Even when there is an accompanying sensory impairment, we advise against quickly exploring the nerve in all cases of Monteggia fracture–dislocation.
Dr. Naveen Sathiyaseelan, Department of Orthopaedic Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: spnaveen17@gmail.com
Introduction: Uncommon complication of Monteggia fracture is associated PIN palsy. The PIN palsy following Monteggia fracture–dislocation is neuropraxias and will recover spontaneously.
Case Reports: Two cases who were diagnosed as Monteggia fracture–dislocation with PIN palsy and associated superficial branch of radial nerve injury – Power 0/5 and sensations 0/2 were taken up for surgery (open reduction internal fixation of fracture of ulna + closed reduction of radial head). By the end of 7 weeks, both sensory and motor power were fully recovered spontaneously in both the cases.
Discussion: Most of the PIN injuries following Monteggia fracture–dislocation are neuropraxias and will recover spontaneously after closed reduction of radial head without any intervention to the nerve. The nerve needs to be intervened if there are no signs of recovery by 3 months. The time frame for the nerve to be intervened remains controversial.
Conclusion: In both of our cases, the injury is probably proximal to the terminal division of radial nerve and the injuries were neuropraxias and have recovered spontaneously. Hence, we suggest not exploring the nerve in all cases with Monteggia fracture–dislocation immediately even when there is associated sensory deficit.
Keywords: Monteggia fracture–dislocation, PIN palsy, neuropraxia.
Monteggia fracture–dislocation was defined by Giovanni Monteggia, long ago as proximal 1/3rd of ulna fracture associated with radial head dislocation [1]. It is usually seen in children of age 4–10 years. However, it can also occur in adults. Incidence in adults is 1–2% of forearm fractures [2]. Most common nerve injury of Monteggia fracture at the time of presentation is with associated posterior interosseous nerve (PIN) palsy [3]. Incidence of PIN palsy ranges from 3.1% to 31.4% [4]. However, most of the nerve injuries are neuropraxias and usually will recover spontaneously after either conservative treatment or open reduction with internal fixation [5]. However, the time frame for the nerve to be intervened remains controversial [6]. In this study, two cases that had PIN injury with associated superficial branch of radial nerve injury immediately following Monteggia fracture–dislocation were studied and observed.
Case Report 1:
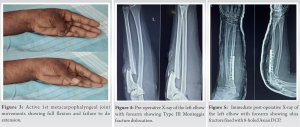
A 26-year-old male came to our hospital with an alleged history of road traffic accident (RTA) – skid and fall from two wheeler and sustained injury to left elbow presenting with He had an open wound of size 5 × 2 × 1 cm present over the dorsum of proximal 1/3rd of the left forearm (Fig. 1). Deformity presents. Swelling and tenderness present over the proximal 1/3rd of ulna. All range of movements of the left elbow was severely restricted and painful. Active wrist movements present (Fig. 2).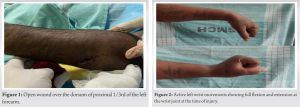
Case Report 2
A 36-year-old female came to our hospital with an alleged history of road traffic accident (RTA) – Auto versus two wheeler 1 day back and sustained injury to right elbow presenting with. No external injuries noted. Deformity was present. Swelling and tenderness present over the proximal 1/3rd of ulna. All range of movements of the right elbow was severely restricted and painful. Active wrist movements present. At 1st metacarpophalangeal joint full flexion is possible (Power-5/5), but extension was unable to do (Power-0/5). Sensations were reduced over the 1st dorsal web space (Grade – 0/2). X-ray was taken and diagnosed as right Monteggia fracture–dislocation (Bado’s Type – III). Open reduction internal fixation with plate osteosynthesis for right proximal 1/3rd ulna shaft fracture was done after 40 h from injury. Checked under C-Arm and found to see radial head was relocated and was in correct position. Above elbow POP application was applied in supination position for 4 weeks. The patient was followed up and examined weekly once. After 5 weeks of fixation, the patient sensations were improved fully (grade – 2/2) and the motor power improved to 3/5. POP was removed and patient was advised to use dynamic cock-up splint. After a total of 7 weeks, on examining, the patient sensations were fully intact (2/2) and motor power improved to 5/5. Fracture union was seen on 3rd month post-operative X-ray and full range of movements of the right elbow obtained.
