Arthroscopic excision of localized Pigmented villonodular synovitis by piecemealing helps in decreasing tumor spillage, lower recurrence rate, and aids in faster recovery.
Dr. Rajkumar S Amaravathi, Division of Arthroscopy, Sports Injury, Joint Preservation and Regenerative Medicine, Department of Orthopaedics, St Johns Medical College, Bengaluru, Karnataka, India. E-mail: rajamarvathi@gmail.com
Introduction: Pigmented villonodular synovitis is an uncommon benign proliferation of the synovium. In the knee joint, it can present as a localized or a diffuse form and can mimic numerous conditions.
Case Report: We present a case report of a 54-year-old male with localized form of this condition. The diagnosis is not often made clinically but usually made with the help of magnetic resonance imaging and histopathology. We used a novel technique for resecting the tumor by arthroscopy.
Conclusion: A high index of suspicion is required for the diagnosis of the condition and arthroscopic excision results in lower morbidity and lesser recurrence rates.
Keywords: Pigmented villonodular synovitis, localized, synovium.
Pigmented villonodular synovitis (PVNS) is an uncommon benign proliferation occurring in the synovial joint, bursal membranes, and tendon sheath with an incidence of 1.8 per million [1]. It is seen in adults more commonly in the age group of 20–50 years and lesser frequently in the pediatric population [2]. It was first reported in 1852 by Chassaignac who identified it as a nodular lesion in the flexor tendon of the hand. In 1941, Jaffe, Lichtenstein, and Sutro coined the term and classified them as circumscribed and diffuse with similar histopathological features [3]. The circumscribed form is now termed as localized form, which may be pedunculated or sessile. Its most common location is the knee joint specifically arising from the meniscocapsular junction, Hoffa’s fat pad, lateral recess, and tibial eminence [4].
A 54-year-old male came with complaints of the left knee pain for 6-month duration which was insidious in onset and was associated with diffuse swelling. He had been evaluated in multiple hospitals and treated with analgesics, therapeutic knee aspiration, and compression bandage application. They were no history of preceding trauma, locking sensation, fever, constitutional symptoms, or night cries. On examination, there was diffuse fullness of the left knee with positive patellar tap (Fig. 1). The range of movement was 0–100° with pain during terminal flexion, and there was no evidence of ligamentous instability. The radiographs were unremarkable, magnetic resonance imaging (MRI) showed a T2 hypointense lesion in Hoffa’s fat pad arising from the synovium measuring 2.5×4.5×2.Fig. 2).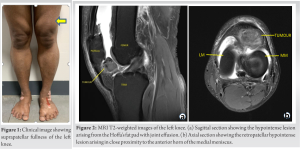
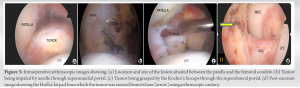
Due to the large extent of the tumor, the following steps were carried out to resect it:
- Superolateral and superomedial portals were made in addition to the standard arthroscopic portals
- On visualizing the entire extent of the tumor, it was grasped from the superolateral portal using a Kocher forceps after impaling it with a needle. Impaling the tumor gives stable conditions to resect the tumor
- The intra-articular resection was carried out by piecemealing the tumor using arthroscopic cautery (Vulcan) from the superomedial portal
- Following which the tumor was resected from its base attachment near the anterior horn of the medial meniscus using arthroscopic cautery and shaver.
Histopathology showed fragments of synovial tissue with inflammatory cell infiltrate comprising lymphocyte admixed with any foamy cells and hemosiderin-laden macrophages. Extensive areas of hyalinization and fibrous areas mimicking osteoid with fibromuscular and fibro collagenous tissue regions were noted (Fig. 4). The immediate post-operative period was uneventful and the patient returned to his daily activities after the 2nd post-operative week. There was no recurrence of symptoms after 1 year of post-operative period of follow-up.
