To lessen the surgical insult on the growing skeleton of children with early-onset scoliosis, we require considerable research to develop efficient surgical and anesthetic techniques and better implant constructs.
Dr. Ankit Rai, Department of Orthopedics Surgery, PGIMER, Chandigarh, India. E-mail: ankitrai.doctor@gmail.com
Introduction: Growing rod construct is one of the most widely acknowledged treatment modalities for early-onset scoliosis around the world, but it is not without complications. Throughout the course of treatment, numerous planned and inadvertent surgical interventions are required, which increase the complexity of the treatment. We share our experience with case examples along with extensive literature search and review to get an insight and document the complications with growing rod treatment.
Case Report: These cases underwent surgery with dual growing rod for thoracolumbar idiopathic scoliosis in the view of failed conservative treatment and progressive deformity. Superficial infection is in one case and recurrence of deformity was a common finding though correction of deformity and final fusion was achieved in the cases. Breakage of screws, autofusion of the spanned segments, and profuse bony growths over the implants are common finding to get. Fibrosis and scar tissue from the previous surgeries result in difficulty in the exposure and performing corrective osteotomy.
Conclusion: Growing rod surgery has high complication rates. Repeated surgical and anesthesia exposure pose a great risk to the body and immature skeleton of the young patient. Previous studies have put forth many possible course of action to lower down the complication rates but have met with variable results. A better implant design and surgical efficacy are needed to cut down the number of complications and surgical interventions in growing rod surgeries.
Keywords: Early-onset scoliosis, dual growing rod, growth sparing surgery.
Regardless of the cause, early-onset scoliosis is first identified in children under the age of 10 and is associated with severe morbidity and mortality if overlooked [1]. By the age of 10, the thoracic cage has significantly grown, and the cardiovascular system has significantly developed. The early-onset scoliosis results in stunted growth of the dorsal spine and thoracic cage that culminates into downswing of the cardiopulmonary function [2]. In this age group, spinal fusion corrects the deformity but at the expense of compromising thoracic height. This increases the complexity of managing early-onset scoliosis. Growth sparing single rod surgery was first described by Harington and then modified by Moe et al. [3, 4]. Akbarnia et al. recommended use of growing dual rods with proximal and distal anchorage. This procedure avoided the spinal fusion to allow growth of thoracic spine and cage with satisfactory curve correction. The growing rod surgery has met with lot of success but not without complications. Previous studies have reported the complication rate in growing rod surgery ranging from 20% to 48% and that too rising with each surgical intervention given to the patient. Wound-related complications, implant failure, and loss of alignment increase the number of unplanned surgeries in this subset of patients [5]. The ultimate spinal fusion is considered end of growing rod treatment, but recent studies have found that it is not imperative in all cases and associated with increased morbidity [6]. We are reviewing our experience at tertiary care center in such cases.
Case 1
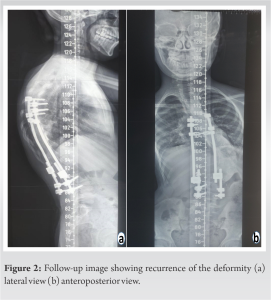
A 4-year-old boy presented with infantile idiopathic scoliosis with right-sided thoracolumbar curve. There were no other associated sign or symptoms. There was no sensory or motor deficit. Standing upright and bending radiographs were done to calculate curve magnitude which was 50°. There was no structural deformity in the spine. Surgical intervention was planned in view of high Cobb angle and progressive deformity. The patient received his index surgery in the form of dual growing rods with deformity correction. Four proximal and distal anchorages were connected with two separate rods to accommodate spinal growth. Post-operative period was uneventful and the patient was mobilized with brace. The patient received four planned surgical procedures during the ensuing period of follow-ups for rod lengthening to accommodate thoracic and lumbar spine growth. At the final follow-up, it was observed that growing rod has hampered the spinal growth and curve progression was also noted. Implant removal was planned. During the surgery, we discerned significant bone formation over the implant and autofusion of some spinal segments (Fig. 1). There were also broken screws which were not radiologically evident. These unforeseen complications lengthened the surgery time and blood loss during the surgery. The patient was advised thoraco-lumbo-sacral orthosis post-operatively and explained for need of spinal fusion surgery, when needed.
Case 2
A 7-years-old female presented with thoracolumbar scoliosis with progressive deformity. The patient was having back pain at presentation. On detailed clinical examination, nothing was found stipulating syndromic or neuromuscular nature of the scoliosis. Neurological examination was unremarkable. Radiological investigations were carried out, which included standing upright and lateral bending radiographs and MRI. A thoracolumbar scoliotic curve of 64° was noted. It was a structural deformity. The surgery with dual growing rods was planned with four proximal and four distal anchorages connected with rods. Proximal and distal anchors were then connected with two separate rods for lengthening. Total five lengthening procedures were performed. The patient acquired chest infection, which lengthened her hospital stay during her hospital admission for lengthening the growing rod for the second time. She developed superficial infection too which was treated with antibiotics. Over the course of treatment, we noted recurrence of the deformity (Fig. 2), which was corrected at the time of final fusion surgery with corrective osteotomy. The patient remained neurologically intact during entire course of treatment. The final fusion surgery was complicated by the extensive scarring, ossification around instrumentation, and autofusion of the segments.
