures following trivial injury and subsequent delayed healing [4, 5]. We present two cases having HIV-AIDS on ART who developed bilateral lower limb fragility fractures following trivial trauma and were managed surgically to highlight the possibility of association between patients with HIV on ART and such fractures. In addition, literature regarding similar cases and their management was reviewed.
Case 1
A 52-year-old female presented to us with pain in the right hip and inability to bear weight since 1 week ago following an episode of trivial fall, the patient also gave a history of dull aching pain in the left hip since the past 2 months. Bilateral hip examination revealed tenderness in both the proximal thigh, with flexion and external rotation deformity of the right lower limb. On subsequent X-rays, it was found that the patient had a right sided intertrochanteric fracture and a left-sided undisplaced unicortical fracture at the level of the lesser trochanter. The patient was a diagnosed case of HIV on ART comprising dolutegravir, lamivudine, and tenofovir since past 10 years. The patient was operated with closed reduction and internal fixation with a proximal femoral nail bilaterally. Post-operative period was uneventful and the patient was wheelchair mobilized initially and discharged after 5 days. The patient gradually progressed later to walking with the aid of a walker. A subsequent follow-up at 3 months revealed a uniting fracture bilaterally.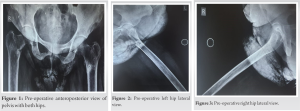
Case 2
A 70-year-old female presented with pain and swelling in both legs since 3 days following trivial trauma, with tenderness in both the legs. The X-rays revealed a fracture of the distal one-third shaft of tibia, bilaterally, with fracture of the bilateral fibula shaft at the same level. The patient was a diagnosed case of HIV on ART comprising dolutegravir, lamivudine, and tenofovir since past 14 years. The patient was managed surgically with closed reduction internal fixation with Intra-medullary interlocking nailing. Post-operative period was uneventful and the patient was wheelchair mobilized initially and discharged after 5 days. The patient gradually progressed later to walking with the aid of a walker. A subsequent follow-up at 3 months revealed a uniting fracture bilaterally. Appropriate calcium, vitamin D supplementation, and bisphosphonates were given to both the patients in the pre- and post-operative period to correct metabolic derangements and to aid fracture union.
HIV infection and ART have both been shown to reduce bone mineral density (BMD), mineralization, and bone turnover. A reduced BMD is thought to be associated with a reduced rate of fracture healing; hence, HIV-positive individuals are not only at an increased risk of fragility fractures but also of delayed fracture healing and failure of fracture fixation [6, 7, 8, 9, 10]. 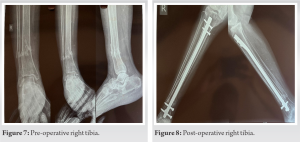 The prevalence of osteopenia in HIV infected individuals is 15%, that is, 3 times compared to uninfected controls; hence, they have an increased risk of fractures, the osteopenia is thought to be due to chronic inflammation directly leading to increased bony resorption and due to direct action on the osteoclastic activity [4, 11, 12]. There is a disturbance in the synchronized bone remodeling process as suggested by the raised osteocalcin, c-telopeptide, and TNF-alpha levels, which have shown to affect osteoclast function, in HIV-affected individuals. HIV is also known to be associated with osteonecrosis secondary to disruption of osseous blood supply which can in turn lead to delays in bone healing and may also result in non-unions [13, 14, 15]. HIV-infected postmenopausal women have lower BMD, increased bone turnover, and higher rates of bone loss than non-HIV infected women.
