Osteochondromas can contribute to attritional tendon rupture in certain situations; osteochondromas occurring near anatomically important tendons should prompt additional care and follow up.
Dr. Lorraine A T Boakye, Orthopedic Foot and Ankle Center, University of Pennsylvania, 230 W Washington Square, 230 W Washington Square, 5th Fl Farm Journal Bldg, Philadelphia, PA 19106, US. E-mail: lorraineboakye7@gmail.com
Introduction: The presentation of the included patient is unique, and the thought process regarding management algorithms used to manage this patient is important to discuss so that other surgeons may benefit. This is the first report of its kind, to our knowledge.
Case Report: A 30-year-old healthy Caucasian male presented with acute Achilles tendon rupture after feeling a pop while playing basketball, in the setting of a known posterior tibial osteochondroma and a recent increase in physical activity.
Conclusion: The resultant injury is likely due to mechanical irritation at the tendon site, which caused wear over time and eventual acute rupture. We expanded our percutaneous repair to include an evaluation of the posterior compartment to adequately visualize and excise the large bony lesion. Therefore, we conclude that it is reasonable to counsel patients with known osteochondromas in this location due to the risk of possible Achilles injury, particularly if at all symptomatic.
Keywords: Achilles tendon rupture, osteochondroma, tendinopathy.
Osteochondromas are the most common benign bone lesion, comprising 20–50% of all benign bone neoplasms and 10–15% of all osteogenic tumors [1]. The exact incidence is not known, as solitary osteochondromas are often asymptomatic and are not identified by clinicians. Current estimates place the prevalence at 0.5–3% [2]. Symptoms arise from the mass effect or irritation of surrounding structures. Long bones are the most common sites of disease, which corresponds to the sites of the most rapid bone growth. An osteochondroma is a cartilage-capped projection of bone arising from the external surface of the bone [3]. It is often characterized as an exophytic lesion located juxtacortical in the metaphysis. The lesions contain a marrow cavity that is continuous with the cavity of the bone from which they arise [2]. Achilles tendon ruptures are a common activity-related lower extremity injury. The incidence has increased in recent decades from 2 to 37/100,000-person-year [4]. The diagnosis is missed on initial presentation in up to 25% of cases [4]. The injury occurs predictably in the hypovascular region, about 4–6 cm proximal to the calcaneal insertion. The most common mechanism of injury is sudden eccentric plantar flexion or forced dorsiflexion of a plantar-flexed foot [5]. The injury occurs most often in males in the third and fourth decades of life [6]. Risk factors may be classified as extrinsic or intrinsic etiologies. Extrinsic factors include overuse, episodic participation in athletics, and fluoroquinolone or corticosteroid use [6]. Intrinsic factors may result in accelerated tendon degeneration and can include subtalar hyperpronation, increased femoral anteversion, leg length discrepancy, and decreased musculotendinous flexibility [4]. Direct mechanical irritation to the tendon is an uncommon but possible cause of chronic tendon injury and could represent a risk factor for rupture. In this case report, we describe a case of Achilles rupture at the site of a symptomatic osteochondroma as well as the subsequent management.
