Scapular fracture should be considered in case of shoulder pain after seizure.
Dr. Varun Chouhan, Department of Orthopaedics, Bombay Hospital, Indore, Madhya Pradesh, India. E-mail: drvarunchouhan@yahoo.co.in
Introduction: Bilateral scapular fractures are a very rare injury with only few cases reported in the literature. They are said to be consequence of a violent trauma to the upper part of shoulder or as a result of electrocution or seizures. Glenoid involvement or open scapular fractures are one of the indications for operative treatment in these injuries, in other cases, simple immobilization is sufficient to obtain good results. Here, we report a case of a bilateral scapular fracture following an epileptic seizure, discussing the mechanism and outcome of conservative treatment.
Case Report: A 450-year-old healthy man with new-onset seizure with upper backache and bilateral shoulder pain, X-ray, and computed tomography (CT) with 3D reconstruction confirmed fracture of neck and body of bilateral scapula. Treatment consisted of immobilization with simple sling for both shoulders for 4 weeks, followed by early rehabilitation by pendular movements then gradually passive and active exercises of amplitude crossing were started at week 3. At 12-month follow-up, there was good clinical and radiological evolution with good resumption of activities.
Conclusion: Bilateral scapular fracture is a rare injury. Scapular fractures should be considered a potential etiology for shoulder and upper back pain following seizure activity. Scapular fracture can be missed easily on plain radiographs. Hence, CT scan with 3D reconstruction is very important in such cases. Treatment of the majority of scapular fractures without intraarticular extension remains to be conservative by simple immobilization. Surgical fixation is reserved for fractures at risk of joint complications or open lesions that would require surgical treatment, because of their long-term functional impact.
Keywords: Scapular fracture, bilateral scapular fracture, epilepsy, seizures.
Scapular fracture is rare clinical entity, only 5% of shoulder fractures and 1% of whole skeletal injuries [1]. Bilateral scapular fractures are a very rare injury with only few cases reported in the literature [2, 3]. They are said to be consequence of a violent trauma to the upper part of shoulder or as a result of electrocution or seizures. Glenoid involvement or open scapular fractures are one of the indications for operative treatment in these injuries, in other cases, simple immobilization is sufficient to obtain good results [4]. Here, we report a case of a bilateral scapular fracture following an epileptic seizure, discussing the mechanism and outcome of conservative treatment.
A 45-year-old healthy man with no significant medical history presented to the emergency department after new-onset seizure, he had complaints of post-ictal confusion, irrelevant talks, and pain over both shoulder and upper back. On examination, he had an improving post-ictal state, tenderness on palpation, and movement of both shoulders, greatest posteriorly. The patient was investigated for complete blood count, urine R/M, coagulation profile, serum electrolytes, random blood glucose, serum calcium, serum inorganic phosphorus, alkaline phosphatase, 25-hydroxy Vit. D, magnetic resonance imaging (MRI) brain, and electroencephalogram (EEG) with sleep record. Investigation reported hypocalcemia (Ca2+: 8.00 mg/dL and 25-Hydroxy Vit-D: 10.60 ng/mL). The patient was further assessed with X-ray of scapula which revealed comminuted fracture of the body of both scapula and computed tomography (CT) with 3D reconstruction confirmed fracture of the neck and body of the bilateral scapula (Fig. 1). 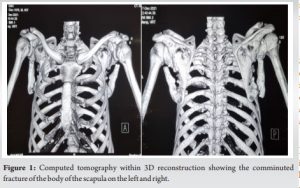
Scapular fracture is a rare lesion. It is often associated with serious pulmonary injury. Direct trauma to the posterior part of the thorax by road accident, work accident, assault, and fall was mentioned as the most frequent cause of this [5]. Bilateral scapular fracture is a very rare injury. Most of these fractures result from high-energy trauma, electrical shock, or epileptic seizure [6]. The significant musculature contraction occurring during the tonic phases of seizures is of the greatest force in the axial and proximal extremity muscle groups that may lead to fractures that occur unrelated to those occurring from direct impact trauma. Scapular fractures can be easily missed in the presence of other obvious injuries in patients with seizures. Hence, patients with history of seizures should always be examined with the possibility of scapular fractures in mind. Identifying scapular fractures on plain film radiography may be challenging, missing up to 43% of fractures in patients suffering from traumatic injuries [7]. Seizures have been identified as associated with a delay in diagnosis compared to those patients who experienced typical traumatic mechanisms [8]. Dedicated scapula view radiographs or preferably CT scans will identify potentially occult scapula fractures and should be strongly considered an additional possible etiology for shoulder and upper back pain following seizure activity [9]. Most frequent fractures of the scapula are those of the body, 35–45%; followed by the neck 25%, then of the acromion 8–12%; of the spine 5–11%, of the glenoid 10%, and the coracoids process 5–7%. Different classifications of scapular fractures are based on different and complementary criteria: Descriptive, anatomical, functional, and even surgical. CT with 3D reconstruction could be of capital importance in the description of the fracture line and eliminate an articular component of the glenoid cavity [10].
