The technique of autograft osteochondral transplantation, commonly used for OCD of the knee and talus, is a viable treatment option for the rare cases of traumatic, full-thickness osteochondral defects of the first metatarsal head in adolescent patients.
Dr. Joana Arcângelo, Department of Pediatric Orthopedic Surgery, CUF Descobertas Hospital, Lisbon, Portugal. E-mail: joana.arcangelo@gmail.com
Introduction: First metatarsophalangeal (MTP) joint mobility is critical to a normal gait pattern; therefore, osteochondral defects (OCDs) of the first metatarsal head should be treated promptly to avoid functional limitation and progression to hallux rigidus. <15 cases of OCDs of the first MTP joint in the pediatric population, predominantly adolescents, have been published so far. The purpose of this article is to present a rare case of an adolescent first MTP joint OCD treated by the technique of autograft osteochondral mosaicplasty, which has been commonly used for OCDs of the knee and talus but scarcely described for the first MTP joint.
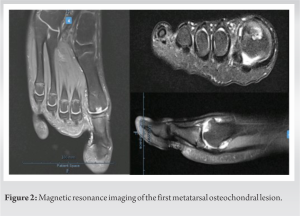
Case Report: The case of a 13-year-old male futsal player with a post-traumatic 50 mm2 OCD of the first metatarsal head is presented. The Osteochondral Autograft Transfer System® (Arthrex Inc™, Naples, FL) was used to harvest a 10-mm diameter donor plug from the medial ipsilateral femoral condyle, then delivered to the first metatarsal head. At the 6-month follow-up, physical activity had been resumed with no pain or significant mobility limitation and an improvement of the American Orthopedic Foot and Ankle Society hallux score of 54–95 points. At the same time, a follow-up magnetic resonance showed complete incorporation of the osteochondral graft without bone edema or subchondral osteonecrosis.
Conclusion: Treatment for osteochondral lesions, regardless of their location, aims to restore function by recreating the articular congruity reducing the potential for a progressive degenerative process. Multiple surgical treatment options exist for OCDs of the first metatarsal head. The treatment decision must take into consideration both patient factors and lesion factors. Based on this, a literature revision and treatment decision rationale are presented. This case demonstrated that an osteochondral transplant could be a reasonable treatment option for a traumatic, full-thickness OCD of the first metatarsal head in adolescent patients.
Keywords: Adolescent, first metatarsal head osteochondral defect, autograft osteochondral mosaicplasty.
Isolated osteochondral defects (OCDs) are caused by damage to the articular cartilage and can be a major source of pain, joint stiffness, osteoarthritis, and functional limitation [1, 2]. Although the insult that activates the degenerative process may be quite variable in nature, trauma has been well recognized as a precipitating factor [1, 2, 3, 4]. The consequence to the articular surface, following a traumatic insult, can be variable in severity. A repetitive low-energy trauma may result in fibrillation or a softening of the articular surface, while an acute incident of a greater intensity could lead to a complete transchondral disruption and subchondral necrosis [3, 5]. Osteochondral lesions have already been described in the knee, ankle, wrist, hip, hand, and less frequently on the foot [2, 4]. The first metatarsophalangeal (MTP) joint is affected even more rarely with about 150 cases published so far [1, 2, 3, 4, 6, 7, 8, 9, 10, 11, 12, 13, 16, 17, 18, 19, 20]. First MTP joint mobility is critical to a normal gait pattern and action of the windlass mechanism that assists in balance, impact reduction, and normal stance [4] Therefore, OCDs of the first metatarsal head should be treated promptly to avoid functional limitation and progression to hallux rigidus. Treatment options classically range from conservative measures to marrow-inducing reparative procedures including subchondral drilling, curettage, microabrasion, and microfracture, both open and arthroscopically [4, 8, 9, 11, 14]. More recently alternative techniques such as osteochondral grafting, mosaicplasty, and frozen osteochondral allografts have been developed to transfer articular hyaline cartilage to replace the injured area [1, 2, 4, 5, 7, 12, 13, 15]. In 2019, Richter et al. published the mid-term results of matrix-associated stem cell transplantation in a series of 81 chondral defects of the first MTP joint [6]. More recently, Bartlett [11] described the arthroscopic debridement for the treatment of an osteochondritis dissecans of the first MTP in a pediatric patient. However, no more than 15 cases of OCDs of the first MTP joint in the pediatric population, predominantly adolescents, have been published so far [11, 16, 17, 18, 19, 20]. All things considered, the purpose of this article is to present a rare case of an adolescent first MTP joint OCD and to describe the technique of autograft osteochondral transplantation, which has been commonly used for OCD of the knee and talus but scarcely described for the first MTP joint [1, 3, 4, 10, 13].