A 30-year-old healthy Caucasian male presented to the emergency room after feeling a pop while playing basketball. He had a history of recurrent intermittent posterior calf pain. He endorsed having recently trained for and completed a marathon two weeks before the presentation. His initial management was for a presumptive Achilles rupture; he was placed in a boot and advised to be weight-bearing as tolerated. He then presented to an orthopedic foot and ankle clinic for follow-up. His examination was notable for a palpable defect in the Achilles tendon, about 3 cm proximal to the insertion. There was asymmetry in the resting position of his feet when prone with his knees flexed, and Thompson’s test was abnormal. He was also noted to have a prominent bony mass in his posterior calf. The bony prominence was in close proximity to the Achilles rupture site. He was aware of the prominence and told during adolescence that it was a benign bony growth. The bone mass had previously caused irritation in his calf with restrictive shoe wear, the donning of boots, and activities requiring significant pushoff and forced dorsiflexion. The aforementioned irritants lead to a history of well-established symptoms of discomfort near the site of the current injury. The patient noted a “pulling” sensation at his Achilles tendon during symptomatic periods. Despite having known symptoms, he had not experienced discomfort or functional limitations significant enough to consider specialist care. The patient did not have a history of bony lesions at other sites and denied familial or hereditary genetic conditions associated with multiple bony lesions. We believe this solitary lesion was sporadic in nature. Radiographic evaluation at presentation was significant for posterior bony prominence in the distal tibia with soft tissue irregularity at the Achilles tendon proximal to the insertion (Fig. 1).  The patient sustained an acute traumatic Achilles tendon rupture in the setting of a longstanding osteochondroma in the posterior tibia. On exam, the rupture site was very close to the site of the osteochondroma. We discussed treatment options, both operative and nonoperative, and ultimately, he elected to proceed with surgery. The surgical plan included Achilles tendon repair and excision of the posterior tibial osteochondroma to prevent future mechanical irritation at the repair site. A posterior open incision was made and carried down through skin and subcutaneous tissue to the paratenon (Fig. 2). The tendon rupture was identified (Fig. 3). The edges were cleaned, and any nonviable portions were debrided. Next, we found the bony mass was immediately palpable and in contact with the tendon. The lesion had eroded through the anterior paratenon, and the posterior tip was visible through the rupture site (Fig. 4).
The patient sustained an acute traumatic Achilles tendon rupture in the setting of a longstanding osteochondroma in the posterior tibia. On exam, the rupture site was very close to the site of the osteochondroma. We discussed treatment options, both operative and nonoperative, and ultimately, he elected to proceed with surgery. The surgical plan included Achilles tendon repair and excision of the posterior tibial osteochondroma to prevent future mechanical irritation at the repair site. A posterior open incision was made and carried down through skin and subcutaneous tissue to the paratenon (Fig. 2). The tendon rupture was identified (Fig. 3). The edges were cleaned, and any nonviable portions were debrided. Next, we found the bony mass was immediately palpable and in contact with the tendon. The lesion had eroded through the anterior paratenon, and the posterior tip was visible through the rupture site (Fig. 4).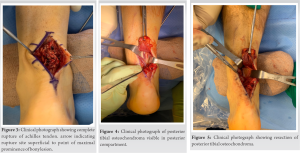 Therefore, we elected to proceed with the excision of the osteochondroma. We opened the deep compartment, mobilized the FHL tendon laterally, and dissected between the neurovascular bundle and the muscle belly. We exposed the bony mass, isolated it from all surrounding tissue, and then used an osteotome to remove it. Once the mass was no longer prominent, we used a rasp to smooth any sharp edges (Fig. 5). We confirmed appropriate resection both clinically and fluoroscopically, irrigated the site, and placed bone wax on open areas to prevent regrowth and augment hemostasis from bleeding bone. The ruptured tendon was repaired using Suture Tape (Arthrex, Inc., Naples, FL) with a running Krakow proximal and distal. The tendon edges were approximated, and sutures were tied together to complete the Achilles tendon repair. This was then augmented with a running-peritendinous repair. The wound was closed in layers and splinted in resting plantarflexion. He was made non-weightbearing for 2 weeks, followed by the initiation of our usual functional rehabilitation protocol [7]. The resected lesion was evaluated by pathology. The gross specimen was found to be partially surfaced with roughened cartilage. Histologic exam findings were consistent with exostosis with fatty marrow and focal partially acellular trabeculae (Fig. 6).