The growing rod surgery is having high complication rates of around 50% and it increases with each surgical procedure (Table 1). 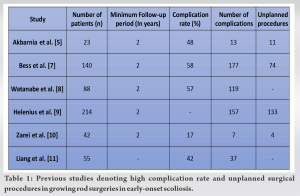
Growing rod surgeries have revolutionized the treatment of early-onset scoliosis but not without its implications and complications. Most of the complications are implant related and that too from proximal anchorage failure. Infections, wound scarring, malalignment, and autofusion further affect the course and outcome of fusion surgery. High complication rate, multiple planned and unplanned surgical procedures, and repeated exposure to anesthetic agents during anesthesia have their adverse effects on the young patients and their immature skeleton. We as authors feel that further research for better implants and surgical efficiency is the need of hour to cut down the number of uncalled surgical procedures and complication rate.
Growing rod surgery despite being widely used worldwide is associated with high complication rates. We need more efficient surgical techniques and implants for lowering number of surgical procedures along with complication rate.
References
- 1.Williams BA, Matsumoto H, McCalla DJ, Akbarnia BA, Blakemore LC, Betz RR, et al. Development and initial validation of the classification of early-onset scoliosis (C-EOS). J Bone Joint Surg Am 2014;96:1359-67. [Google Scholar]
- 2.Canavese F, Dimeglio A. Normal and abnormal spine and thoracic cage development. World J Orthop 2013;4:167-74. [Google Scholar]
- 3.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am 1962;44-A:591-610. [Google Scholar]
- 4.Moe JH, Kharrat K, Winter RB, Cummine JL. Harrington instrumentation without fusion plus external orthotic support for the treatment of difficult curvature problems in young children. Clin Orthop Relat Res 1984;185:35-45. [Google Scholar]
- 5.Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA. Dual growing rod technique for the treatment of progressive early-onset scoliosis: A multicenter study. Spine (Phila Pa 1976) 2005;30:S46-57. [Google Scholar]
- 6.Jain A, Sponseller PD, Flynn JM, Shah SA, Thompson GH, Emans JB, et al. Avoidance of "Final" surgical fusion after growing-rod treatment for early-onset scoliosis. J Bone Joint Surg Am 2016;98:1073-8. [Google Scholar]
- 7.Bess S, Akbarnia BA, Thompson GH, Sponseller PD, Shah SA, El Sebaie H, et al. Complications of growing-rod treatment for early-onset scoliosis: Analysis of one hundred and forty patients. J Bone Joint Surg Am 2010;92:2533-43. [Google Scholar]
- 8.Watanabe K, Uno K, Suzuki T, Kawakami N, Tsuji T, Yanagida H, et al. Risk factors for complications associated with growing-rod surgery for early-onset scoliosis. Spine (Phila Pa 1976) 2013;38:E464-8. [Google Scholar]
- 9.Helenius IJ, Oksanen HM, McClung A, Pawelek JB, Yazici M, Sponseller PD, et al. Outcomes of growing rod surgery for severe compared with moderate early-onset scoliosis: A matched comparative study. Bone Joint J 2018;100-B:772-9. [Google Scholar]
- 10.Zarei M, Tavakoli M, Ghadimi E, Moharrami A, Nili A, Vafaei A, et al. Complications of dual growing rod with all-pedicle screw instrumentation in the treatment of early-onset scoliosis. J Orthop Surg Res 2021;16:112. [Google Scholar]
- 11.Liang J, Li S, Xu D, Zhuang Q, Ren Z, Chen X, et al. Risk factors for predicting complications associated with growing rod surgery for early-onset scoliosis. Clin Neurol Neurosurg 2015;136:15-9. [Google Scholar]
- 12.Cahill PJ, Marvil S, Cuddihy L, Schutt C, Idema J, Clements DH, et al. Autofusion in the immature spine treated with growing rods. Spine (Phila Pa 1976) 2010;35:E1199-203. [Google Scholar]
- 13.Kocyigit IA, Olgun ZD, Demirkiran HG, Ayvaz M, Yazici M. Graduation protocol after growing-rod treatment: Removal of implants without new instrumentation is not a realistic approach. J Bone Joint Surg Am 2017;99:1554-64. [Google Scholar]
- 14.Goldstein MJ, Kabirian N, Pawelek JB, Arandi NR, Mundis GM Jr., Yaszay B, et al. Quantifying anesthesia exposure in growing rod treatment for early onset scoliosis. J Pediatr Orthop 2017;37:e563-6. [Google Scholar]