This article highlights the challenge differentiating distal tibia pain in professional Muay Thai athletes due to the high contact sport profile, the limited population in the literature, and an atypical presentation
Dr. Marco Pes, Department of Orthopaedic, University of Sassari, Sassari, Italy. E-mail: marco92pes@gmail.com
Introduction: Sports injuries occur during sport athletic activities, or exercising. However, there are some lesions which are typically associated to sports, in such a demanding and physical sport like Muay Thai that no typical lesion has been detected yet. We performed a narrative review of the literature to highlight the typical lesions of this sport to analyze the differential diagnosis of those conditions.
Case Report: A 28-year-old female, Muay Thai athlete since 16 years, presented with a 6 months history of a persistent pain in the metaphyseal lateral part of the right tibia. Differentiation between stress injuries, malignant bone tumors, and tumor-like lesions after repetitive microtrauma following sport activities can be difficult. The diagnostic approach involved conventional X-ray, echotomography, computed tomography scan, and magnetic resonance imaging scan with controversial findings. The biopsy confirmed the final diagnosis of non-ossifying fibroma.
Conclusion: The purpose of this case report is to exhibit the challenges in the diagnosis of a professional Muay Thai athlete with tibial pain and to discuss the clinical presentation of this type of patients with a limited population in the literature. Our case illustrates that even modern imaging techniques cannot always distinguish between tumor and tumor-like lesions caused by sports; meanwhile remembered us that we should never be too focused on a particular characteristic forgetting even rare pathologies as adamantinoma.
Keywords: Muay Thai, tumor-like, microtrauma, adamantinoma, non-ossifying fibroma
Sports injuries occur during sport athletic activities or exercising. However, there are some lesions which are typically associated to sports (like: Sports-related changes of the synovial membrane [1, 2], or more specifically, shoulder impingement for overhead sports players, knee instability for contact sports players, hamstring lesion for runners, and bone bruise lesions for marathon runners), in such a demanding and physical sport like Muay Thai that no typical lesion has been detected yet [2]. Muay Thai is a traditional martial art of Thailand that uses stand-up striking, along with various clinching techniques intended to throw an opponent to the ground. It promotes both physical and mental energy and requires the guide of instructors placing great emphasis on discipline, respect, and spirituality [3]. Muay Thai is referred to as the “Art of Eight Limbs” because it makes use of punches, kicks, and elbow and knee strikes [2]. The peculiarity for Thai fighters is the body kick, a basic technique that they master at a young age. What differentiates the Muay Thai body kick from other kicks is the use of the shin bone. While other styles often utilize the foot, Muay Thai fighters kick with their shin. Nowadays, little is known about the injuries and risk factors for injuries among Muay Thai fighters. Obtaining more information about the nature and frequency of injury in this sport provides part of the overall sports injury picture to improve the health and safety of Muay Thai fighters engaged in competition [2]. The purpose of this case report is to exhibit the challenges in the diagnosis of a professional Muay Thai athlete with distal tibial pain and to discuss the clinical presentation of this type of patients with a limited population in the literature [4]. We performed a narrative review of the literature to highlight the typical lesions of this sport and to analyze the differential diagnosis of those conditions.