Operative treatment indications include:
- Displaced intra-articular glenoid fractures involving >25% of the articular surface, with or without subluxation
- Scapular neck fracture with >40° angulation or 1 cm medial translation
- Scapular neck fracture with an associated displaced clavicle fracture
- Fractures of the acromion that impinges on subacromial space
- Fractures of coracoids process that result in a functional acromioclavicular separation
- Comminuted fracture of the scapular spine.
Treatment of most scapula fractures which are extra-articular requires just simple immobilization until acute pain is gone, followed by active rehabilitation. Immobilization can be provided with an orthosis or sling for 3 weeks, followed by mobilization as soon as possible to reduce the risk of shoulder stiffness. In case of scapular fracture secondary to seizure, the patient has to investigated from the cause of seizure which might include MRI of the brain, serum electrolytes, serum calcium level, and EEG.
Bilateral scapular fracture is a rare injury. Scapular fractures should be considered a potential etiology for shoulder and upper back pain following seizure activity. Scapular fractures can be missed easily on plain radiographs. Hence, CT scan with 3D reconstruction is very important in such cases. Treatment of the majority of scapular fractures without intra-articular extension remains to be conservative by simple immobilization. Surgical fixation is reserved for fractures at risk of joint complications or open lesions that would require surgical treatment, because of their long-term functional impact. Long-term sequelae are rare after well-conducted early rehabilitation.
Scapular fractures should be considered a possibility for shoulder and upper back pain following seizure activity. Scapular fractures can be missed easily on plain radiographs. Hence, CT scan with 3D reconstruction is very important in such cases.
References
- 1.Zengui et al.; AJCRS 2021;6:6-10; AJRCS. 64669 [Google Scholar]
- 2.Henry JE, Beveridge CR, Horner I. Bilateral scapular fracture and triceps tendon rupture after a grand mal seizure: A case report. JBJS Case Connect 2013;3:e35. [Google Scholar]
- 3.Betten DP, Batson IS, Babiarz LN, Owen KN. Bilateral scapular fractures occurring as a result of a first-time seizure. Case Rep Emerg Med 2022;2022:9186275. [Google Scholar]
- 4.Brown MA, Sikka RS, Guanche CA, Fischer DA. Bilateral fractures of the scapula in a professional football player: A case report. Am J Sports Med 2004;32:237-42. [Google Scholar]
- 5.Bartonicek J, Fric V. Scapular body fractures: Results of operative treatement. Int Orthop 2011;35:747-53. [Google Scholar]
- 6.Liaw YH, Pollack A. Bilateral scapular fractures from electrical injury. Aust N Z J Surg 1996;66:189-90. [Google Scholar]
- 7.Harris RD, Harris JH Jr. The prevalence and significance of missed scapular fractures in blunt chest trauma. AJR Am J Roentgenol 1988;151:747-50. [Google Scholar]
- 8.Berritto D, Pinto A, Russo A, Urraro F, Laporta A, La Porta M, et al. Scapular fractures: A common diagnostic pitfall. Acta Biomed 2018;89 Suppl 1:102-10. [Google Scholar]
- 9.Tadros AM, Lunsjo K, Czechowski J, Abu-Zidan FM. Causes of delayed diagnosis of scapular fractures. Injury 2008;39:314-8. [Google Scholar]
- 10.Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zolodzki M, et al. Mapping of scapular fractures with three dimensional computed tomography. J Bone Joint Surg Am 2009;91:2222-8. [Google Scholar]