Therefore, we elected to proceed with the excision of the osteochondroma. We opened the deep compartment, mobilized the FHL tendon laterally, and dissected between the neurovascular bundle and the muscle belly. We exposed the bony mass, isolated it from all surrounding tissue, and then used an osteotome to remove it. Once the mass was no longer prominent, we used a rasp to smooth any sharp edges (Fig. 5). We confirmed appropriate resection both clinically and fluoroscopically, irrigated the site, and placed bone wax on open areas to prevent regrowth and augment hemostasis from bleeding bone. The ruptured tendon was repaired using Suture Tape (Arthrex, Inc., Naples, FL) with a running Krakow proximal and distal. The tendon edges were approximated, and sutures were tied together to complete the Achilles tendon repair. This was then augmented with a running-peritendinous repair. The wound was closed in layers and splinted in resting plantarflexion. He was made non-weightbearing for 2 weeks, followed by the initiation of our usual functional rehabilitation protocol [7]. The resected lesion was evaluated by pathology. The gross specimen was found to be partially surfaced with roughened cartilage. Histologic exam findings were consistent with exostosis with fatty marrow and focal partially acellular trabeculae (Fig. 6).  At his first post-operative evaluation, 2 weeks post-surgery, his wound was well healed, radiographs were obtained, and he started physical therapy (PT) (Fig. 7).
At his first post-operative evaluation, 2 weeks post-surgery, his wound was well healed, radiographs were obtained, and he started physical therapy (PT) (Fig. 7).  He continued to do well with minimal pain and had made progress regarding range of motion with PT. He noted some subjective stiffness in the great toe range of motion, which was resolved by the final follow-up. At 3 months post-operatively, he was participating in PT and continued to do well. He has returned to work without issue and is resuming athletic activities. At the final follow-up, he reported no pain with activities and that he had returned to running 4 miles a day as well as playing basketball recreationally. He feels clinically improved and is particularly relieved to no longer feel the mass in his posterior calf.
He continued to do well with minimal pain and had made progress regarding range of motion with PT. He noted some subjective stiffness in the great toe range of motion, which was resolved by the final follow-up. At 3 months post-operatively, he was participating in PT and continued to do well. He has returned to work without issue and is resuming athletic activities. At the final follow-up, he reported no pain with activities and that he had returned to running 4 miles a day as well as playing basketball recreationally. He feels clinically improved and is particularly relieved to no longer feel the mass in his posterior calf.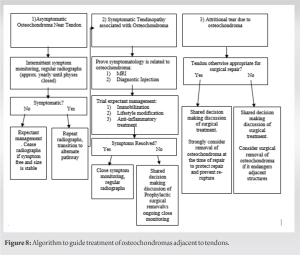
This case is novel in that it is the first to describe an Achilles rupture in the setting of posterior tibial osteochondroma. A careful understanding of factors contributing to Achilles rupture is required for appropriate and definitive treatment. The chronic mechanical irritation to the Achilles tendon from prominent bony impingement likely played a role in the acute rupture event. There are many factors in the patient’s presentation that elucidate the likely role the mechanical irritation played in the eventual rupture. Firstly, the patient had chronic intermittent symptoms of irritation with certain shoe wear and increased activity with a known palpable mass in the area. Secondly, the osteochondroma protruded through the rupture, lending credence to the theory that the protuberance at the site of the rupture contributed to the rupture itself. Given these findings, we felt it was necessary to address this aspect of his anatomy concomitantly to prevent a possible re-rupture or other complications that would cause functional limitation. While non-operative management of Achilles ruptures has established literature to support its implementation, it is not clear how this patient’s pre-existing symptoms from his osteochondroma would have mitigated its effectiveness [8]. Therefore, after careful consideration of non-operative and operative management, the patient elected to proceed with surgical intervention and address both issues at once. Osteochondromas arise from the metaphysis of long bones due to disordered growth at the physis [1]. Endochondral ossification at the physis leads to perpendicular and parallel vectored growth relative to the physis. A hyaline cartilaginous cap covers the distal end of the lesion, which grows away from the nearest joint and epiphysis. The morphology can be either sessile or pedunculated. Both types of osteochondroma display a cauliflower-shaped marginal expansion and retain the cortex and periosteum of the parent bone [3]. These lesions are physeal; thus, they experience proportional growth until skeletal maturity. Solitary osteochondromas are thought to be spontaneous; however, physeal injury via Salter-Harris fracture, surgery, or radiation therapy are risk factors for their formation [2]. Most osteochondromas are incidentally found and asymptomatic [9]. This contrasts with symptomatic solitary lesions, which occur predominantly in young patients. As many as 75–80% are discovered by age 20 [9]. Additionally, there seems to be an unexplained male predominance of 1.6–3.4 to 1 [9]. The existing literature regarding osteochondromas includes many case reports and/or small cohort studies of symptomatic osteochondromas presenting with mass effect syndromes, similar to our patient’s presentation.