Investigations, diagnosis, treatment of acute COVID-related hip arthritis.
Dr. Dimitrios Kalavrytinos, Department of Trauma & Orthopaedic, Mid and South Essex NHS Foundation Trust, Basildon and Thurrock University Hospital, Nether Mayne, Basildon SS165NL. E-mail: dk.kalavritinos@gmail.com/dimitrios.kalavrytinos@nhs.net
Introduction: 2 years after the SARS-CoV-2 outbreak which is responsible for the COVID-19 pandemic, the clinical presentations remain unclear and unpredictable. The disease can present with a heterogeneous clinical course and a wide spectrum of clinical manifestations which can cause various complications from different systems, including musculoskeletal.
Case Report: The case of a young, fit, and healthy female patient with severe onset of hip pain which started only shortly after being tested positive for COVID-19 infection is presented in this study. There is no history of rheumatologic disease. Clinical assessment did not show any signs of erythema at the hip region, however, on palpation, there was significant tenderness at the anterior aspect of the left hip joint. The patient was unable to bare weight on this hip and could not straight leg raise, and the rotation of the hip was severely restricted due to underlying pain. The nasopharyngeal swabs for SARS-Vo2 were performed and came back positive. The CRP was 205 (μοναδα μετρησης ) and plain anteroposterior radiograph of the pelvis did not show abnormalities. A diagnostic aspiration under sedation in theaters was offered; the culture and enrichment were negative for infection. Since the symptoms were not improving with conservative measures, an open washout of the joint cavity was performed in theatres. The microbiologists guided on the antibiotic treatment and adequate analgesia was prescribed. Symptoms settled very soon after the open procedure and the requirements for analgesics were reduced to minimal use. The following couple of days, the pain, range of movement, and mobility significantly improved, and the patient returned within 2 weeks back to her normal activities. The rheumatologists organized a complete screening which ruled out elements of seronegative disease. In the final, 6-month follow-up, the patient was totally symptom free, and the blood markers were entirely unremarkable.
Conclusion: This is the first case of COVID-19-related, hip arthritis recorded worldwide, in a patient without any predisposing factors. Clinical suspicion is the key for early diagnosis and treatment for every COVID-19-positive patient with musculoskeletal symptoms, even for the patients with no history of autoimmune diseases. Viral-related arthritis remains a diagnosis of exclusion and underlies the importance to perform all the test to rule out other possible inflammatory arthritis. Our experience showed that early irrigation of the joint cavity is related with efficient symptoms relief, less requirement for analgesia, less time in hospital, and quicker return to daily activities.
Keywords: COVID, arthritis, acute, hip
The World Health Organization has reported more than 6.38 million deaths related to the COVID-19 pandemic [1]. The disease can appear with numerous atypical/uncommon clinical manifestations that can lead to late diagnosis and remain a challenge for the clinician. Various systems, including the musculoskeletal, can be affected and the complications can either settle early or last for a longer period or even become permanent. There is strong correlation between the different variants and the clinical presentation [2]. Crucial role to the clinical presentation of the COVID-19 demonstrates the variant that every time is responsible for the disease. Predominant musculoskeletal symptoms include arthralgia and myalgia. There is also established evidence that the virus can either trigger undiagnosed rheumatologic conditions or be responsible for the exacerbation of a previously controlled disease. Arthralgia is a well-reported side effect of COVID-19 vaccine [3, 4, 5]. The current paper presents the case of a young patient, without background of rheumatologic disease or any comorbidities, with acute, severe onset of hip pain which started only shortly after being tested positive for COVID-19. The diagnostic approach, management, and follow-up are presented followed by a literature review.
