Flexion-type supracondylar humeral fractures have a risk of cubitus valgus deformity.
Dr. Hiroo Kimura, Department of Orthopaedic Surgery, Keio University School of Medicine, Tokyo, Japan. E-mail: kimura.9th.sep@gmail.com
Introduction: Supracondylar humeral fractures (SHFs) in children are mostly extension-type. SHFs have a high risk of cubitus varus deformity, while valgus deformity is rarely described. Nerve palsy can also occur during or after the injury, with most cases recovering spontaneously. Here, we present a rare case of cubitus valgus deformity after a flexion-type SHF with ulnar nerve (UN) palsy, which was successfully treated by corrective osteotomy and anterior transposition of the UN.
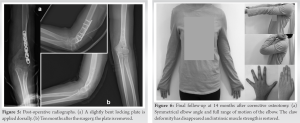
Case Report: A 10-year-old girl had left-sided cubitus valgus deformity with persistent UN palsy 4 months after open reduction and internal fixation (ORIF) at another hospital. Half a year after the initial operation, corrective osteotomy of the distal humerus with neurolysis and subcutaneous anterior transposition of the UN were performed. She showed excellent recovery 14-month postoperatively and reported restored motor and sensory function with symmetrical elbow appearance.
Conclusion: Surgeons usually observe the elbow angle carefully to avoid cubitus varus deformity. However, when treating a case of flexion-type SHFs, ORIF should be conducted to avoid cubitus valgus deformity, which could potentially cause UN traction as well as cosmetic dissatisfaction.
Keywords: Elbow, humerus, supracondylar fracture, ulnar nerve, cubitus valgus.
Supracondylar humeral fractures (SHFs) are the most ubiquitous fractures of the elbow in the pediatric population, comprising over half of all elbow fractures [1, 2]. The majority of SHFs are extension-type fractures and flexion-type fractures account for 2–5% [3, 4, 5, 6]. The challenge in SHF management is a high rate of complications, represented by cubitus varus deformity and nerve injury. Cubitus varus deformity is a common complication after SHFs, often requiring correction osteotomy depending on the degree of angulation. Nerve injury mostly recovers spontaneously without an intervention if mechanical issues are correctly addressed. Herein, we present a rare case of cubitus valgus deformity after a flexion-type SHF with ulnar nerve (UN) palsy, which did not recover in half a year. We successfully treated the lesion with corrective osteotomy and anterior transposition of the UN.
A 10-year-old right-handed girl fell from a monkey bar and sustained a left flexion-type SHF and a radial shaft fracture with UN palsy, which were immediately operated on at another hospital (Fig. 1a).

Contrary to cubitus varus deformity, cubitus valgus deformity following an SHF is poorly described. De Boeck et al. reviewed 196 SHF cases, with 10 cases (5.1%) showing radiographic cubitus valgus deformity [8], with incomplete correction identified as the main cause of deformity. They noted that cubitus valgus deformity occurred following collapse of the lateral column, as is the case with cubitus varus deformity following collapse of the medial column, which is often seen in an extension-type SHF. Kuoppala et al. reported that seven patients with flexion-type SHFs showed increased carrying angles (CA): the mean CA was 50% greater in injured elbows (21°) than in uninjured elbows (14°) [9]. Moreover, case reports by Hara et al. [10] and Vellingiri et al. [11] on the surgical treatment of flexion-type SHFs demonstrated an increased CA in all three patients at the final follow-up. In our case, the patient showed an increase in the HEW angle by 14°, and radiographic images revealed the presence of subtle comminution of the lateral column. Overall, a flexion-type SHF is more likely to result in cubitus valgus deformity than varus deformity; this may be due to the collapse of the lateral column. Although cubitus valgus deformity seldom produces an obviously unsatisfactory-appearing elbow [12], the possibility of cubitus valgus deformity should be recognized when treating flexion-type SHFs, and thus anatomical reduction should be aimed at. Flexion-type SHFs are frequently associated with UN palsy [13]. Kim et al. reported that six out of 23 cases of flexion-type SHFs presented with UN neurapraxia, which spontaneously resolved following observation [6]. Khademolhosseini et al. reported 272 cases of nerve injuries with SHFs, with resolution taking 3.5 months on average [14]. However, our patient did not show any improvement in half a year and thus underwent surgery. We estimated that the mechanism of residual UN palsy was as follows: The UN was adherent to surrounding soft tissues, with reduced mobility at this level, leading to distal stretching due to the cubitus valgus deformity. Therefore, it was thought that soon after neurolysis and anterior transposition of the UN, the symptoms started to improve. Despite the degree of valgus deformity not being severe, multiple factors provoked traction neuropathy of the UN, which prohibited spontaneous recovery.
