Regional migratory osteoporosis is an unusual condition that affects the weight-bearing joints of the lower extremities. Most cases spontaneously resolve with conservative management.
Dr. Sidra Moiyad, Department of Orthopaedics, Toowoomba Hospital, School of Medicine, Rural Clinical School, University of Queensland, Australia. E-mail: sidra.moiyad@health.qld.gov.au
Introduction: Regional migratory osteoporosis (RMO) is an unusual phenomenon characterized by migrating arthralgia of the lower limbs due to underlying bone marrow edema.
Case Report: We discuss a 57-year-old male with a 3-month history of atraumatic medial knee pain. Magnetic resonance imaging demonstrated bone marrow edema of the medial femoral condyle that resolved with rest and simple analgesia, followed by posterolateral knee pain and similar imaging changes in the lateral femoral condyle.
Conclusion: Most cases of RMO spontaneously resolve with limitation of weight-bearing and simple analgesia. For recurrent cases, surgical intervention may be required.
Key words: Regional migratory osteoporosis, transient osteoporosis, transient bone marrow edema, knee pain, magnetic resonance imaging.
First described in 1967 as osteolysis of the lower extremities [1], regional migratory osteoporosis (RMO) typically presents as migratory arthralgia in weight-bearing joints and is diagnosed with magnetic resonance imaging (MRI) [2]. RMO commonly presents in the fourth and fifth decades, has a male predominance, and is associated with low dietary calcium intake and smoking [3]. The classic yet non-specific transitory MRI signaling pattern is decreased T1 and increased T2 signal of the affected region. RMO resembles bone marrow edema, a phenomenon also noted in various rheumatological disorders, traumatized bone, and other inflammatory conditions [4]. We present the case of a 57-year-old man with RMO. The purpose of this article is to report a relatively rare entity with unclear pathogenesis and summarise the condition’s etiology, underlying radiological findings, postulated pathological correlations, and available treatment strategies.
A 57-year-old farmer presented with a 3-month history of right-sided medial knee pain. The pain had an insidious onset with no history of trauma and gradually worsened to the point that it was interfering with his activities of daily living. The patient had a past medical history of hypertension, obstructive sleep apnea, and lumbar spinal stenosis and was a heavy drinker and smoker. He had previously sustained shoulder and spinal injuries in a motor vehicle accident but described no previous trauma to his lower limbs. 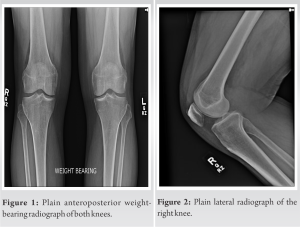
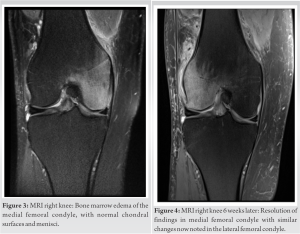
Bone marrow edema is a non-specific MRI finding that may be noted in the setting of rheumatological disorders and trauma. It is characterized by interstitial fluid with accompanying fibrosis in the trabecular structure of subchondral bone, presenting as high signal intensity on T2 and low signal intensity on T1-weighted images [5]. These findings are noted to be self-limiting in some disorders and are then described as transient bone marrow edema (TBMO). TBMO is seen in conditions such as transient osteoporosis of the hip and RMO, terms that are often used interchangeably throughout the literature [2]. On occasions, TBMO is associated with subchondral insufficiency fractures with recent hypotheses suggesting prolonged subchondral insufficiency fractures can trigger TBMO [6] with osteoporosis causing the former or a sub-sequence of the latter [2, 7]. RMO is a distinctive form of TBMO, characterized by the migratory nature of the radiographic changes with clinically correlating symptoms. While systemic osteoporosis is common in patients with RMO, a causal link has not been proven [8, 9]. Other risk factors include sudden limb overuse and a prior episode of transient osteoporosis [9, 10]. The proposed pathology involves the accumulation of toxic stimuli secondary to microdamage to the bone, which increases cellular turnover and activates regenerative foci resulting in rapid bone healing and therefore transient osteoporosis [10]. This so-called regional acceleratory phenomenon [11] has been demonstrated on biopsies obtained from patients with TBME [7]. It is important to note that while systemic osteoporosis predisposes bone to microdamage, even in its absence, weight-bearing joints of the lower extremities are already predisposed to fatigue failure and microdamage secondary to weight-bearing mechanisms; thus, all conditions that result in bone microdamage can potentially cause TBMO [7, 9]. RMO typically affects the weight-bearing joints of the lower extremities, with the hip more commonly affected than the knee. Very few cases involving the ankle and foot have been reported. In RMO affecting the lower limb, 59% of cases involve the proximal femur, 36 % involve the knee, and 4.5% involve the ankle [10]. The MFC is more commonly affected than the LFC due to the biomechanics of the knee [12], and its relatively limited vascular supply; a single vessel supplying the subchondral bone with an apparent watershed area [7]. Rare cases of intra-articular and contralateral migration are reported in the literature [7]. The shifting of weight distribution to avoid pain may increase the load on unaffected joint surfaces, which could potentially be a cause of intra-articular and contralateral migration [10]. Previously, it had been conjectured that TBMO may be an early reversible phase of avascular necrosis (AVN). However, a histological examination of TBMO would suggest that this is not the case. TBMO is characterized by areas of rapid bone turnover, with no evidence of osteonecrosis [7, 13]. It should also be noted that common risk factors for AVN including steroid use, renal disease, and chemotherapy, have not been reported in RMO to date [2]. Various treatment strategies have been employed in the management of RMO [2], ranging from conservative management with simple analgesia, treatment with bisphosphonates for underlying osteoporosis, to surgical decompression to alleviate elevated intramedullary pressures [7], and extracorporeal shockwave therapy to trigger osteoblastic regeneration within the bone [14]. Simple analgesia and avoidance of weight-bearing seem to be the most efficacious treatment [2, 9]. While bisphosphonate therapy has been reported as efficacious in initial presentations, the role of ongoing therapy for the prevention of RMO is unclear [2, 15]. For recurrent cases, core decompression has been shown to be effective, with complete symptomatic and radiological resolution after 5 years [7].