Classically, there are three types of PVNS, an extra-articular localized tumor arising from the tendon sheath also known as a giant cell tumor of the tendon sheath. Second is an intra-articular localized tumor most commonly found in the knee seen in meniscocapsular junction [5], lateral recess, suprapatellar recess, Hoffa’s fat pad, and posterior compartment of the knee in order of decreasing frequency [6]. Third is a diffuse variety which is a monoarticular proliferation of the synovium most common site being the knee followed by hip, ankle, shoulder, and elbow [7]. Fisk had postulated that PVNS occurs due to repeated microtrauma and hydroarthrosis occurring in the synovial fringes [8]. However, there is a lot of speculation regarding the etiology being neoplastic or a result of an inflammatory process. The clinical presentation is very non-specific for the localized type of PVNS unlike the classic symptoms of diffuse PVNS and therefore, a clinical diagnosis is very challenging [9]. The initial presentation is mild-to-moderate knee pain or in some cases, patients refer it to as discomfort in the knee. Localized PVNS may present as a palpable mass or may cause a locking sensation in the knee or restricted terminal range of movement [10]. Clinically, the localized lesions can mimic meniscal injuries or other intra-articular pathologies and hence, formulating a surgical plan after locating the lesion on MRI is advisable [6]. The radiology might reveal a soft-tissue shadow and the MRI shows a low signal intensity in the T1- and T2-weighted images and a large joint effusion. Bony erosions and hypertrophied synovium are the additional features. The hypointense signals are the result of the hemosiderin deposits in the synovium [11]. Macroscopically, they may be sessile or pedunculated yellowish-brown masses firm to elastic inconsistency and on the cut section, they have variegated surfaces with focal areas of hemorrhage [12]. Histopathology shows active proliferation of fibroblastic and histiocytic element showing an evident macrophagic activity with phagocytosis and abundant hemosiderin and lipids [13]. Excision of the localized PVNS tumor is the mainstay of the treatment, arthroscopic excision is the preferred method in this type, and as it allows for identifying the size and location of small localized lesions accurately. Being less invasive is associated with decreased complications, lower morbidity, shorter hospital stay, and a lower recurrence rate as compared to the open method of excising the tumor [14]. The localized form has a low recurrence rate of around 8% when surgically managed appropriately.
Localized PVNS is an uncommon condition and a high degree of clinical suspicion is required to diagnose this condition. MRI is the diagnostic modality of choice. However, it can be confirmed only by histopathology. Arthroscopy plays an instrumental role in the diagnosis and surgical excision with lower morbidity and recurrence rates.
A high index of suspicion is required for the diagnosis of localized PVNS and arthroscopic excision results in lower morbidity and lesser recurrence rates.
References
- 1.Karami M, Soleimani M, Shari R. Pigmented villonodular synovitis in the pediatric population: Review of literature and a case report. Pediatr Rheumatol Online J 2018;16:6. [Google Scholar]
- 2.Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: A retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum 2011;40:539-46. [Google Scholar]
- 3.Bentley G, McAuliffe T. Pigmented villonodular synovitis. Ann Rheum Dis 1990;49:15-6. [Google Scholar]
- 4.Hernandez AJ, Camanho GL, Laraya MH, Fávaro E, Filho MM. Localized pigmented villonodular synovitis of the knee : An arthroscopic treatment. Acta Ortop Bras 2005;13:76-8. [Google Scholar]
- 5.Lee BI, Yoo JE, Lee SH, Min KD. Localized pigmented villonodular synovitis of the knee: Arthroscopic treatment. Arthroscopy 1998;14:764-8. [Google Scholar]
- 6.Noailles T, Brulefert K, Briand S, Longis PM, Andrieu K, Chalopin A, et al. Giant cell tumor of tendon sheath: Open surgery or arthroscopic synovectomy? A systematic review of the literature. Orthop Traumatol Surg Res 2017;103:809-14. [Google Scholar]
- 7.Brashear HR. Pigmented villonodular synovitis. South Med J 1956;49:679-84. [Google Scholar]
- 8.Fisk GR. Hyperplasia and metaplasia in the synovial membrane. Ann R Coll Surg Engl 1952;11:157-70. [Google Scholar]
- 9.Bouguennec N, Meyer A, Graveleau N. Localized form of pigmented villonodular synovitis of the knee: The meniscal mime. Orthop Traumatol Surg Res 2014;100:255-8. [Google Scholar]
- 10.Jobe CM, Raza A, Zuckerman L. Pigmented villonodular synovitis: Extrasynovial recurrence. Arthroscopy 2011;27:1449-51. [Google Scholar]
- 11.Holiday Q, Fernandez R. Diffuse pigmented villonodular synovitis of the elbow. Joint Bone Spine 2021;88:105278. [Google Scholar]
- 12.Loriaut P, Djian P, Boyer T, Bonvarlet JP, Delin C, Makridis KG. Arthroscopic treatment of localized pigmented villonodular synovitis of the knee. Knee Surg Sport Traumatol Arthrosc 2012;20:1550-3. [Google Scholar]
- 13.Patnaik CS. A case of localized pigmented villonodular synovitis presenting as loose body in the knee joint. MOJ Orthop Rheumatol 2014;1:125-7. [Google Scholar]
- 14.De Ponti A, Sansone V, Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy 2003;19:602-7. [Google Scholar]
- 15.Venkateswarlu CH, Rao AS. International VS of K-R of 2 C. J Curr Med Appl Sci 2016;9:89-91. [Google Scholar]