We demonstrated a rare case of cubitus valgus deformity after a flexion-type SHF with UN palsy, which was successfully treated by corrective osteotomy and anterior transposition of the UN. Flexion-type SHFs could lead to cubitus valgus deformity, which should be well recognized during surgery, to achieve anatomical reduction.
When treating a patient with a flexion-type SHF, the possibility of cubitus valgus deformity should be recognized. Because the deformity could affect the UN as well as cosmesis (asymmetrical elbow appearance), anatomical reduction of the coronal plane in particular should be always aimed at.
References
- 1.Landin LA, Danielsson LG. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand 1986;57:309-12. [Google Scholar]
- 2.Emery KH, Zingula SN, Anton CG, Salisbury SR, Tamai J. Pediatric elbow fractures: A new angle on an old topic. Pediatr Radiol 2016;46:61-6. [Google Scholar]
- 3.Mahan ST, May CD, Kocher MS. Operative management of displaced flexion supracondylar humerus fractures in children. J Pediatr Orthop 2007;27:551-6. [Google Scholar]
- 4.Fowles JV, Kassab MT. Displaced supracondylar fractures of the elbow in children. A report on the fixation of extension and flexion fractures by two lateral percutaneous pins. J Bone Joint Surg Br 1974;56B:490-500. [Google Scholar]
- 5.Price CT, Flynn JM. Management of fractures. In: Lovell and Winter’s Pediatric Orthopaedics. Philadelphia, PA: Lippincott Williams and Wilkins; 2006. [Google Scholar]
- 6.Kim KY, Conaway W, Schell R, Hennrikus WL. Prevalence of ulnar nerve palsy with flexion-type supracondylar fractures of the humerus. J Pediatr Orthop B 2020;29:133-6. [Google Scholar]
- 7.Hasegawa M, Suzuki T, Kuroiwa T, Oka Y, Maeda A, Takeda H, et al. Reliability and validity of radiographic measurement of humerus-elbow-wrist angle in healthy children. JBJS Open Access 2017;2:e0012. [Google Scholar]
- 8.De Boeck H, De Smet P. Valgus deformity following supracondylar elbow fractures in children. Acta Orthop Belg 1997;63:240-4. [Google Scholar]
- 9.Kuoppala E, Parviainen R, Pokka T, Sirviö M, Serlo W, Sinikumpu JJ. Low incidence of flexion-type supracondylar humerus fractures but high rate of complications. Acta Orthop 2016;87:406-11. [Google Scholar]
- 10.Hara S, Kuriyama K, Shimada T, Abe S. Pediatric flexion type supracondylar fracture of the humerus: Two cases report. (in Japanese) J Jpn Elbow Soc 2021;28:1-3. [Google Scholar]
- 11.Vellingiri K, Suryanarayana MS, Sambathkumar B, Seenappa H. Surgical management of flexion type supracondylar humeral fracture with ulnar nerve injury-a report of a rare case. Cureus 2022;14:e26433. [Google Scholar]
- 12.Damsin JP, Langlais J. Supracondylar fractures. (in French) Rev Chir Orthop Reparatrice Appar Mot 1987;73:421-36. [Google Scholar]
- 13.Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: A meta-analysis. J Pediatr Orthop 2010;30:253-63. [Google Scholar]
- 14.Khademolhosseini M, Rashid AH, Ibrahim S. Nerve injuries in supracondylar fractures of the humerus in children: Is nerve exploration indicated? J Pediatr Orthop B 2013;22:123-6. [Google Scholar]