[8,10,11] Additional mass effect presentations include vascular compromise [8,12,13], peripheral neurologic entrapment [14], overlying bursitis [15], clinical deformity [16] and fracture [17] have also been reported. Tendinopathy and tendon rupture due to mechanical irritation or repetitive microtrauma in the setting of impingement are the most commonly reported occurrence. Reize and Buess described an atraumatic subscapularis tear associated with a humeral osteochondroma [18], and Reichmister et al. similarly described rotator cuff impingement and pain associated with clavicular osteochondromas [19]. Distal biceps tendon ruptures in the setting of an impinging osteochondroma have also been reported by Kim et al. [20]. Additionally, there are reported cases of digital tendon rupture due to carpal osteochondromas near the flexor pollicis longus [21] and extensor digiti minimi [22]. Literature reviews conclude that symptomatic osteochondromas around the ankle are rare. Of these rare lesions, most are reported to be found in the talus [23, 24, 25, 26]. The lesions most commonly remain an incidental finding following athletic injuries [23]; however, some of the lesions have associated mass effect irritation due to shoe wear [4], restricted range of motion due to impingement [24, 25, 26], sinus tarsi syndrome [27, 28] clinical deformity [25, 29] and even nerve impingement [26]. We find that the majority of these may be managed non-operatively; however, surgery may be more appropriate in cases of deformity, intractable mechanical irritation, or impending fracture. Osteochondroma-mediated tendon irritation about the ankle is very rare, and tendon rupture remains even less frequently reported. At this time, the presented case is the first of an Achilles rupture attributable to osteochondroma attritional wear. The above literature review highlights that osteochondromas, although mostly asymptomatic, can present with varied clinical syndromes, including attritional tendinopathy. It is reasonable to ask whether any osteochondroma-induced tendon rupture is preventable. Certainly, it is not in the setting of unrecognized, asymptomatic lesions; however, other presentations may benefit from prophylactic treatment. We explore those implications and present a potential algorithm to guide treatment (Fig. 8).
Patients can present in three different categories of attritional tendinopathy due to osteochondromas; addressing each in turn, these are:
- Asymptomatic cases where the anatomical location of the osteochondroma could possibly cause tendinopathy. This will represent the majority of cases, as most osteochondromas are incidental findings. In these cases, no surgical treatment is indicated; however, monitoring is prudent. Once the osteochondroma is stabilized and the patient continues to be asymptomatic, monitoring can be stopped as long as the presence of osteochondroma is well documented in the medical record. If the osteochondroma begins to cause tendinopathy, the patient will transition to the symptomatic treatment pathway.
- Patients with symptomatic tendinopathy necessitate additional treatment and care. The first objective is to determine if the osteochondroma directly contributes to the attritional pathology. This should be done with the use of advanced imaging and diagnostic procedures. Magnetic resonance imaging provides the best visualization of soft tissues and is thus the treatment modality of choice. Attritional tendinopathy directly related to osteochondromas will demonstrate inflammation of the tendon in question at the site of the osteochondroma. A diagnostic injection may be used to both further delineate the site of irritation as well as predict pain relief after surgical removal if the anatomic area is amenable to injection. Despite proving the pathologic involvement of osteochondroma, a non-surgical approach should be the first line of treatment for attritional tendinopathy. This includes short-term immobilization and anti-inflammatory treatments. In certain cases where non-surgical treatment is desired, lifestyle modification may be indicated to decrease stress on the tendon in question. If the patient fails nonoperative management, surgery can be considered. A careful discussion of the risks and benefits of surgery, concurrent with the patient’s wishes, should be performed in the prophylactic setting.
