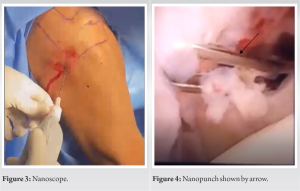
Minimally invasive surgery is always recommended wherever possible. Nanoscope has advantages of being percutaneous and its application can be extended to various pathology corrections.
Dr. Hari Krishna Yadoji, Department of Arthroscopy and Shoulder Surgery, Sunshine Hospital, Secunderabad, Telangana, India. E-mail: drharikrishna20@gmail.com
Introduction: Adhesive capsulitis or frozen shoulder is a painful condition. With advent of newer and newer technology, minimally invasive surgeries are being tried in all kinds of surgeries. Nanoscope is one such invention that lead to the idea of percutaneous arthroscopy. The aim of this case report is to emphasize the role of nanoscope under local anesthesia in treatment of adhesive capsulitis.
Case Report: A 45-year-old male presented with a history of restricted movements in the right shoulder for 1 year. On clinical examination, rotator cuff strength was under normal limits, his forward elevation was 100°, lateral elavation was 90°, external rotation - 45°, abduction external rotation 30°, and abduction internal rotation 40°. X-ray shoulder was normal. MRI shoulder was showing features of adhesive capsulitis.
Conclusion: Percutaneous arthroscopic capsular release with nanoscope under local anesthesia is a safe and cost-effective procedure. With minimal infrastructure, it can be developed into an outpatient procedure. The advantages of this percutaneous technique over conventional arthroscopic release needs further studies.
Keywords: Nanoscope, adhesive capsulitis, capsule release.
Shoulder has multidirectional mobility and is vital for day to day activities. Adhesive capsulitis is a painful condition and affects daily living. Adhesive capsulitis is a specific pathology in which chronic inflammation of the capsule subsynovial layer produces capsular thickening, fibrosis, and adherence of the capsule to itself and to the anatomic neck of the humerus [1]. Despite physiotherapy being the first line of treatment, refractory cases are managed by procedures such as manipulation under anesthesia and arthroscopic capsule release. Manipulation under anesthesia is an easy procedure but there are potential complications such as rotator cuff tear and humerus fracture with it [2]. On the other hand, arthroscopy has the advantage of complete inspection of the joint, confirmation of the diagnosis, and a more precise capsulotomy without the risks of manipulation. When compared to manipulation under anesthesia, arthroscopic capsular division has shown improved pain relief and restoration of function for longer duration [3, 4]. Arthroscopic capsule release is done under general anesthesia or regional nerve block. We used to perform arthroscopic capsule release under regional nerve block due to its benefits over general anesthesia [5]. After the introduction of nanoscope by arthrex, it has been in usage in different procedures [6, 7, 8, 9]. Lavender et al. [7] reported the advantages of nanoscope such as it avoids posterior capsule and rotator cuff injury, fluid extravasation, and single incision labral repair. At our center, we use nanoscope in selected cases like knee meniscal root repair and shoulder labral repair. In this surgical note, we would like to describe an incision less arthroscopic capsular release of adhesive capsulitis under local anesthesia done for the first time in the literature.
A 45-year-old male presented with a history of restricted movements in the right shoulder for 1 year. There was no history of trauma. Patient was a known case of Type 2 diabetes mellitus for 5 years and is on regular medication. On clinical examination, rotator cuff strength was under normal limits, his forward elevation was 100°, lateral elavation was 90°, external rotation – 45°, abduction external rotation 30°, and abduction internal rotation 40°. X-ray shoulder was normal as in Fig. 1. MRI shoulder was showing features of adhesive capsulitis. There was a history of intra-articular steroid therapy along with physiotherapy 6 months ago. (The patient was suffering with pain since more than a year not 6 months. 
Surgical Technique
Position: Beach chair as in Fig. 2.
