Efficient management of hand soft tissue defects in a resource limited field situation.
Dr. Varun Vig, Department of Orthopaedic Surgery, Military Hospital, Bhopal, Madhya Pradesh, India. E-mail: vampire3090@gamail.com
Introduction: Managing soft-tissue defects of hand is a challenging problem for any surgical team, even more in a field hospital setting of a conflict combat zone, where resources are scarce and such cases due to blunt trauma, gunshot wound and deep tissue infections are common.
Case Report: We present four different cases, all middle aged males, who sustained injuries due to crush, low velocity gun shot, and defects post-debridement of acute onset infections following abrasions. The first patient was managed with doubled pedicled abdominal flap, the second patient was managed with external fixation for fracture, and cross finger flap for the defect. The third and fourth patients had similar presentations of acute onset deep soft tissue and bony infection, out of which one was managed with full thickness skin graft from anterior abdominal wall and the other with bi-pedicled abdominal flap. All the patients had good functional outcomes with no functional restrictions at follow-up of 12 weeks.
Conclusion: All the cases were performed in a challenging situation of a highly active combat field zone, with limited resources and lack of availability of a trained hand surgeon. An early soft-tissue coverage, as soon as possible, was crucial in saving the hand function and guaranteeing a speedy return to function in view of lack of a professional hand surgery team and specialized microsurgery equipment.
Keywords: Hand defect, UN field hospital, combat zone.
Field hospitals are typically located in conflict zones and are equipped with facilities that help save lives from life-threatening battlefield injuries. If you ever need a limb reconstruction procedure by a plastic surgeon, the hospital is typically mandated by law to evacuate them to a place where they can be operated on. Managing soft-tissue defects of hand is a challenging problem for any surgical team, irrespective of the setup [1]. When such a case with a large, soft-tissue defect is encountered in a field hospital setting, the task becomes even more arduous. Our surgical team comprised of an Orthopedic Surgeon and a General Surgeon, with limited resources in a conflict combat zone in a field location. In such conflict situations, it becomes difficult to organize for air evacuation of such patients due to administrative challenges. The injuries are usually associated with severe contamination and high degree of soft tissue injury, which makes the management even more challenging. This case series aims to present the management and successful outcomes for cases of soft tissue defects of hand, due to varied causes such s blunt trauma, gunshot wound, and deep tissue infections. These indications demand technically challenging reconstructive surgery procedures, which are extremely difficult to perform in a resource limited environment of a United Nations Field hospital.
Case 1
The patient was a 36-year-old male who injured his right hand and sustained Open dislocation of Distal Inter phalangeal Joint (DIP) of his right middle finger, laceration of the dorsum of right ring finger, and a closed comminuted fracture of the distal phalanx of the right little finger, after receiving an injury while operating an electric generator. The laceration over the ring finger was clean and amenable to lavage and primary closure and the fracture of the little finger warranted splinting. There was significant soft-tissue loss to the dorsal aspect of the middle finger from the head of proximal phalanx till the nail bed with exposed extensor tendon slip and associated contamination by oily material and powdery dirt, rendering it unfit for primary closure (Fig. 1).
Case 2
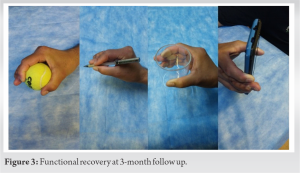
A 29-year-old, UN peacekeeper, sustained a gunshot wound to his dominant hand primarily involving thumb and little finger. He sustained an open, comminuted fracture of his thumb distal phalanx and head of proximal phalanx, with severe crush and stellate shaped irregular wound margin just proximal to the nail plate. The splinter injury also caused full thickness soft-tissue loss on the volar aspect of the little finger overlying the area of middle phalanx. The thumb fracture was managed with external JESS fixator application after through debridement of the wound initially (Fig. 4).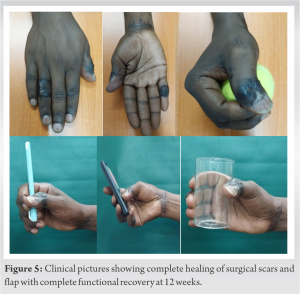
Case 3
A 32-year-old gentleman presented with complaints of severe pain with gross swelling and deformity involving his little finger of the right hand. The symptoms had stared 7 days back when individual sustained an abrasion wound over the dorsal aspect of little finger following a fall from a two wheeler and had rapidly progressed over next few days to have circumferential involvement of the finger with moderate grade fever. On gross examination, the digit was swollen, shiny, tender to touch with minimal, or no movements at IP joints, along with skin defect and purulent discharge from volar aspect of the finger. Based on the initial laboratory and radiological workup, a presumptive diagnosis of finger abscess with underlying osteomyelitis was made and patient was taken up for radical debridement. After debridement, the raw wound created over the little finger was amenable for coverage by a full thickness skin graft. The graft was harvested from skin over the anterior abdominal wall. In addition, the finger was stabilized at IP joints using a K wire (Fig. 6). Intraoperatively, specimen was sent for laboratory identification of causative organism, and broad spectrum antibiotics were started immediately. The organism was found to be Staph aureus after which culture specific antibiotics were continued for 14 days intravenously, followed by orally for a period of around 6 weeks, along with serial saline wound dressings. The K wire was removed at 6 weeks and range of motion exercise was commenced.