A 28-year-old female, Muay Thai athlete since 16 years, was first seen in orthopedic clinic for a persistent pain in the metaphyseal lateral part of the right tibia that she was experiencing in the past 6 months. History was negative for other pathologies or familiar tumors. Clinical examination revealed mild swelling in the region, a feeble bruising, and a pain present on palpation of the distal two-thirds of the posterolateral tibial border. The pain was referred as persistent, with moment of sharpness not always relate with sport activity. The initial diagnostic approach was conventional radiology of the distal third of the right leg (Fig. 1), which showed sign of periosteal reaction and a thickening area, due, probably, to an osteoid osteoma according to the opinion of the radiologist.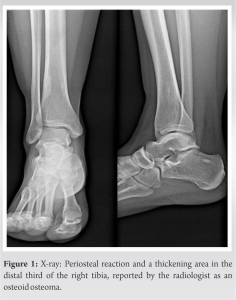
Sports injuries are injuries that occur during sport, athletic activities, or exercising. These activities by school-age children and young adults produce a significant amount of emergency medical use in the United States [8]. A common clinical presentation among those injuries, which may be difficult to diagnose, is chronic leg pain in weight-bearing athletes because pain in the foot, ankle, calf, or shin typically impedes activity and is non-specific in nature [9]. It is not uncommon to see arriving in academics center patients treated for persistent unexplained pain, the final diagnosis of which was a tumor. Revealing all the difficulty in diagnosing chronic sports pain, atypical or unrelated to a trauma during sports [10]. The clinical presentation of our patient leads us to think about a stress injury or a contusion, supported from Gartland et al. who refer that soft-tissue injuries have been shown to be the most common type of injury, contributing to at least 80–90% of all injuries in athletes [3]. Stress injuries represent a spectrum of injuries ranging from periostitis, caused by inflammation of the periosteum, to a complete stress fracture that includes a full cortical break. They are relatively common overuse injuries in athletes [11, 12]. Differential diagnosis in this type of patient can be challenging, even to experienced orthopedic surgeons and diagnosticians, particularly in young adults that because symptoms associated with these conditions often overlap [9]. Given the location and the clinical presentation, our differential diagnosis of exercise-induced leg pain also included: Medial tibial stress syndrome (MTSS), tibial stress fracture, chronic exertional compartment syndrome (CECS), and to a lesser extent popliteal artery entrapment and nerve entrapment (excluded from the beginning for her negative medical history) [13].
- MTSS is a frequent overuse lower extremity injury in athletes and military personnel. MTSS is an exercise-induced pain over the anterior tibia and is an early stress injury in the continuum of tibial stress fractures [14, 15].
- Tibial stress fractures can be difficult to distinguish from MTSS and are often part of the same continuum of tibial bone stress injury. Anterior cortex stress fractures are more common than posteromedial or posterolateral tibial stress fractures and are distinguished by point tenderness (<5 cm) along the tibia. Radiographs may reveal the “dreaded black line,” and MRI can help determine the severity of the stress injury [1, 11, 14].
- CECS is considered a disorder of muscular origin and presents similarly with exercise-induced lower extremity pain that is also diffusely located. It often involves both extremities, relieved by rest, and may have additional symptoms such as paresthesia, pallor, cold skin temperature, and loss of pulses in the distal lower extremity. CECS diagnosis is made by measuring intramuscular compartment pressures [13].
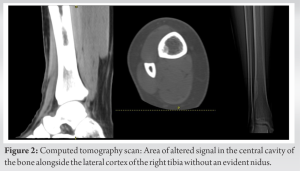
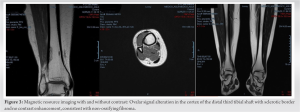
The initial diagnostic approach is always conventional radiology, which is inexpensive, widely available, and quick to perform. Despite the low sensitivity, radiography can reveal frank fractures or even abnormalities such as bone tumors and calcifications of the soft tissues [16]. The standard X-ray helped us to exclude some of our first hypothesis (stress injury) at the same time giving us new thoughts about the osteoid osteoma, which is common, benign osteoblastic tumors that can occur in any bone in the body. They are almost always solitary, with only rare reports of multiple tumors in the same patient [17]. Osteoid osteomas typically occur in the cortex of long bones of the lower extremities but can occur in any bone and can be intramedullary or sub-periosteal. In over 50% of the cases, they are located in the diaphysis