A very large osteolytic lesion with cortical expansion and septations near the articular region may not always be a bone tumor or bone infection. A large subchondral cyst may also be considered as a possibility.
Dr. Sivabalaganesh Amirthalingam, Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: sivabalaganeshamirthalingam@gmail.com
Introduction: Osteoarthritis is now understood to be an aberrant remodeling of the joint organ caused by wear-and-tear mechanism and by a variety of inflammatory mediators. Subchondral cysts have been one of the important radiological features of knee osteoarthritis that is not well understood. We report a case of large subchondral lytic lesion which was initially thought to be a giant cell tumor and later was identified as subchondral cyst.
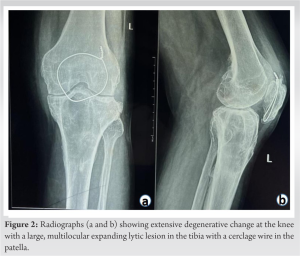
Case Report: A 50-year-old man presented to the outpatient department with complaints of intermittent pain and swelling over the left knee associated with difficulty in performing his daily activities Patient had undergone cerclage wiring for fracture left patella fracture 8 years back following which pain started. Radiographs showed extensive degenerative change at the knee with a large, multilocular lytic lesion in the proximal tibia. Magnetic resonance imaging showed similar features with an additional lesion in the distal femur. Core needle biopsy and histopathological examination of both lesions showed fibrocollageous tissue with bone fragments and lymphocytes. Patient was treated conservatively with analgesics and physiotherapy. He had good relief of pain and is on regular follow-up till date.
Discussion: Osteoarthritis knee is the most prevalent and leading cause of pain and disability worldwide. Subchondral cysts are strongly associated with osteoarthritis. Articular cartilage damage in osteoarthritis exposes the subarticular bone to injury, particularly in the weight-bearing joints. Large cysts are a well-recognized feature of other disorders such as simple bone cyst, aneurysmal bone cyst, giant cell tumor, and osteomyelitis. As these cases are rarely reported the treatment options are not standardized. Studies had shown similar cases treated both conservatively and surgically. The occurrence of the pathological fracture in these cases is high so prophylactic surgical fixation of massive geodes is advised. We decided to treat our case conservatively with analgesics and physiotherapy. The patient has good relief of pain at present and is on regular follow-up. He has been counseled that he may need a total knee replacement in the future if pain increases in severity.
Conclusion: In the presence of osteolytic lesion showing very large cyst with cortical expansion and septations in radiographs with adjacent joint arthritis, the diagnosis of subchondral cyst/Geode should be strongly considered.
Keywords: Proximal tibia geode, osteolytic lesion of proximal tibia, subchondral cyst, proximal tibia geode conservative management.
Osteoarthritis is now understood to be an aberrant remodeling of the joint organ caused by wear-and-tear mechanism and by a variety of inflammatory mediators [1]. Osteoarthritis of the knee is a degenerative joint organ disease causing significant morbidity and its prevalence has increased in the past years [2]. Subchondral cysts are one of the important radiological features of knee osteoarthritis that is not well understood [3]. The presence of a large subchondral lytic lesion in a radiograph will alarm the surgeon’s to think of bone tumors or bone cyst [4]. We report a case of large subchondral lytic lesion which was initially thought to be a giant cell tumor and later was identified as subchondral cyst.
A 50-year-old man presented to our out-patient department with complaints of intermittent pain and swelling over the left knee associated with difficulty in performing his daily activities. The knee pain started following the cerclage wiring for fracture left patella done 8 years back. A longitudinal surgical scar of 8 cm healed by primary intention was present over anterior aspect of knee (Fig. 1a).