Case 4
Another 35-year-old male individual had similar presentation, with fever, pain, swollen digit, and purulent discharge after a traumatic injury to his right little finger. The case was evaluated on similar lines and identified as finger abscess with acute osteomyelitis. He was also managed similarly with radical debridement. However, after debridement the defect was deep with exposed tendons and bone, hence could not be covered by skin graft alone. Based on the size and depth of defect, it was decided to be covered by Bi-pedicled abdominal flap again (Fig. 7). The division of flap, with respect to both the pedicles was done again in a staged manner, and was completely divided at the end of 4 weeks. After this, the physiotherapy was started at 6 weeks. At 12 weeks follow-up, there was good function of hand with no limitation or restriction of functional activities of daily living.
Soft-tissue defects of hand are usually encountered in situations of traumatic events such as crush injuries, sharp lacerations, infections, post-tumor resections, or burns [2]. Given the variety of movements that many joints enable, soft-tissue defects of hand, especially those to the dominant hand, are likely to result in a severe functional handicap and disfigurement, often with financial repercussions for the victim. The prevalence has increased with the use of sophisticated machines, especially in the dominant hand. In a retrospective review of 58 patients of hand crush injury by Okeke et al. during the end of last century, it was documented that more aggressive management needs to be taken while managing such soft tissue injuries [3]. Adequate management of these defects requires an early diagnosis followed by appropriate surgical care as appropriate which must be followed by appropriate rehabilitation to ensure adequate return of function. Shrestha et al. in their series of 2899 cases of crush injury of hand stressed the importance of early referral to a tertiary care center for management of these injuries [4]. Accurate damage assessment and building a reconstruction strategy by structures are crucial management elements. Injuries of the dorsal surface of the hand are peculiar with exposure of extensor mechanisms of hand and adequate skin cover is essential. Primary surgery requires exact and thorough debridement, skeletal stabilization, vascular repair, and soft-tissue cover if any exposed vessels are present. Procedures to improve the hand’s appearance or functionality should be part of secondary surgery [5]. These include bone grafting, fusion, rebuilding of tendons and nerves, debulking of flaps, and toe-to-hand transfers. The management options for these defects include a wide spectrum from linear closure, primary or delayed partial or full thickness skin grafts to loco regional or free flaps [6]. The main aim of reconstruction of hand defects is to provide a thin, pliable skin that ensures mobility of the fingers involved [7]. The reconstruction strategy usually depends on a lot of variables including exact location and defect size, presence of infection, requirement of staged procedures, esthetics, and availability of resources. Skin grafts are usually poor in volume and they should be reserved only for small defects with healthy subcutaneous tissue underneath [8]. Skin grafts do require healthy vascularized beds for their survival. Moreover, regional flaps based on radial and ulnar artery perforators are not long enough to safely reconstruct these defects. Other options for coverage of large defects of hand include distant flaps like groin or abdominal flap and free flaps like anterolateral thigh flap, medial sural artery perforator flap, dorsalis pedis artery flap, or lateral arm flap [9]. Even though, free tissue transfer is one of the common reconstructive options for the soft-tissue cover in hand, distal pedicled flaps are still considered the lifeboat in a failed free tissue transfer and in lesser experienced surgeon performing the surgery. Sabapathy and Bajantri stressed the importance of a distal flap in reconstruction of hand defects [10]. Random pattern abdominal flap is considered an excellent flap design for finger reconstruction. The anterior abdominal wall is abundantly supplied by the segmental lumbar vessels and provides for an excellent choice for raising flaps. Yu et al. in their series of 23 patients for finger reconstruction using random pattern abdominal flap showed that there is good sensory recovery at the end of 6 months in wound areas up to 2.5 × 3 cm. Moreover, most of the patients were satisfied with their finger appearance, satisfactory flexibility, and texture [11]. In a recent study by Elliot et al., they emphasized that good or sometimes better functional outcomes can be achieved by much simpler procedures as well. They advocated use of simple moist dressings for fingertip defects, which require extra care and patience both on the part of surgeon and the patient. Another method proposed by them is the use of dermal substitutes initially to cover the defect, which allows for regeneration of subcutaneous tissues, followed by a full thickness skin graft. The results of this method are very promising for major defects, with minimal morbidity of donor site and good function, sensation, and cosmesis. However, the major drawback is the cost factor and limitation of resources, in field situation like ours [12]. The use of venous flaps in hand defects is also an attractive option due to their less bulky appearance, no arterial sacrifice, and less deep dissection of donor vessels.