RMO is an uncommon condition that affects the weight-bearing joints of the lower extremities. RMO presents initially as focal arthralgia with radiological evidence of bone marrow edema, followed by migration to other weight-bearing joints or other areas within the affected joint. Although various treatment strategies have been employed, simple analgesia and avoidance of weight-bearing are the most effective. The majority of cases resolve spontaneously with conservative treatment.
- RMO should be considered in the differential diagnosis for patients with chronic joint pain
- MRI is a useful diagnostic tool
- Conservative management with simple analgesia and restricted weight-bearing is successful for most patients
- Surgical intervention may be required for recurrent or refractory cases.
References
- 1.Duncan H, Frame BO, Frost HM, Arnstein AR. Migratory osteolysis of the lower extremities. Ann Int Med 1967;66:1165-73. [Google Scholar]
- 2.Cahir JG, Toms AP. Regional migratory osteoporosis. Eur J Radiol 2008;67:2-10. [Google Scholar]
- 3.Trevisan C, Ortolani S, Monteleone M, Marinoni EC. Regional migratory osteoporosis: A pathogenetic hypothesis based on three cases and a review of the literature. Clin Rheumatol 2002;21:418-25. [Google Scholar]
- 4.Schett G. Bone Marrow Edema. Ann N Y Acad Sci 2009;1154:35-40. [Google Scholar]
- 5.Yamasaki S, Masuhara K, Miki H, Fuji T. Three cases of regional migratory osteoporosis. Arch Orthop Trauma Surg 2003;12:439-41. [Google Scholar]
- 6.Geith T, Stellwag A, Müller PE, Reiser M, Baur-Melnyk A. Is bone marrow edema syndrome a precursor of hip or knee osteonecrosis? Results of 49 patients and review of the literature. Diagn Interv Radiol 2020;26:355-62. [Google Scholar]
- 7.Berger CE, Kröner AH, Kristen K, Grabmeier GF, Kluger R, Minai-Pour MB, et al. Transient bone marrow edema syndrome of the knee: Clinical and magnetic resonance imaging results at 5 years after core decompression. Arthroscopy 2006;22:866-71. [Google Scholar]
- 8.Alsaed O, Hammoudeh M. Recurrent migratory transient bone marrow edema of the knees associated with low vitamin D and systemic low bone mineral density: A case report and literature review. Case Rep Rheumatol 2018;2018:7657982. [Google Scholar]
- 9.Kotwal A, Hurtado MD, Sfeir JG, Wermers RA. Transient osteoporosis: Clinical spectrum in adults and associated risk factors. Endocr Pract 2019;25:648-56. [Google Scholar]
- 10.Karantanas AH, Nikolakopoulos I, Korompilias AV, Apostolaki E, Skoulikaris N, Eracleous E. Regional migratory osteoporosis in the knee: MRI findings in 22 patients and review of the literature. Eur J Radiol 2008;67:34-41. [Google Scholar]
- 11.Frost HM. Perspectives: Bone’s mechanical usage windows. Bone Miner 1992;19:257-71. [Google Scholar]
- 12.Plett S, Hackney L, Heilmeier U, Nardo L, Yu A, Zhang C, et al. Femoral condyle insufficiency fractures: Associated clinical and morphological findings and impact on outcome. Skeletal Radiol 2015;44:1785-94. [Google Scholar]
- 13.Geith T, Niethammer T, Milz S, Dietrich O, Reiser M, Baur-Melnyk A. Transient bone marrow edema syndrome versus osteonecrosis: Perfusion patterns at dynamic contrast-enhanced mr imaging with high temporal resolution can allow differentiation. Radiology 2017;283:478-85. [Google Scholar]
- 14.Vitali MM, Rodriguez NM, Pedretti AM, Drossinos AB, Pironti P, Di Carlo GM, et al. Bone marrow edema syndrome of the medial femoral condyle treated with extracorporeal shock wave therapy: A clinical and MRI retrospective comparative study. Arch Phy Med Rehabil 2018;99:873-9. [Google Scholar]
- 15.Patel S. Primary bone marrow oedema syndromes. Rheumatology (Oxford) 2013;53:785-92. [Google Scholar]