A 13-year-old healthy, male futsal player, presented in our outpatient clinic with a chief complaint of progressive right hallux pain with 5 months duration. These complaints started after a direct axial load to his first MTP joint during a training exercise. Futsal practice was then interrupted and had not been resumed since due to persistent pain. On examination, the first MTP joint dorsiflexion and plantarflexion were 10° each and markedly painful. Axial compression resulted in severe pain. There was no crepitation, warmth, or erythema. Non-inflammatory dorsal volume increase and a noticeably decreased force of contraction of the extensor hallucis longus were noted. Gait examination showed an antalgic pattern on the right side. Plain film radiographs showed a circumscribed area of radiolucency at the articular surface of the first metatarsal head and dorsal osteophyte formation (Fig. 1). Joint space narrowing was not visualized. 
Surgical Technique
A decision to perform an autologous osteochondral graft mosaicplasty was made. The patient was placed in the supine position under balanced anesthesia with a peripheral popliteal nerve block. A thigh tourniquet was used for hemostasis. A 5-cm longitudinal dorsal incision was made overlying the right first MTP joint. A linear capsulotomy was made to expose the first MTP joint. A 9-mm of larger diameter and 5-mm deep OCD was discovered in the first metatarsal head (Fig. 3). 


A functional great toe is important considering its role during gait. In healthy patients, the forces during the push-off phase under the first metatarsal head and hallux account for about 53% of the body weight [4]. Consequently, loss of first MTP joint motion may not be acceptable for active patients who aim to resume recreational and sports activities. Healing of an OCD depends on several factors, including the depth and orientation of the lesion, the orientation of the fracture line, age of the patient, time from injury, the radiographic stage at the time of presentation, and degree of fibrous tissue replacement of bone [3] Kessel, and Bonney [18] reported nine cases of adolescent hallux rigidus in 1958, two of them had radiographic evidence of osteochondritis of the first metatarsal head. Years later, in 1966, Goodfellow [19] presented two cases of adolescent osteochondritis of the first metatarsal head and proposed this lesion as the cause of swelling and spasm of the surrounding soft tissues and, consequently, joint degeneration. If osteochondritis is recognized early, an attempt at conservative therapy with non-weight-bearing, anti-inflammatory medication, sports abstention, and physiotherapy may be considered. However, with high-grade OCD (stage IV, as in our case), the probability of further arthrosis is almost certain and the need for additional surgical intervention is most likely [22]. OCDs have been surgically treated with methods such as drilling, curettage, microabrasion, and microfracture. Thomas and Dwyer [16] published a series of five cases, with ages between 12 and 16 years old. In three cases, the initial operative treatment was defect curettage or drilling with a significant immediate improvement of the symptoms followed, however, by the recurrence of the pain. These techniques result in a fibrocartilage-filled defect characterized by inferior resistance to compression, cyclic loading, and shearing when compared to hyaline cartilage [10]. Smaller defects <15 mm in diameter and more superficial defects may respond well to excision of the osteochondral fragment, curettage, and subchondral drilling procedures. However, larger lesions (>15 mm), especially lesions with extensive subchondral defects, may not respond to these techniques and the articular surface may continue to deteriorate. Alternative techniques such as osteochondral grafting, mosaicplasty, and frozen osteochondral allografts have been developed to transfer articular hyaline cartilage to replace the injured area [10]. Furthermore, we must bear in mind that the metatarsal head is relatively small in comparison with the talus or distal femur, and therefore, a proportional smaller defect size cutoff point must be considered. Kim et al. [4] published a clinical comparison between the osteochondral autograft system and subchondral drilling in OCD of the first metatarsal head and concluded that OCDs larger than 50 mm2 or the presence of a subchondral cyst were predictors of worse clinical results and further arthritis progression in the subchondral drilling group and, therefore, recommended OATS as the treatment of choice rather than subchondral drilling for the treatment of OCD of the first metatarsal head [4]. Our patient presented with a significant progressive limitation of the range of motion of his first MTP joint due to a 5-month evolution grade IV lesion with 50 mm2 and almost 10 mm of greater axis which represented about one-third of the first metatarsal head articular surface; therefore, a decision for surgical