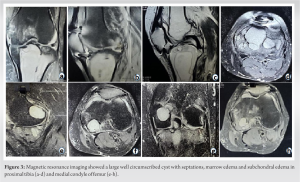
Osteoarthritis knee is the most prevalent and leading cause of pain and disability worldwide [2]. The prevalence increases with age and it is strongly associated with aging and physical activity [5]. Subchondral cysts are radiolucent cystic lesions adjacent to joint surface commonly associated with osteoarthritis but it can be also seen in rheumatoid arthritis, avascular necrosis of the femoral head, and calcium pyrophosphate deposition disease [6]. The etiology of subchondral cysts is strongly associated with osteoarthritis. Delamination of articular cartilage in osteoarthritis exposes the subarticular bone to injury, particularly in the weight-bearing joints [7]. Seepage of synovial fluid into the subarticular bone leads to formation of cysts which may be walled off when the denuded articular cartilage is replaced with fibrous tissue. Large cysts are a well-recognized feature of other inflammatory disorders. In rheumatoid arthritis subchondral cysts may attain a considerable size, especially if physical activity is maintained. Calcium pyrophosphate deposition disease may produce large cysts that are histologically identical to those associated with primary osteoarthritis [8]. Pigmented villonodular synovitis of the knee occasionally results in bony erosions, which may be extensive [9]. Subchondral intraosseous ganglia have some similar radiological features to degenerative cysts. However, they are not associated with osteoarthritis, rarely communicate with the joint space, and tend to occur adjacent to non-weight-bearing surfaces of the joint [10]. Freund in 1940 was the first investigator to suggest that elevated intra-articular pressure might lead to seeping of joint fluid through gaps in the articular surface with secondary resorption of bony trabeculae [11]. Landell suggested that they form when synovial fluid is pumped through defects in the attenuated cartilage and sub-articular cortical plate, causing a gradually expanding lesion in the underlying trabecular bone [12]. Rhaney and Lamb proposed that necrosis of trabecular bone precedes fracture of the subchondral bony plate and results from the increase in transmitted pressure through articular surface that is devoid of cartilage. This theory receives support from experiments performed by Ondrouch, in which lines of stress were observed in a photoelastic material subjected to varying loads [13]. Ferguson noted the resemblance of the tissue elements about the cystic lesions to those seen in fracture callus, lending support to the theory of primary cystic necrosis of bone. He stressed that communication between the cavity and articulate surface was a secondary phenomenon related to unroofing of the cyst. Dürr et al. proposed that stress-induced microfractures of the subchondral bone may be primary events in the development of subchondral bone cysts in OA [14]. Glass et al. reported a huge multiloculated, expanding subchondral cyst involving most of the medial tibial plateau in a patient with osteoarthritis following medial meniscectomy. In this case, CT demonstrated posterolateral extension of the lesion and disruption of the expanded posterior cortex [15]. Cyst formation as a result of ingrowth of synovium or synovial metaplasia, as proposed by some, is not supported by the histological character of the cyst lining which is fibrous rather than synovial. Our case and those reported by Ostlere et al., Resnick and Glass et al. share certain radiologic features: (1) The lesions were lytic, well defined, and adjacent to the medial tibial cortex; (2) other changes indicating moderate osteoarthritis of the medial tibiofemoral joint were present; and (3) the lesions were elliptical with the long axis in the sagittal plane. Recognition of these features may be important in distinguishing large degenerative cysts from tumor [6,15]. If further imaging assessment is needed, CT may provide valuable information that is not available in radiographs. As these cases are rarely reported the treatment options are not standardized. Studies had shown similar cases treated both conservatively and surgically. The occurrence of the pathological fracture in these cases is high so prophylactic surgical fixation of massive geodes is advised [8]. Novel surgical treatment options for subchondral bone abnormalities and cartilage include both biological and structural components. Marrow stimulation methods such as K-wire drilling, Micro-fracturing, Nano-fracturing, and core decompression are among the biological components of therapy. This therapy also involves autologous platelet-rich plasma injections, adipose derivative treatment, and bone marrow cell injections. Sub-chondroplasty features include cement injections, allograft transplantation, bone marrow cell graft injections, and iliac crest bone grafting [16]. Percutaneous injection of bone cement under CT and fluoroscopy guidance appears to be a successful and safe therapy in the treatment of symptomatic subchondral cysts, with a considerable reduction in patient discomfort and a less intrusive approach than traditional surgical treatment [17]. We decided to treat our patient conservatively with analgesics and physiotherapy. Pain considerably reduced and patient was able to carry out his daily activities reasonably well. He is on regular follow-up and he has been explained that if pain becomes severe, he might need undergo a total knee replacement with stemmed tibial prosthesis in the future.