of the femur or tibia with the proximal femur being the most frequently affected [18, 19]. While the clinical sign and the images were, in our opinion, uncertain, we decided to carry out further analysis including an echotomography and a CT scan. The radiologist’s suggestion of osteoid osteoma was disclaimed by the further examinations which instead advanced three hypotheses: FD, adamantinoma, or a NOF. Adamantinoma is a rare cancerous tumor, accounting for < 1% of all primary bone tumors. The World Health Organization (WHO) defines it as a biphasic tumor, characterized by a variety of morphological patterns [17, 18]. The tibia is the most affected bone and it is predominant in male patients between the second and third decades of life [16]. Imaging plays an important role in the diagnosis of bone tumors. Radiography is the most reliable diagnostic imaging method [3]. Typical lesions are in the anterior lateral axis of the tibia. They are eccentric, dilated, cortical or intramedullary soluble lesions with multilocular features, and sclerotic margins. Pathological fractures may occur. Anterior arch deformity of tibia is common [20]. According to Desai et al., location in the tibia with intracortical development is two diagnostic indicators for adamantinoma, furthermore, as Chen et al. wrote: Adamantinoma should be considered in any differential diagnosis of tibial cortical lesion, regardless of size, or benign sign [17]. For all those reasons, we did not excluded adamantinoma yet. The second hypothesis was FD, which is an uncommon and debilitating skeletal disorder resulting in fractures, deformity, functional impairment, and pain [21]. The disease may affect one bone (monostotic) or multiple (polyostotic), and may occur in isolation or in combination with cafe-au-lait spots and hyperfunctioning endocrinopathies, termed McCune-Albright syndrome [22]. Any part or combination of features is possible, giving rise to a phenotype that is complex and striking in its diversity. Besides clinical examination, FD is diagnosed based on the results of radiographic imaging and the microscopic histopathological findings. On CT scan, FD shows the characteristic “Ground-glass” appearance with well-defined borders. On MRI, FD has a low signal intensity on T1-weighted MRI and variable signal intensity on T2-weighted MRI [10]. The last one was NOF, classified as a tumor-like lesion grouped according to the histologic classification of bone tumors by the WHO [23], most lesions are discovered incidentally and show classic radiographic features within the long bones. There is no specific indication for MRI in cases of non-ossifying fibroma unless the radiographic appearance is atypical [24]. Diagnosis of NOF in the long bones is based on the radiographic characteristic and clinical appearance. Typically, the NOF appears as an asymptomatic multiloculated lesion often identified incidentally during radiographic evaluation indicated for another reason [21]. In general, are recognized two phases, in the early stage is more visible on imaging, due to the reactive rim, once it reaches the healed stage it becomes less visible on imaging (involutionary phase). Finally, to settle the doubt about the diagnosis, we ordered an MRI scan as well as a biopsy, the first highlighted oval signal alteration in the cortex of the distal third of the tibial shaft: Intermediate signal in T1 and long TR, with sclerotic border and no contrast enhancement; the biopsy reported spindle shaped fibroblasts arranged in storiform pattern, interspersed with osteoclast-like multinucleated giant cells, small cystic changes and areas of hemorrhage, and little inflammatory cells, compatible with NOF, achieving the diagnosis of non-ossifying fibroma.
Our case illustrates that even modern imaging techniques cannot always distinguish between tumor and tumor like lesions caused by sports activities; meanwhile remembered us that we should never be too focused on a particular characteristic forgetting even rare pathologies as adamantinoma. It also stresses the importance of correct techniques in sports like Muay Thai, the needs of greater awareness of risks in those athletes, and the urgency of more complete clinical studies which could lead to a reduction of unrecognized associated complications and a better management.
All the possible causes leading to anterior tibia pain should always be taken in consideration when approaching to an athlete. Differentiation between stress injuries, malignant bone tumors, and tumor like lesions after repetitive microtrauma following sport activities can be difficult. The common clinical presentation among those injuries is typically non-specific in nature.
