Palsy of the common peroneal nerve following total knee arthroplasty can be managed conservatively if it presents without any obvious cause, and such cases may even take over 6 months for complete recovery, hence warranting patience.
Dr. Amyn M Rajani, Consultant Orthopedic Surgeon, OAKS Clinic, Gamdevi, Mumbai, Maharashtra, India. E-mail: dramrajani@gmail.com
Introduction: Common peroneal nerve palsy (CPNP) is a rare complication post total knee arthroplasty (TKA). Even though it is diagnosed acutely, the recovery potential is just over 50%. The average period for complete recovery in such cases is 5 months; however, the management remains controversial. Through this report, we present one such case of complete CPNP after bilateral TKA who was conserved with various modalities. Even though the recovery was delayed, the patient made full recovery.
Case Report: A 70-year-old female patient was diagnosed to have bilateral tricompartmental knee osteoarthritis with varus deformity, both clinically and radiologically (Kellgren–Lawrence grade 4). She underwent bilateral TKA in a single sitting as per the standard protocols practiced by the primary author. On post-operative day 1, she had left-sided foot drop with a complete sensory deficit. The patient underwent routine rehabilitation with an ankle foot orthosis splint in the immediate post-operative period, with simultaneous faradic current stimulation for the left lower limb. Periodic electromyography and nerve conduction study was done at the end of 4-week and 3-month post-TKA. At 6.5-month post-surgery, she made a full clinical recovery.
Conclusion: The surgical maneuvers and full neurovascular examination before and after every TKA surgery should be carefully performed. Despite this, if a patient presents with CPNP, the surgeon need not take an aggressive approach, unlike fracture fixation cases. These patients can be managed conservatively using appropriate orthosis, physical therapy, and faradic current stimulation. Through this case, we attempt to report that CPNP patient can recover even after 6 months of surgery when there is no tangible cause for the palsy.
Keywords: Common peroneal nerve palsy, total knee arthroplasty, EMG, NCV, faradic stimulator.
Common peroneal nerve palsy (CPNP) is an uncommon complication post total knee arthroplasty (TKA). The reported incidence of CPNP ranges from 0.01% to 4.3% after a primary TKA [1, 2, 3, 4, 5]. Most of these patients are diagnosed within 48 h of surgery [3, 4, 5]. The potential for complete recovery in such cases ranges from 9.1% to 68% [5, 6, 7]. Despite the rare incidence of CPNP, there could be an alarming rise in its incidence proportionately to the rising numbers of TKAs (primary/revision) [8]. Individuals with CPNP may present with numbness, impaired sensation, tingling over the dorsal surface of the foot, and weakness of the dorsiflexors at the ankle and toes. CPNP can also present with dysesthesia or paresthesia in the dermatomes supplied by the nerve, and nil or diminished motor control of the muscles innervated by the CPN and its branches. CPNP usually manifests at, or shortly after the surgery [6, 7, 9]. Published literature has shown variable rates of recovery in patients diagnosed with CPNP after TKA, ranging from 2% to 100%. The current literature and studies quote that the chances of complete recovery when CPNP is diagnosed after TKA ranges from 9.1% to 68% and if delayed beyond 5 months, surgical intervention is to be considered [5, 6, 7]. This case report not only focuses on the hybrid conservative modality of treatment in such cases but also highlights the fact that these patients can fully recover even after 6.5 months of TKA with dedicated rehabilitation.
A 70-year-old woman consulted for pain in bilateral knee joints, difficulty in climbing stairs, difficulty sitting cross-legged, and difficulty in standing from a sitting position for 6 months. On clinical examination, she had a non-correctible varus deformity in both knees, with medial and lateral joint line tenderness, and positive patellar grind. Her range-of-movement was restricted beyond 115° and she had no flexion deformity of the knee bilaterally. A provisional diagnosis of bilateral tricompartmental knee osteoarthritis was made and the patient was asked to undergo a radiological assessment for confirmation of the diagnosis. Routine X-rays of both knees revealed bone on bone picture medially with significantly reduced lateral joint space and patellofemoral joint space with subchondral sclerosis and marginal osteophytes (Fig. 1).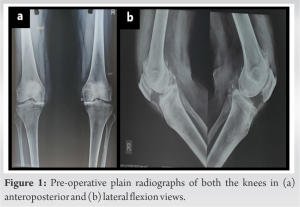
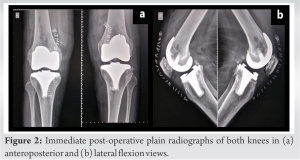

CPNP is a devastating complication of TKA and compromises sensory and/or motor functions of the CPN or its branches, including dysesthesia or paresthesia in the L4, L5, S1, and S2 dermatomes, or decreased motor supply to the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and the peronei. Patients lose the ability to dorsiflex and evert the foot [12]. This was evident in our patient from the EMG and NCV studies of the left foot, which showed left common peroneal sensorimotor neuropathy. The CPN makes its way into the popliteal fossa from the apex and bifurcates, with its fibular branch winding lateral to the fibular head. The nerve lies superficially at the level of the fibular head and is therefore susceptible to blunt force trauma or acute external/internal compression at this level. The possible causes of CPNP, as reported in the literature are compressive dressings, hematoma, direct trauma while cutting the tibial surface, or release of the knee joint capsule, or traction injury during operation by Hohmann retractor [9, 13]. Prolonged tourniquet time, preoperative valgus deformity, and flexion contracture at the knee are the other predisposing factors responsible for CPNP after TKA [14]. These factors are found to be irrelevant in several studies. However, most of these causes were ruled out in our case due to minimal tibial cuts, post-operative compressive dressing being snugly applied, placement of Hohmann retractors under vision, carefully maneuvering the leg under anesthesia, not using the tourniquet, no preoperative valgus or flexion contracture, no signs of hematoma postoperatively. In addition, we neither kept the knees in rectus nor overcorrected it to produce a valgus but under-corrected the varus keeping in mind the kinematic alignment of the knee [10]. We hypothesized the causes of CPNP in this case to be double crush injury due to pre-existing central neuropathy, or traction injury secondary to abnormal anatomy of the nerve route. The use of AFO for foot drop was done as has been established in literature. Faradic current is a direct current that is applied at a frequency of 50:100 Hz with a pulse duration of 0.1–1 ms without any interruption. This facilitates the contraction and relaxation of innervated muscles through the innervated motor fibers, thereby rescuing residual nerve function and preventing muscle wasting. We used this principle for conservative management in our patients. EMG NCV was done at 4 weeks and 3 months, as is protocol in literature [4]. However, unlike a few suggestions by various authors such as Rose et al. [2], and Webster and Murray [7], the primary author decided to prolong the conservative management beyond 5 months and delayed surgical intervention [15]. The patient made a complete clinical recovery at 6.5-month postoperatively and had an excellent knee society score at 18-month follow-up in both knees.