- Should the patient present with a complete tear of a tendon near or directly attributable to an osteochondroma, a different pathway should be discussed. If the tendon is one that otherwise would be appropriate for surgical repair, the presence of the osteochondroma does not warrant an alternate to the typical considerations for surgical management. In the absence of a required tendon repair, removal may be considered if additional adjacent structures are at risk. In the setting of a necessary tendon repair or reconstruction, the osteochondroma should be excised as long as the risk of excision does not outweigh the benefits of reconstruction. Removal in this case is intended to protect the repair and prevent re-rupture.
The etiology of our patient’s posterior tibial osteochondroma is thought to be spontaneous, as there is no history of pediatric physeal injury and no clear timeline of symptom onset and workup that may further elucidate its development. Given the clinical symptoms and patient’s history, it is likely that there was mechanical irritation at the tendon site, which caused attrition over time. This predisposed the patient to an eventual acute rupture. It is also possible that his recent marathon training further exacerbated this process. We expanded our typical limited-incision percutaneous repair to include evaluation of the posterior compartment fascia and musculature to adequately visualize the large bony lesion. We believe that his outcome will be similar to other acute ruptures repaired as above, given the elimination of the critical inciting factor. Given the additional case reports of attritional tendinopathy due to osteochondromas in the literature, we feel that our proposed guideline may be beneficial to other practitioners addressing osteochondroma-related tendinopathy.
It is a reasonable conclusion to counsel patients with known osteochondromas in this location regarding the risk of possible Achilles injury, particularly if symptomatic. Furthermore, we present a broad set of guidelines where osteochondromas causing attritional tendinopathy at any anatomic location can be considered for prophylactic excision after failure of non-operative treatment. Lastly, we present the removal of the Achilles-related osteochondroma as a model for treatment in tendon rupture where repair is otherwise deemed most clinically appropriate.
References
- 1.Wodajo FM. Top five lesions that do not need referral to orthopedic oncology. Orthop Clin North Am 2015;46:303-14. [Google Scholar]
- 2.Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: Review of the clinical, radiological and pathological features. In Vivo 2008;22:633-46. [Google Scholar]
- 3.Scarborough MT, Moreau G. Benign cartilage tumors. Orthop Clin North Am 1996;27:583-9. [Google Scholar]
- 4.Hess GW. Achilles tendon rupture: A review of etiology, population, anatomy, risk factors, and injury prevention. Foot Ankle Spec 2010;3:29-32. [Google Scholar]
- 5.Chiodo CP, Glazebrook M, Bluman EM, Cohen BE, Femino JE, Giza E, et al. Diagnosis and treatment of acute Achilles tendon rupture. J Am Acad Orthop Surg 2010;18:503-10. [Google Scholar]
- 6.Noback PC, Jang ES, Cuellar DO, Seetharaman M, Malagoli E, Greisberg JK, et al. Risk factors for Achilles tendon rupture: A matched case control study. Injury 2017;48:2342-7. [Google Scholar]
- 7.Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: A multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am 2010;92:2767-75. [Google Scholar]