The prevalence of osteopenia in HIV infected individuals is 15%, that is, 3 times compared to uninfected controls; hence, they have an increased risk of fractures, the osteopenia is thought to be due to chronic inflammation directly leading to increased bony resorption and due to direct action on the osteoclastic activity [4, 11, 12]. There is a disturbance in the synchronized bone remodeling process as suggested by the raised osteocalcin, c-telopeptide, and TNF-alpha levels, which have shown to affect osteoclast function, in HIV-affected individuals. HIV is also known to be associated with osteonecrosis secondary to disruption of osseous blood supply which can in turn lead to delays in bone healing and may also result in non-unions [13, 14, 15]. HIV-infected postmenopausal women have lower BMD, increased bone turnover, and higher rates of bone loss than non-HIV infected women. 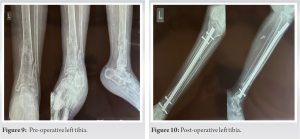 This is because estrogen mitigates the proresorptive effects of inflammatory cytokines, which are up-regulated in HIV infection; hence, bone loss may be accelerated in HIV-infected postmenopausal women during the menopausal transition stage placing these women at increased risk for fracture [16]. Brown and Qaqish also noted that the prevalence of osteopenia was significantly higher in those individuals taking ART, BMD was found to decrease after initiation of ART and stabilize later on [17]. There is 6% decrease in the BMD in the first 2 years post initiation of ART, irrespective of the drugs used. The mechanism is thought to be multifactorial, but, in part, is due to a direct effect on the osteoblasts and osteoclasts and increased catabolism of vitamin D along with mitochondrial damage [18]. Tenofovir, a nucleoside reverse-transcriptase inhibitors (NRTIs), is known to cause proximal renal tubulopathy with hypophosphatemia, hypokalemia, and metabolic acidosis affecting bone mineralization, leading to osteomalacia with multiple bone pains, weakness and fractures. The condition is managed by cessation of use of tenofovir and by electrolyte correction. In those presenting with renal fanconi syndrome, tenofovir may be substituted with other ART drugs [19]. Zidovudine an NRTI is also known to cause increased osteoclastic activity and hence bone loss. NRTI and protease inhibitors cause decrease BMD, with protease inhibitors having risk of vitamin D deficiency as well. Doltegravir containing regimens are thought to be excellent options to reduce the impact of ART on bone, especially in patients with low BMD, to reduce bone loss and fracture risk [20]. Overall, it is necessary to be to be aware of the association between fragility fractures and ART, to allow for the early diagnosis and management of such patients.
This is because estrogen mitigates the proresorptive effects of inflammatory cytokines, which are up-regulated in HIV infection; hence, bone loss may be accelerated in HIV-infected postmenopausal women during the menopausal transition stage placing these women at increased risk for fracture [16]. Brown and Qaqish also noted that the prevalence of osteopenia was significantly higher in those individuals taking ART, BMD was found to decrease after initiation of ART and stabilize later on [17]. There is 6% decrease in the BMD in the first 2 years post initiation of ART, irrespective of the drugs used. The mechanism is thought to be multifactorial, but, in part, is due to a direct effect on the osteoblasts and osteoclasts and increased catabolism of vitamin D along with mitochondrial damage [18]. Tenofovir, a nucleoside reverse-transcriptase inhibitors (NRTIs), is known to cause proximal renal tubulopathy with hypophosphatemia, hypokalemia, and metabolic acidosis affecting bone mineralization, leading to osteomalacia with multiple bone pains, weakness and fractures. The condition is managed by cessation of use of tenofovir and by electrolyte correction. In those presenting with renal fanconi syndrome, tenofovir may be substituted with other ART drugs [19]. Zidovudine an NRTI is also known to cause increased osteoclastic activity and hence bone loss. NRTI and protease inhibitors cause decrease BMD, with protease inhibitors having risk of vitamin D deficiency as well. Doltegravir containing regimens are thought to be excellent options to reduce the impact of ART on bone, especially in patients with low BMD, to reduce bone loss and fracture risk [20]. Overall, it is necessary to be to be aware of the association between fragility fractures and ART, to allow for the early diagnosis and management of such patients.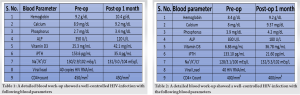
There should be a strong index of suspicion to the possibility of fragility fractures in patients with HIV on ART, having complaints of bony pains. Surgical principles of fracture fixation remain similar as in other patients; however, a thorough metabolic work-up should be undertaken and other contributory factors should be investigated and treated accordingly. To reduce the chances of osteoporosis and associated fragility fractures in patients of HIV on ART, daily vitamin D supplementation has been recommended, and other measures such as calcium supplementation, bisphosphonates, and weight-bearing exercises have also been recommended. A collaborative approach between orthopedic surgeons and other specialties is required to bring about optimal results in such patients.
A high index of suspicion should be there to the possibility of fragility fractures in patients of HIV on ART. They should be managed following principles of fracture management, along with correction of the metabolic abnormalities.