In our series of four patients, two were managed with bi-pedicled abdominal flap, one with cross finger flap and another one with full thickness skin graft. However, all of them were performed in a challenging situation of a highly active combat field zone, with limited resources and lack of availability of a trained hand surgeon. An early intervention was necessary in these patients, without rapid access to facilities for hand surgery due to logistical considerations, to ensure the preservation of hand function.
The use of soft-tissue coverage in the form of a graft or flap, as soon as possible was crucial in saving the hand and guaranteeing a speedy return to function due to the lack of a professional hand surgery team and specialized microsurgery equipment. A detailed knowledge of proper anatomy, correct indications, and various methods of reconstruction of soft-tissue defects is mandatory before attempting any such procedure; however, modifications and innovations should be made in situations of extreme constraints to provide early definitive surgery.
References
- 1.Yannascoli SM, Thibaudeau S, Levin LS. Management of soft tissue defects of the hand. J Hand Surg Am 2015;40:1237-44. [Google Scholar]
- 2.Battiston B, Fulchignoni C. Soft tissue defects of the hand: Etiology and classification. Plast Aesthet Res 2023;10:25. [Google Scholar]
- 3.Okeke LI, Dogo D, Ladipo JK, Ajao OG. Crush injuries of the hand. Afr J Med Med Sci 1993;22:69-72. [Google Scholar]
- 4.Shrestha S, Tamrakar S, Banskota AK. Outline of hand and wrist injuries presenting to an emergency of a tertiary care centre in Nepal. J Nepal Health Res Counc 2019;17:340-4. [Google Scholar]
- 5.Lahiri A. Guidelines for management of crush injuries of the hand. J Clin Orthop Trauma 2020;11:517-22. [Google Scholar]
- 6.Rehim SA, Chung KC. Local flaps of the hand. Hand Clin 2014;30:137-51, v. [Google Scholar]
- 7.De SD, Sebastin SJ. Considerations in flap selection for soft tissue defects of the hand. Clin Plast Surg 2019;46:393-406. [Google Scholar]
- 8.Ray S, Rao K. Full thickness skin grafts. In: Spear M, editor. Skin Grafts. Rijeka: IntechOpen; 2011. [Google Scholar]
- 9.Almobarak BA, Mohamed ME, Hassan MI. Different modalities of soft tissue coverage of hand and wrist defects. Clin Pract 2017;15:466-72. [Google Scholar]
- 10.Sabapathy SR, Bajantri B. Indications, selection, and use of distant pedicled flap for upper limb reconstruction. Hand Clin 2014;30:185-99, vi. [Google Scholar]
- 11.Yu YD, Zhang YZ, Bi WD, Wu T. Functional sensory function recovery of random-pattern abdominal skin flap in the repair of fingertip skin defects. Exp Ther Med 2013;5:830-4. [Google Scholar]
- 12.Elliot D, Adani R, Woo SH, Tang JB. Repair of soft tissue defects in finger, thumb and forearm: Less invasive methods with similar outcomes. J Hand Surg Eur Vol 2018;43:1019-29. [Google Scholar]