Anesthesia: Skin infiltration with 2% xylocaine and joint infiltration with 0.5% xylocard. Arthroscopy: Bony landmarks of spine of scapula, acromion, clavicle, and coracoid were marked with a marker. Posterior skin infiltration was done around the posterolateral corner. After confirming the effect of local anesthesia, 17-gauge spinal needle was introduced into the joint, at a point 2 cm inferior and 1–2 cm medial from the acromion posterolateral corner. After confirming Intra-articular placement of the needle by injecting normal saline, joint was infiltrated with 10 mL of 0.5% xylocard and waited for 5 min for its action on capsule. A nitinol guide wire was passed through the needle. The needle was withdrawn securing the guide wire. 
Arthroscopic capsular release is safe and the relief is for longer duration. Regional nerveblock and general anesthesia have their own demerits of pulmonary and other complications [10]. Designing a procedure that can be done under local anesthesia is very safe for the patient and is also cost effective. In arthroscopic procedure, there is a chance of fluid leakage from the portals made, resulting in usage of larger quantity of fluid. There is also a potential risk of fluid extravasation in the muscle planes leading to increased pain during immediate post-operative period and also the patients may require longer time for pain recovery. On the other hand with the advent of nanoscope and other small instruments that can be inserted percutaneous, fluid leakage can be avoided. Percutaneous technique decreases the risk of fluid extravasation, thus decreasing post-operative pain and aids in a speedy recovery. Use of regional nerve block or general anesthesia demands 4–6 h or in some cases a 24 h stay in the hospital. With our technique done under local anesthesia, at present, we are discharging the patient within 2 h, this duration can be further shortened. Nevertheless, there are disadvantages with this technique. An extensive release of capsule is not possible in this technique. Patient selection is vital. The aim of our surgical technique is to emphasise on the possibility of making capsular release as an outpatient walk-in procedure and make it available for wider sections of people.
Percutaneous arthroscopic capsular release with nanoscope under local anesthesia is a safe and cost-effective procedure. With minimal infrastructure, it can be developed into an outpatient procedure. The advantages of this percutaneous technique over conventional arthroscopic release need further studies.
Percutaneous nanoscope capsule release is a cost-effective procedure in treating refractory cases of adhesive capsulitis.
References
- 1.Neviaser JS. Adhesive capsulitis of the shoulder. J Bone Joint Surg Am 1945;27:211-22. [Google Scholar]
- 2.Loew M, Heichel TO, Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg 2005;14:16-21. [Google Scholar]
- 3.Ogilvie-Harris DJ, Biggs DJ, Fitsialos DP, MacKay M. The resistant frozen shoulder. Manipulation versus arthroscopic release. Clin Orthop Relat Res 1995;319:238-48. [Google Scholar]
- 4.Ide J, Takagi K. Early and long-term results of arthroscopic treatment for shoulder stiffness. J Shoulder Elbow Surg 2004;13:174-9. [Google Scholar]
- 5.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomised trials. BMJ 2000;321:1493. [Google Scholar]
- 6.Lavender C, Lycans D, Adil SA, Berdis G. Single-incision rotator cuff repair with a needle arthroscope. Arthrosc Tech 2020;9:e419-23. [Google Scholar]
- 7.Lavender C, Lycans D, Kopiec A, Sayan A. Nanoscopic single-incision anterior labrum repair. Arthrosc Tech 2020;9:e297-301. [Google Scholar]
- 8.Munaretto N, Hinchcliff K, Dutton L, Kakar S. Is wrist arthroscopy safer with the nanoscope? J Wrist Surg 2022;11:450-5. [Google Scholar]
- 9.Senna LF, Lavender C. Nanoscopic distal clavicle resection. Arthrosc Tech 2022;11:e551-4. [Google Scholar]
- 10.Hausman MS Jr., Jewell ES, Engoren M. Regional versus general anesthesia in surgical patients with chronic obstructive pulmonary disease: Does avoiding general anesthesia reduce the risk of postoperative complications? Anesth Analg 2015;120:1405-12. [Google Scholar]