Exostosis rarely affects the foot or ankle but can cause debilitating effects to a patient’s life. Therefore, sesamoidal radiographical views are vital when investigating plantar-based symptoms
Dr. Nimra Akram, Department of Orthopaedics, University Hospitals of Leicester NHS Trust, Leicester, UK. E-mail: nimra.akram2@nhs.net
Introduction: Exostoses in the foot and ankle are extremely rare with no current literature of exostosis of the sesamoid bone.
Case Report: A middle-aged woman was referred to orthopedic foot surgeons following a long-standing issue of a painful non-fluctuant swelling beneath her left hallux with normal imaging. Repeat X-rays, with sesamoid views of the foot, were conducted due to the patient’s ongoing symptoms. The patient underwent a surgical excision and made a complete recovery. The patient is now able to comfortably walk for longer distances with no restrictions to her mobility.
Conclusion: Conservative management should be initially trialed to preserve the foot’s functions and limit the risk of surgical complications. As in this case, when surgical options are explored, it is critical to preserve as much of the sesamoid bone as possible to restore and sustain function.
Keywords: Orthopedics, trauma, foot, surgery, osteochondroma, exostosis.
An exostosis is a benign aberrant bone growth from the underlying old bone, which is derived from the Greek translation of ex (out of) and osteon (bone). Osteochondromas are a subset of exostoses, which are surrounded by an external cartilage layer commonly localized to the metaphysis of long bones [1]. Exostoses can be caused by the autosomal dominant disorder: Multiple hereditary exostoses (MHE), however, the majority are isolated benign growths hypothesized to be caused by skeletal dysplasia or neoplastic variations [1]. Localization to the foot and ankle is extremely rare and most exclusively occur as a result of an underlying background of MHE; thus, our case is the first of its kind to be reported of a rare exostosis in a sesamoid bone [2].
A middle-aged lady was referred from her general practitioner (GP) due to a 2-year history of a localized painful swelling beneath her left big toe with gradual onset and no previous known injury. She sought out various podiatric services (both under the public and private sectors) and had custom insoles produced to assist in her ongoing issue. Despite exhausting all conservative measures, the patient was reported to have persistent discomfort, particularly on weight bearing which severely limited the distance in which she could walk. The patient had a history of hypertension and hypercholesterolaemia, both of which were well-controlled pharmacologically.
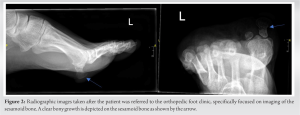
The biomechanics of an effective and normal functioning gait are composed of intricacies in anatomical function which rely heavily on the first metatarsophalangeal joint (MTPJ). This ginglymoarthrodial joint is relatively unstable due to the poor articulation between the metatarsal head and proximal phalanx and is vitally reinforced by the sesamoid complex to provide a more stable foundation [3]. The medial sesamoid is larger in comparison to its lateral counterpart and therefore bears more weight and is more susceptible to pathologies. It also allows for an insertion point for the abductor hallucis tendon, whereas the lateral sesamoid attaches to the adductor hallucis muscle [4]. The intricacy of the sesamoid complex allows for increased power of plantarflexion and therefore aids in the motion of walking by enabling the movement of intrinsic foot flexors and the elevation of the first metatarsal head [3]. Debilitating and painful sesamoids usually present in a complex manner and can be difficult to isolate-specific sesamoid pathologies due to the ambiguity of the presenting complaint and clinical signs. The most common sesamoid disorders include sesamoiditis, fractures, repetitive stress injury, osteoarthritis, and osteochondritis [5]. The prompt use of imaging can assist in isolating sesamoid issues and allow for timely management. Conservative management is the predominant proposition to most sesamoid issues, but indeterminate issues commonly lead to surgical intervention [6], such as in our case. As osteochondromas are formed from the endochondral ossification of the primary bone cartilage (with a consistent medullary cavity), these benign bone tumors usually affect long bones [7, 8]. The incidence of exostosis is difficult to interpret as the majority of patients are asymptomatic and most cases are diagnosed in children and adolescents [9]. There are limited reports of cases showing exostosis in the foot or ankle, excluding cases of MHE [2]. Sesamoidectomy is rarely performed due to the close proximity of essential surrounding structures and risks of significant complications including development of hallux valgus, reduced range of motion in the first MTPJ, and weakness in plantarflexion [10]. As in this case, a prudent approach was taken to ensure that the remaining normal medial sesamoid bone was retained to inhibit the high risk of complications associated with a complete sesamoidectomy.
With no previous cases to our knowledge of exostosis formation in the sesamoid bone, conservative treatment such as analgesia, rest, and orthotics had already been trialed. Given the severity of the symptoms and the impact on the patient’s ability to comfortably walk long distances, surgical excision was deemed the best course of action. Particular care was taken to ensure that the full exostosis from the medial sesamoid was excised to prevent recurrence and preserve as much of the foot’s biomechanical function as possible.
Conservative management is a key in initial management of sesamoid pathologies. Sesamoidal views are vital when investigating plantar-based foot symptoms, as normal foot views (AP and lateral) can easily miss sesamoid pathologies. Exostosis rarely affects the foot or ankle but can cause debilitating effects to a patient’s life. Surgical intervention of sesamoid exostosis can cause serious complications to the foot and if considered, the operating surgeon should focus on preserving as much of the sesamoid bone as possible.
References
- 1.Parvizi J, Kim G. Osteochondroma. In: High Yield Orthopaedics. 2010. p. 340-1. [Google Scholar]
- 2.Herrera-Perez M, Aciego De Mendoza M, De Bergua-Domingo JM, Pais-Brito JL. Osteochondromas around the ankle: Report of a case and literature review. Int J Surg Case Rep 2013;4:1025-7. [Google Scholar]
- 3.Mason LW, Molloy AP. Turf toe and disorders of the sesamoid complex. Clin Sports Med 2015;34:725-39. [Google Scholar]
- 4.Lombard C, Gillet R, Rauch A, Germain E, Dodin G, Blum A, et al. Hallux sesamoid complex imaging: A practical diagnostic approach. Skeletal Radiol 2020;49:1889-901. [Google Scholar]
- 5.Boike A, Schnirring-Judge M, McMillin S. Sesamoid disorders of the first metatarsophalangeal joint. Clin Podiatr Med Surg 2011;28:269-85, vii. [Google Scholar]
- 6.Sims AL, Kurup HV. Painful sesamoid of the great toe. World J Orthop 2014;5:146-50. [Google Scholar]
- 7.Bailescu I, Popescu M, Sarafoleanu LR, Bondari S, Sabetay C, Mitroi MR, et al. Diagnosis and evolution of the benign tumor osteochondroma. Exp Ther Med 2022;23:103. [Google Scholar]
- 8.de Souza AM, Bispo Júnior RZ. Osteochondroma: Ignore or investigate? Rev Bras Ortop 2014;49:555-64. [Google Scholar]
- 9.Gaumer GR, Weinberg DS, Collier CD, Getty PJ, Liu RW. An osteological study on the prevalence of osteochondromas. Iowa Orthop J 2017;37:147-50. [Google Scholar]
- 10.Shimozono Y, Hurley ET, Brown AJ, Kennedy JG. Sesamoidectomy for hallux sesamoid disorders: A systematic review. J Foot Ankle Surg 2018;57:1186-90. [Google Scholar]