References
- 1.Manunta AF, Zedde P, Pisanu F, Marras F. Sports-related changes of the synovial membrane. Joints 2014;2:181-7. [Google Scholar]
- 2.Strotmeyer S Jr., Coben JH, Fabio A, Songer T, Brooks M. Epidemiology of Muay Thai fight-related injuries. Inj Epidemiol 2016;3:30. [Google Scholar]
- 3.Gartland S, Malik MH, Lovell ME. Injury and injury rates in Muay Thai kick boxing. Br J Sports Med 2001;35:308-13. [Google Scholar]
- 4.Arikan Y, Dincel YM, Ozkul B, Ozcafer R, Kirat A, Ozer D. Painful transient edema in the tibial diaphysis: The challenges and the essence of biopsy in treatment. World J Surg Oncol 2018;16:106. [Google Scholar]
- 5.Manca A, Pisanu F, Ortu E, De Natale ER, Ginatempo F, Dragone D, et al. A comprehensive assessment of the cross-training effect in ankle dorsiflexors of healthy subjects: A randomized controlled study. Gait Posture 2015;42:1-6. [Google Scholar]
- 6.Manca A, Pisanu F, Ortu E, De Natale E, Ginatempo F, Dragone D, et al. Isokinetic cross-training effect in foot drop following common peroneal nerve injury. Isokinet Exerc Sci 2014;23:17-20 . [Google Scholar]
- 7.Pisanu F, Ortu S, Corda M, Andreozzi M, Caggiari G, Manunta AF, et al. Deltoid ligament reconstruction with autologous gracilis tendon in chronic medial ankle instability after ankle fracture surgery: A case report. Foot (Edinp) 2020;49:101714. [Google Scholar]
- 8.Burt CW, Overpeck MD. Emergency visits for sports-related injuries. Ann Emerg Med 2001;37:301-8. [Google Scholar]
- 9.Edwards PH, Wright ML, Hartman JF. A practical approach for the differential diagnosis of chronic leg pain in the athlete. Am J Sports Med 2005;33:1241-9. [Google Scholar]
- 10.Alkhaibary A, Alassiri AH, Alsalman M, Edrees S. Unusual presentation of fibrous dysplasia in an elderly patient. J Radiol Case Rep 2019;13:26-33. [Google Scholar]
- 11.Hazelwood SJ, Castillo AB. Simulated effects of marathon training on bone density, remodeling, and microdamage accumulation of the femur. Int J Fatigue 2007;29:1057-64. [Google Scholar]
- 12.Stress Reaction and Fractures. StatPearls; n.d . [Google Scholar]
- 13.Beck BR. Tibial stress injuries. An aetiological review for the purposes of guiding management. Sport Med 1998;26:265-79 [Google Scholar]
- 14.Mcclure CJ, Oh R, Army M. Medial tibial Stress Syndrome pathophysiology treatment. Management 2019;??? :1-5. [Google Scholar]
- 15.Yates B, White S. The Incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med 2004;32:772-80. [Google Scholar]
- 16.Zumárraga JP, Cartolano R, Kohara MT, Baptista AM, dos Santos FG, de Camargo OP. Tibial adamantinoma: Analysis of seven consecutive cases in a single institution. Acta Ortop Bras 2018;26:252-4. [Google Scholar]
- 17.De Ga K, Bateni C, Darrow M, McGahan J, Randall RL, Chen D. Polyostotic osteoid osteoma: A case report. Radiol Case Rep 2020;15:411-5. [Google Scholar]
- 18.Schneider S, Seither B, Tönges S, Schmitt H. Sports injuries: Population based representative data on incidence, diagnosis, sequelae, and high risk groups. Br J Sports Med 2006;40:334-9, discussion 339. [Google Scholar]
- 19.Senne J, Davis R, Yasin J, Brimmo O, Evenski A, Bhat A. Computed tomography guided radio-frequency ablation of osteoid osteomas in atypical locations. Indian J Radiol Imaging 2019;29:253. [Google Scholar]
- 20.Chen J, Zhang J. Adamantinoma filling the medullary space of the tibia: A case report. Radiol Case Rep 2019;14:1330-3. [Google Scholar]
- 21.Martinez SR, Gay MS, LZ . HHS Public Access. Physiol Behav 2016;176:139-48 . [Google Scholar]
- 22.Weinstein LS, Shenker A, Gejman PV, Merino MJ, Friedman E, Spiegel AM. Activating mutations of the stimulatory G protein in the McCune-Albright syndrome. N Engl J Med 1991;325:1688-95. [Google Scholar]
- 23.Shanmugaratnam K, Sobin LH. The world health organization histological classification of tumours of the upper respiratory tract and ear. A commentary on the second edition. Cancer 1993;71:2689-97. [Google Scholar]
- 24.Jee WH, Choe BY, Kang HS, Suh KJ, Suh JS, Ryu KN, et al. Nonossifying fibroma: Characteristics at MR imaging with pathologic correlation. Radiology 1998;209:197-202. [Google Scholar]