Large subchondral cysts/geodes in osteoarthritis may mimic bone tumors like giant cell tumor. In the presence of osteolytic lesion showing very large cyst with cortical expansion and septations in radiographs with adjacent joint arthritis, the diagnosis of subchondral cyst/Geode should be strongly considered.
Large subchondral geodes/cysts due to osteoarthritis may mimic giant cell tumors or metastatic lesions.
References
- 1.Hsu H, Siwiec RM. Knee Osteoarthritis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507884/. [Last updated on 2022 Sep 04]. [Google Scholar]
- 2.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med 2010;26:355-69. [Google Scholar]
- 3.Burnett WD, Kontulainen SA, McLennan CE, Hazel D, Talmo C, Wilson DR, et al. Knee osteoarthritis patients with more subchondral cysts have altered tibial subchondral bone mineral density. BMC Musculoskelet Disord 2019;20:14. [Google Scholar]
- 4.Purohit S, Pardiwala DN. Imaging of giant cell tumor of bone. Indian J Orthop 2007;41:91-6. [Google Scholar]
- 5.Pal CP, Singh P, Chaturvedi S, Pruthi KK, Vij A. Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop 2016;50:518-22. [Google Scholar]
- 6.Resnick D, Niwayama G, Coutts RD. Subchondral cysts (geodes) in arthritic disorders: pathologic and radiographic appearance of the hip joint. AJR Am J Roentgenol 1977;128:799-806. [Google Scholar]
- 7.Kaspiris A, Hadjimichael AC, Lianou I, Iliopoulos ID, Ntourantonis D, Melissaridou D, et al. Subchondral bone cyst development in osteoarthritis: From pathophysiology to bone microarchitecture changes and clinical implementations. J Clin Med 2023;12:815. [Google Scholar]
- 8.Maher LV. Geode of the tibia. J Clin Rheumatol 2016;22:41. [Google Scholar]
- 9.Ma X, Shi G, Xia C, Liu H, He J, Jin W. Pigmented villonodular synovitis: A retrospective study of seventy five cases (eighty one joints). Int Orthop 2013;37:1165-70. [Google Scholar]
- 10.Mohapatra A, Patel V, Choudhury P, Phalak M. Intraosseous ganglion cyst of the distal tibia: A rare entity in a rarer location. BMJ Case Rep 2018;2018:r-224395. [Google Scholar]
- 11.Freund E. The pathological significance of intra-articular pressure. Edinb Med J 1940;47:192-203. [Google Scholar]
- 12.andells JW. The bone cysts of osteoarthritis. J Bone Joint Surg Br 1953;35-B:643-9. [Google Scholar]
- 13.Rhaney K, Lamb DW. The cysts of osteoarthritis of the hip; a radiological and pathological study. J Bone Joint Surg Br 1955;37-B:663-75. [Google Scholar]
- 14.Dürr HD, Martin H, Pellengahr C, Schlemmer M, Maier M, Jansson V. The cause of subchondral bone cysts in osteoarthrosis: A finite element analysis. Acta Orthop Scand 2004;75:554-8. [Google Scholar]
- 15.Glass TA, Dyer R, Fisher L, Fechner RE. Expansile subchondral bone cyst. AJR Am J Roentgenol 1982;139:1210-1. [Google Scholar]
- 16.Gobbi A, Arbas AJ, Dallo, I. Proximal Tibial Subchondral Cystic Lesion Treatment with Osteo-Core-Plasty. Joint Function Preservation 2021;237–246. 10.1007/978-3-030-82958-2_21. [Google Scholar]
- 17.Bertrand AS, Schmid-Antomarchi H, Foti P, Nouri Y, Gérardin E, et al. Percutaneous Injection of Bone Cement (Cementoplasty) for the Treatment of Symptomatic Subchondral Cysts. Journal of Cell Science & Therapy. 2014;05:(4):176.10.4172/2157-7013.1000176. [Google Scholar]