PIN palsy can occur following Monteggia fracture–dislocation due to direct trauma, entrapment of nerve between ulna and radius, compression at arcade of Forsche and also stretching around the radial neck while doing closed reduction [7]. Unreduced radial head leads to tardy PIN palsy. There are several classifications for Monteggia fracture–dislocation, out of which Bado’s is the most commonly used. Bado’s classified into Type I, II, III, and IV based on the radial head dislocation into anterior, posterior, lateral, and associated proximal 1/3rd radius fracture, respectively [8]. This classification is mainly based on the mechanism of injury and also subdivided into true Monteggia fracture–dislocation (four types) and equivalent lesions. Out of these, Type – I and Type III are most commonly seen. Most of the PIN injuries following Monteggia fracture–dislocation (All types) are neuropraxias and will recover spontaneously over a period of time after closed reduction of radius [9]. Literature suggests that failure to reduce a dislocated radial head may be due to interposed structures such as capsule, intra-articular fractures, annular ligament, and PIN nerve [10]. In such cases of failure to reduce a dislocated radial head with PIN injury, exploration of nerve should also be done as there are high chances of PIN obstructing the reduction and forceful reduction can lead to complete tear of PIN. This is usually seen in Type III Monteggia fracture–dislocation as lateral dislocation of radial head leads to PIN slide posteriorly to radial head. Any attempt to relocate the radial head in such cases may cause PIN to interposed into the radiocapitellar joint. The time frame for the nerve to be intervened remains to be controversial [11]. Without the exploration of nerve, the grade can be assumed based on indirect evidences, from physical examination and electromyography (EMG) studies [12]. However, this could not be differentiate whether the nerve involved is stretched or entrapped. The physical examination can detect the clinical features such as sensory or motor weakness or dysfunction and can only indicate the location but not the morphology of nerve injury. In the same way, EMG studies at 4th week are useful in localizing the site of injury of nerve and also estimate the extent of injury. The disadvantage of EMG study is that the connective tissue component of nerve status cannot be assessed without the exploration of nerve [13]. To ensure the need for surgery, EMG studies should be done at 4th, 8th, and 12th week and compare the results. However, present examination and studies could not potentially help the surgeon to determine the need of early exploration of nerve in acute stages [14]. In the present study of two cases, patients not only had motor deficit but also sensations were reduced over the 1st dorsal web space indicating the superficial branch of radial nerve is also affected. This suggests that injury of nerve might be present before the bifurcation of radial nerve into superficial and deep branches. Literature shows that isolated PIN injury following Monteggia fracture–dislocation is neuropraxia and will recover spontaneously. In our study both the cases are Type III Monteggia fracture–dislocation, in Case I full sensory recovery has been obtained by 4 weeks and full motor recovery has been obtained by 6 weeks without any need for the exploration of nerve. In Case II, full sensory recovery has been obtained by 5 weeks and full motor recovery has been obtained by 7 weeks without any need for the exploration of nerve. This suggests that not only isolated PIN injury but PIN injury associated with superficial branch of radial nerve injury will recover spontaneously without any intervention. However, nerve needs to be explored and is considered as optimal treatment of choice if there are no signs of recovery after 3 months of injury.
In both of our cases of Monteggia fracture–dislocation with PIN injury with associated superficial branch of radial nerve injury, we have reported the injury is probably proximal to the terminal division of radial nerve and the injuries were neuropraxias and have recovered spontaneously. Hence, we suggest not to explore the nerve in all cases with Monteggia fracture–dislocation immediately even when there is associated sensory deficit.
We suggest not to explore the radial nerve in all cases with Monteggia fracture–dislocation immediately.
References
- 1.ElKhouly A, Fairhurst J, Aarvold A. The MonteggiaFracture: Literature review and report of a new variant. J Orthop Case Rep 2018;8:78-81. [Google Scholar]
- 2.Calderazzi F, Galavotti C, Nosenzo A, Menozzi M, Ceccarelli F. How to approach Monteggia-like lesions in adults: A review. Ann Med Surg (Lond) 2018;35:108-16. [Google Scholar]
- 3.Terra BB, Sassine TJ, Lima GF, Rodrigues LM, Padua DV, Nadai A. Radial head fracture associated with posterior interosseous nerve injury. Rev Bras Ortop 2016;51:725-9. [Google Scholar]
- 4.Yoshida N, Tsuchida Y. Posterior interosseous nerve palsy due to Bado Type-III Monteggia fracture. BMJ Case Rep 2018;2018:226254. [Google Scholar]
- 5.Matar HE, Akimau PI, Stanley D, Ali AA. Surgical treatment of Monteggia variant fracture dislocations of the elbow in adults: Surgical technique and clinical outcomes. Eur J Orthop Surg Traumatol 2017;27:599-605. [Google Scholar]
- 6.Quignon R, Marteau E, Penaud A, Corcia P, Laulan J. Posterior interosseous nerve palsy. A series of 18 cases and literature review. Chir Main 2012;31:18-23. [Google Scholar]
- 7.Hubbard J, Chauhan A, Fitzgerald R, Abrams R, Mubarak S, Sangimino M. Missed pediatric Monteggia fractures. JBJS Rev 2018;6:e2. [Google Scholar]
- 8.Bado JL. The Monteggia lesion. Clin Orthop Relat Res 1967;50:71-86. [Google Scholar]
- 9.Daurka J, Chen A, Akhtar K, Kamineni S.Tardy posterior interosseous nerve palsy associated with radial head fracture: A case report. Cases J 2009;2:22. [Google Scholar]
- 10.Ruchelsman DE, Pasqualetto M, Price AE, Grossman JA. Persistent posterior interosseous nerve palsy associated with a chronic Type I Monteggia fracture-dislocation in a child: A case report and review of the literature. Hand (N Y) 2009;4:167-72. [Google Scholar]
- 11.Sigamoney KV, Rashid A, Ng CY. Management of a traumatic posterior interosseous nerve palsy. J Hand Surg Am 2017;42:826-30. [Google Scholar]
- 12.Bulstra LF, Schep NW, van der Vlies CH. Posterior interosseous nerve palsy after closed proximal forearm fractures. Trauma Case Rep 2019;23:100240. [Google Scholar]
- 13.Maldonado AA, Amrami KK, Mauermann ML, Spinner RJ. Nontraumatic “isolated” posterior interosseous nerve palsy: Reinterpretation of electrodiagnostic studies and MRIs. J Plast Reconstr Aesthet Surg 2017;70:159-65. [Google Scholar]
- 14.Josten C, Freitag S. Monteggia and Monteggia-like-lesions: Classification, indication, and techniques in operative treatment. Eur J Trauma Emerg Surg 2009;35:296-304. [Google Scholar]