References
- 1.Global HIV and AIDS Statistics-fact Sheet (UNAIDS 2021). Available from: https://www.unaids.org/en/resources/fact-sheet Last accessed on 2012. [Google Scholar]
- 2.Lederman MM, Valdez H. Immune restoration with antiretroviral therapies: Implications for clinical management. JAMA 2000;284:223-8. [Google Scholar]
- 3.Behrens G, Dejam A, Schmidt H, Balks HJ, Brabant G, Körner T, et al. Impaired glucose tolerance, beta cell function and lipid metabolism in HIV patients under treatment with protease inhibitors. AIDS 1999;13:F63-70. [Google Scholar]
- 4.Prior J, Burdge D, Maan E, Milner R, Hankins C, Klein M, et al. Fragility fractures and bone mineral density in HIV positive women: A case-control population-based study. Osteoporos Int 2007;18:1345-53. [Google Scholar]
- 5.Tebas P, Powderly WG, Claxton S, Marin D, Tantisiriwat W, Teitelbaum SL, et al. Accelerated bone mineral loss in HIV-infected patients receiving potent antiretroviral therapy. AIDS 2000;14:F63-7. [Google Scholar]
- 6.Singh K, Moyle GJ. Bone mineral abnormalities in persons with HIV infection: Signal or noise? AIDS Read 2006;16:407-10, 413-8. [Google Scholar]
- 7.Soyka LA, Fairfield WP, Klibanski A. Clinical review 117: Hormonal determinants and disorders of peak bone mass in children. J Clin Endocrinol Metab 2000;85:3951-63. [Google Scholar]
- 8.Mondy K, Tebas P. Emerging bone problems in patients infected with human immunodeficiency virus. Clin Infect Dis 2003;36 Suppl 2:S101-5. [Google Scholar]
- 9.Mondy K, Yarasheski K, Powderly WG, Whyte M, Claxton S, DeMarco D, et al. Longitudinal evolution of bone mineral density and bone markers in human immunodeficiency virus-infected individuals. Clin Infect Dis 2003;36:482-90. [Google Scholar]
- 10.Arnsten JH, Freeman R, Howard AA, Floris-Moore M, Lo Y, Klein RS. Decreased bone mineral density and increased fracture risk in aging men with or at risk for HIV infection. AIDS 2007;21:617-23. [Google Scholar]
- 11.Giannoudis P, Tzioupis C, Almalki T, Buckley R. Fracture healing in osteoporotic fractures: Is it really different? A basic science perspective. Injury 2007;38 Suppl 1:S90-9. [Google Scholar]
- 12.Aukrust P, Haug CJ, Ueland T, Lien E, Müller F, Espevik T, et al. Decreased bone formative and enhanced resorptive markers in human immunodeficiency virus infection: Indication of normalization of the bone-remodeling process during highly active antiretroviral therapy. J Clin Endocrinol Metab 1999;84:145-50. [Google Scholar]
- 13.Monier P, McKown K, Bronze MS. Osteonecrosis complicating highly active antiretroviral therapy in patients infected with human immunodeficiency virus. Clin Infect Dis 2000;31:1488-92. [Google Scholar]
- 14.Chokotho L, Harrison WJ, Lubega N, Mkandawire NC. Avascular necrosis of the femoral head in HIV positive patients-an assessment of risk factors and early response to surgical treatment. Malawi Med J 2013;25:28-32. [Google Scholar]
- 15.Matos MA, de Alencar RW, de Rocha Matos SS. Avascular necrosis of the femoral head in HIV infected patients. Braz J Infect Dis 2007;11:31-4. [Google Scholar]
- 16.Yin MT, McMahon DJ, Ferris DC, Zhang CA, Shu A, Staron R, et al. Low bone mass and high bone turnover in postmenopausal human immunodeficiency virus-infected women. J Clin Endocrinol Metab 2010;95:620-9. [Google Scholar]
- 17.Brown TT, Qaqish RB. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: A meta-analytic review. AIDS 2006;20:2165-74. [Google Scholar]
- 18.Grund B, Peng G, Gibert CL, Hoy JF, Isaksson RL, Shlay JC, et al. Continuous antiretroviral therapy decreases bone mineral density. AIDS 2009;23:1519-29. [Google Scholar]
- 19.Rebolledo BJ, Unnanuntana A, Lane JM. Bilateral pathologic hip fractures associated with antiretroviral therapy: A case report. J Bone Joint Surg Am 2011;93:e78. [Google Scholar]
- 20.Bonfanti P, De Vito A, Ricci E, Menzaghi B, Orofino G, Squillace N, et al. Bone safety of Dolutegravir-containing regimens in people living with HIV: Results from a real-world cohort. Infect Drug Resist 2020;13:2291-300. [Google Scholar]