Surgical techniques and maneuvers in TKA should be performed with caution and comprehensive neurovascular examination should be done before and after the, especially in high-risk patients with previous neuropathy (central or peripheral), preoperative flexion deformity of the knee, rheumatoid arthritis, or valgus deformity. Patients presenting with CPNP post-TKA, without any tangible cause for the same, can be managed conservatively with an AFO splint and faradic current stimulation, coupled with periodic clinical and investigative screening for recovery which can take as long as 6.5 months.
CPNP after TKA can be managed conservatively if it presents without any obvious cause, and such cases may even take over 6 months for complete recovery, hence warranting patience.
References
- 1.Idusuyi OB, Morrey BF. Peroneal nerve palsy after total knee arthroplasty. Assessment of predisposing and prognostic factors. J Bone Joint Surg Am 1996;78:177-84. [Google Scholar]
- 2.Rose HA, Hood RW, Otis JC, Ranawat CS, Insall JN. Peroneal-nerve palsy following total knee arthroplasty. A review of The Hospital for Special Surgery experience. J Bone Joint Surg Am 1982;64:347-51. [Google Scholar]
- 3.Asp JP, Rand JA. Peroneal nerve palsy after total knee arthroplasty. Clin Orthop Relat Res 1990;261:233-7. [Google Scholar]
- 4.Nercessian OA, Ugwonali OF, Park S. Peroneal nerve palsy after total knee arthroplasty. J Arthroplasty 2005;20:1068-73. [Google Scholar]
- 5.Schinsky MF, Macaulay W, Parks ML, Kiernan H, Nercessian OA. Nerve injury after primary total knee arthroplasty. J Arthroplasty 2001;16:1048-54. [Google Scholar]
- 6.Horlocker TT, Cabanela ME, Wedel DJ. Does postoperative epidural analgesia increase the risk of peroneal nerve palsy after total knee arthroplasty? Anesth Analg 1994;79:495-500. [Google Scholar]
- 7.Webster DA, Murray DG. Complications of variable axis total knee arthroplasty. Clin Orthop Relat Res 1985;193:160-7. [Google Scholar]
- 8.Singh JA, Yu S, Chen L, Cleveland JD. Rates of total joint replacement in the Unites States: Future projections to 2020-2040 Using the National Inpatient Sample. J Rheumatol 2019;46:1134-40. [Google Scholar]
- 9.Krackow KA, Maar DC, Mont MA, Carroll C 4th. Surgical decompression for peroneal nerve palsy after total knee arthroplasty. Clin Orthop 1993;292:223-8. [Google Scholar]
- 10.Rajani AM, Mittal AR, Rajani K, Shah UA, Singhal R. 12-year functional outcome of patients undergoing total knee replacement with under-correction of Varus Deformity. J Truma Orthop Surg 2022 ;17:12-6. [Google Scholar]
- 11.Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB, Kinemax Outcomes Group. Validity and responsiveness of the knee society clinical rating system in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am 2001;83:1856-64. [Google Scholar]
- 12.Cohen EE, Van Duker B, Siegel S, Keon TP. Common peroneal nerve palsy associated with epidural analgesia. Anesth Analg 1993;76:429-31. [Google Scholar]
- 13.Bruzzone M, Ranawat A, Castoldi F, Dettoni F, Rossi P, Rossi R. The risk of direct peroneal nerve injury using the Ranawat “Inside-Out” lateral release technique in valgus total knee arthroplasty. J Arthroplasty 2010;25:161-5. [Google Scholar]
- 14.Rodríguez-Merchán E, De la Corte-Rodríguez H, Encinas-Ullán, CA. Peroneal nerve palsy after total knee arthroplasty: Prevalence, risk factors, diagnosis and management. In: Comprehensive Treatment of Knee Osteoarthritis. Cham: Springer; 2020. [Google Scholar]
- 15.Satardekar MB, Bhoir DV. Analysis and enhancement in the performance of electrical muscle stimulator. Int J Eng Sci Res Technol 2017;6:235-41. [Google Scholar]