treatment with autograft mosaicplasty was made. Autograft-type procedures have been described with excellent results. Such a technique was originally done to address OCDs on the weight-bearing surface of femoral condyles but have become a viable treatment option for similar defects in other joints [12]. Second-look arthroscopies have demonstrated normal and congruent appearing articular surfaces at follow-up [3, 23]. Furthermore, the use of autografts eliminates the question of graft acceptance which can be a disadvantage of allografts, along with limited chondrocyte viability and extended recovery time [3, 24]. Recently, Hollawell et al. [12] published the results of 13 patients with first metatarsal head OCDs treated with fresh first metatarsal head osteochondral allograft and despite having reported an overall improvement in pre-operative symptoms and patient satisfaction, the technique was not recommended for patients with a desire to return to a higher activity level, including running, or activities that created a greater load on the first MTP joint. Van Dyke et al. [7] reviewed the results of nine patients who underwent particulated juvenile cartilage allograft implantation for first metatarsal head OCDs, the large majority sized <50 mm2 (average 44.6 mm2). Despite the good results presented, the cost of these grafts is very high, and autograft remains the gold standard, especially for larger-size defects. Nevertheless, some concerns about the autograft technique include donor site morbidity and the limited availability of donor sites [3]. Furthermore, identification of a donor site that will match the exact topography of such a specific recipient lesion can be difficult. In their research, Kim et al. [4] described the results of ten cases treated with femoral condyle plug autograft transplantation with a significant improvement in the mean AOFAS score and activity levels with no report on donor site morbidity. This represented the largest series of first metatarsal head OCDs treated with osteochondral autograft. In three cases, an uneven radiographic appearance of the subchondral bone was found caused by thicker articular cartilage present in the distal femur when harvesting the donor graft from the distal femur. After using the same harvesting technique in one case, Kravitz [10] evaluated this subchondral bone mismatch with follow-up MRI and reported no obvious joint incongruities in the sagittal view, despite the radiographic findings. This author postulated that alternative options for acquiring osteochondral grafts for first metatarsal osteochondral transfer may include an autogenous transplant from the talus since the thickness of articular cartilage is presumably closer to that of a first metatarsal head. Nonetheless, so far only one case of talus plug autograft transfer to the first metatarsal head has been published by Zelent and Neese [3]. The authors believe that this non-articular talar surface donor site is better geometrically matched to the articulating portion of the metatarsal head and that it eliminates the need for additional consultation and preparation required to obtain a graft from a distant articular surface. Still, more studies are needed to predict the success of this technique. More recently, Saxena and Shou [1] described a technique that combined subchondral drilling with autograft transfer from the dorsal metatarsal exostosis priorly removed, which proved sometimes non-viable, insufficient, or in need of additional fixation with bioabsorbable pins for larger lesions. In our case, based not only on the lesion characteristics but also on literature and surgeon experience, the donor site decision was made in favor of the femoral condyle through a mini-arthrotomy with no report on donor site morbidity or subchondral radiographic or MRI mismatch on follow-up.
Multiple surgical treatment options exist for OCDs of the first metatarsal head. The goal is to restore function by recreating the articular congruity reducing the potential for a progressive degenerative process. The treatment decision must take into consideration both patient factors (age, skeletal maturity stage, physical activity level/sports modality, and clinical presentation) and lesion factors (size, location, stability, and subchondral extension). This case demonstrated that an osteochondral transplant could be a reasonable treatment option for a traumatic, full-thickness OCD of the first metatarsal head also in adolescent patients. Further, evaluation of a large case series is needed to determine the long-term efficacy of this procedure.
In the pediatric population, <15 cases of MTP joint OCDs have been published with surgical treatment options ranging from realignment osteotomies to marrow-inducing reparative procedures. This case proves that an alternative technique such as osteochondral autografting is a reasonable treatment option for a traumatic, full-thickness defect of the first metatarsal head also in adolescent patients.