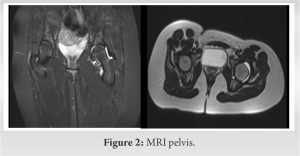
We present the case of a 20-year-old white female patient, previously fit and healthy with sudden onset of left hip pain. Symptoms started a day before presentation to accident and emergency and 9 days after tested positive for COVID-19. The pain progressively deteriorated and at presentation was unable to weight bear. On assessment, the left hip joint was in 15° of flexion and 20° of external rotation. The area was not warm to the touch and there was no erythema. On palpation and leg roll, the groin was significantly tender and the patient was unable to straight leg raise. There was no focal neurology and the perfusion of the leg was normal. The patient denied any history of trauma. 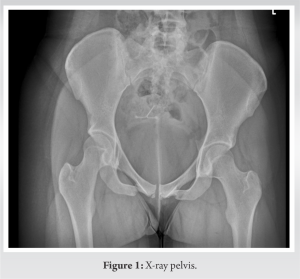
The SARS-CoV-2 virus infection is expressed predominantly by respiratory complications, however, can also be responsible for extra-pulmonary symptoms [6]. More than 570 cases have been reported since the outbreak of the pandemic and the continuously raising number causes uncertainty regarding the long-term complications [1]. The complications from the musculoskeletal system may require medical attention and the severity can require some form of intervention. Immunocompromised patients and those suffering from autoimmune disease are considered more vulnerable when exposed to the virus and can suffer more severe complications. Despite the large number of cases reported globally, only 9 cases of acute monoarthritis in which there is no history of other rheumatic diseases have been reported in the literature. Among those cases, there is not a single case that involves pathology of the hip joint [6, 7, 8, 9]. Therefore, the case presented in the current paper is the first COVID-19-related acute monoarthritis, reported worldwide. We found the case of a young, fit, and healthy female patient presented in this study, a diagnostic challenge and we would like to share the management that can be of exceptional value to the clinicians that can come across similar situations. Those patients with sudden presentation of monoarthritis should be screened routinely for COVID-19 infection. An updated diagnostic algorithm for acute monoarthritis, taking under consideration, the SARS-CoV-2 virus would lead to earlier diagnosis, more efficient planning of the treatment and would reduce the morbidity and the length of stay in the hospital and therefore minimizing the cost of care providing by the health-care systems. Our experience showed that after the open irrigation of the joint, the symptoms immediately settled and the patient very soon reported excellent recovery and returned her daily activities. Regarding management, comparing to the other reported cases which have been treated conservatively with IV antibiotics, our approach was surgical with open wash out. Both treatment plans have good outcomes and the patients returned back to their daily activities. However, surgical management seems to help symptoms settle quicker as from the 1st post-operative day, there was a significant improvement of the symptoms and reduced the duration of hospitalization.
Viral-related arthritis remains a diagnosis of exclusion and underlines the importance to perform all the tests to rule out the possibility of serum negative arthritis. Negative joint fluid cultures and negative rheumatologic screening (rheumatoid factor, antinuclear antibody, anti-citrullinated protein antibody, and HLA-B27) are essential [10]. This case argued that clinical suspicion is the key of the early diagnosis and treatment for every COVID-19-positive patient with musculoskeletal symptoms, even for the patients with no history of autoimmune diseases.
Clinical suspicion and expansion of the differential diagnosis are the keys to diagnose the cause of arthritis to patients without predisposing factors. MDT is a crucial necessity for treatment and diagnosis in additional to surgical intervention.
References
- 1.According to WHO, Weekly Epidemiological Update on COVID-19-27 July 2022. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---27-july-2022. [Last accessed on 27 Jul 2022]. [Google Scholar]
- 2.Ahmed S, Gasparyan AY, Zimba O. Comorbidities in rheumatic diseases need special consideration during the COVID-19 pandemic. Rheumatol Int 2021;41:243-56. [Google Scholar]
- 3.Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, et al. Musculoskeletal consequences of COVID-19. J Bone Joint Surg Am 2020;102:1197-204. [Google Scholar]
- 4.Ono K, Kishimoto M, Shimasaki T, Uchida H, Kurai D, Deshpande GA, et al. Reactive arthritis after COVID-19 infection. RMD Open 2020;6:e001350. [Google Scholar]
- 5.An QJ, Qin DA, Pei JX. Reactive arthritis after COVID-19 vaccination. Hum Vaccin Immunother 2021;17:2954-6. [Google Scholar]
- 6.Conway R, Konig MF, Graef ER, Webb K, Yazdany J, Kim AH. Inflammatory arthritis in patients with COVID-19. Transl Res 2021;232:49-59. [Google Scholar]
- 7.Parisi S, Borrelli R, Bianchi S, Fusaro E. Viral arthritis and COVID-19. Lancet Rheumatol 2020;2:e655-7. [Google Scholar]
- 8.Saricaoglu EM, Hasanoglu I, Guner R. The first reactive arthritis case associated with COVID-19. J Med Virol 2021;93:192-3. [Google Scholar]
- 9.Yokogawa N, Minematsu N, Katano H, Suzuki T. Case of acute arthritis following SARS-CoV-2 infection. Ann Rheum Dis 2021;80:e101. [Google Scholar]
- 10.Gasparotto M, Framba V, Piovella C, Doria A, Iaccarino L. Post-COVID-19 arthritis: A case report and literature review. Clin Rheumatol 2021;40:3357-62. [Google Scholar]