References
- 1.Saxena A, Shou L. A novel technique to treat hallux rigidus in athletic patients with central osteochondral defects: Preliminary report on 12 cases. J Foot Ankle Surg 2021;60:845-9. [Google Scholar]
- 2.Bruno MA, Marcos RF, Wagner FV, Wagner FV. Treatment of osteochondral lesion of the first metatarsal head: Osteochondral graft transplantation combined with moberg osteotomy: Case report. Foot Ankle Spec 2021;14:515-20. [Google Scholar]
- 3.Zelent ME, Neese DJ. Osteochondral autograft transfer of the first metatarsal head: A case report. J Foot Ankle Surg 2005;44:406-11. [Google Scholar]
- 4.Kim YS, Park EH, Lee HJ, Koh YG, Lee JW. Clinical comparison of the osteochondral autograft transfer system and subchondral drilling in osteochondral defects of the first metatarsal head. Am J Sports Med 2012;40:1824-33. [Google Scholar]
- 5.Goecker RM. Osteochondral Allograft of First Metatarsal Head Lesions. The Podiatry Institute Manual. 2012 Update. United States: The Podiatry Institute; 2012. p. 115-9. [Google Scholar]
- 6.Richter M, Zech S, Meissner SA, Naef I. Mid-term (4-7 years) results of matrix-associated stem cell transplantation (MAST) in chondral defects of the first metatarsophalangeal joint. Food Ankle 2019;17:11-20. [Google Scholar]
- 7.Van Dyke B, Berlet GC, Daigre JL, Hyer CF, Philbin TM. First metatarsal head osteochondral defect treatment with particulated juvenile cartilage allograft transplantation: A case series. Foot Ankle Int 2018;39:236-41. [Google Scholar]
- 8.Kuyucu E, Mutlu H, Mutlu S, Gülenç B, Erdil M. Arthroscopic treatment of focal osteochondral lesions of the first metatarsophalangeal joint. J Orthop Surg Res 2017;12:95. [Google Scholar]
- 9.Bojanić I, Smoljanović T, Kubat O. Osteochondritis dissecans of the first metatarsophalangeal joint: Arthroscopy and microfracture technique. J Foot Ankle Surg 2011;50:623-5. [Google Scholar]
- 10.Kravitz AB. Osteochondral autogenous transplantation for an osteochondral defect of the first metatarsal head: A case report. J Foot Ankle Surg 2005;44:152-5. [Google Scholar]
- 11.Bartlett DH. Arthroscopic management of osteochondritis dissecans of the first metatarsal Head. Arthroscopy 1988;4:51-4. [Google Scholar]
- 12.Hollawell S, Moen R, Coleman M, Carson M. Osteochondral fresh allograft transfer to address osteochondral defect of the first metatarsal head in early hallux limitus. J Foot Ankle Surg 2021;60:157-62. [Google Scholar]
- 13.Delniotis I, Leidinger B. A case report of osteochondritis dissecans of the first metatarsophalangeal joint treated with autologous cancellous bone and chondral flap reconstruction. J Surg Case Rep 2020;2020:rjaa026. [Google Scholar]
- 14.Sherman TI, Kern M, Marcel J, Butler A, McGuigan FX. First metatarsophalangeal joint arthroscopy for osteochondral lesions. Arthrosc Tech 2016;5:e513-8. [Google Scholar]
- 15.Giannini S, Buda R, Ruffilli A, Pagliazzi G, Vannini F. Bipolar fresh osteochondral allograft for the treatment of hallux rigidus. Foot Ankle Int 2013;34:908-11. [Google Scholar]
- 16.Thomas AP, Dwyer NS. Osteochondral defects of the first metatarsal head in adolescence: A stage in the development of hallux rigidus. J Pediatr Orthop 2020;9:236-9. [Google Scholar]
- 17.Jack EA. The aetiology of hallux rigidus. Br J Surg 2005;27:492-7. [Google Scholar]
- 18.Kessel L, Bonney G. Hallux rigidus in the adolescent. J Bone Joint Surg Br 1958;40:668-73. [Google Scholar]
- 19.Goodfellow J. Aetiology of hallux rigidus. Proc R Soc Med 1966;59:821-4. [Google Scholar]
- 20.McMaster M. The pathogenesis of hallux rigidus. J Bone Joint Surg Br 1978;60:82-7. [Google Scholar]
- 21.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994;15:349-53. [Google Scholar]
- 22.Vancil D, Mozena J. Osteochondritis dissecans and the first metatarsophalangeal joint. J Am Podiatr Med Assoc 1986;76:645-7. [Google Scholar]
- 23.Hayes DW Jr., Averett RK. Articular cartilage transplantation. Current and future limitations and solutions. Clin Podiatr Med Surg 2001;18:161-76. [Google Scholar]
- 24.Lee C, Chao K, Huang G, Wu S. Osteochondral autografts for osteochondritis dissecans of the talus. Foot Ankle Int 2003;24:815-22. [Google Scholar]