- 8.Shore RM, Poznanski AK, Anandappa EC, Dias LS. Arterial and venous compromise by an osteochondroma. Pediatr Radiol 1994;24:39-40. [Google Scholar]
- 9.Giudici MA, Moser RP Jr., Kransdorf MJ. Cartilaginous bone tumors. Radiol Clin North Am 1993;31:237-25. [Google Scholar]
- 10.Karasick D, Schweitzer ME, Eschelman DJ. Symptomatic osteochondromas: Imaging features. AJR Am J Roentgenol 1997;168:1507-12 [Google Scholar]
- 11.Karasick D, Schweitzer ME, Eschelman DJ. Symptomatic osteochondromas: Imaging features. AJR Am J Roentgenol 1997;168:1507-12. [Google Scholar]
- 12.Vallance R, Hamblen DL, Kelly IG. Vascular complications of osteochondroma. Clin Radiol 1985;36:639-42. [Google Scholar]
- 13.Andrikopoulos V, Skourtis G, Papacharalambous G, Antoniou I, Tsolias K, Panoussis P. Arterial compromise caused by lower limb osteochondroma. Vasc Endovascular Surg 2003;37:185-90. [Google Scholar]
- 14.Cardelia JM, Dormans JP, Drummond DS, Davidson RS, Duhaime C, Sutton L. Proximal fibular osteochondroma with associated peroneal nerve palsy: A review of six cases. J Pediatr Orthop 1995;15:574-7. [Google Scholar]
- 15.Unni KK. Osteochondroma (osteocartilaginous exostosis). In: Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed. Springfield, Ill: Thomas; 1996. p. 11-23. [Google Scholar]
- 16.Keith A. Studies in the anatomical changes which accompany certain growth-disorders of the human body. J Anat 1920;54:101-5. [Google Scholar]
- 17.Davids JR, Glancy GL, Eilert RE. Fracture through the stalk of pedunculated osteochondromas: A report of three cases. Clin Orthop 1991;271:258-64. [Google Scholar]
- 18.Reize F, Buess E. Humeral osteochondroma causing a subscapularis tear: A rare source of shoulder dysfunction. Arch Orthop Trauma Surg 2007;127:67-70. [Google Scholar]
- 19.Reichmister J, Reeder JD, Gold DL. Osteochondroma of the distal clavicle: An unusual cause of rotator cuff impingement. Am J Orthop (Belle Mead NJ) 2000;20:807-9. [Google Scholar]
- 20.Kim JP, Seo JB, Kim MH, Yoo MJ, Min BK, Moon SY. Osteochondroma associated with complete rupture of the distal biceps tendon: Case report. J Hand Surg Am 2010;35:1340-3. [Google Scholar]
- 21.O’Dwyer KJ, Jefferiss CD. Scaphoid exostosis causing rupture of the flexor pollicis longus. Acta Orthop Belg 1994;60:124-6. [Google Scholar]
- 22.Shah NR, Wilczynski M, Gelberman R. Osteochondroma of the capitate causing rupture of the extensor digiti minimi: Case report. J Hand Surg Am 2009;34:46-8. [Google Scholar]
- 23.Montella BJ, O‘Farrell DA, Furr WS, Harrelson JM. Fibular osteochondroma presenting as chronic ankle sprain. Foot Ankle Int 1995;16:207-9. [Google Scholar]
- 24.Ercin E, Bilgili MG, Gamsizkan M, Avsar S. Talar osteochondroma fracture presenting as posterior ankle impingement. J Am Podiatr Med Assoc 2016;106:225-8. [Google Scholar]
- 25.Appy-Fedida B, Krief E, Deroussen F, Plancq MC, Collet LM, Klein C, et al. Mitigating risk of ankle valgus from ankle osteochondroma resection using a transfibular approach: A retrospective study with six years of follow-up. J Foot Ankle Surg 2017;56:564-7. [Google Scholar]
- 26.Andreacchio A, Marengo L, Canavese F. Solitary osteochondroma of the sinus tarsi. J Pediatr Orthop B 2018;27:88-91. [Google Scholar]
- 27.Pham L, Wu D. Rare osteochondroma of the posterior talar process: A case report. J Am Podiatr Med Assoc 2021;111:15. [Google Scholar]
- 28.Lee JH, Rathod CM, Park H, Lee HS, Rhee I, Kim HW. Longitudinal observation of changes in the ankle alignment and tibiofibular relationships in hereditary multiple exostoses. Diagnostics (Basel) 2020;10:752. [Google Scholar]
- 29.Herrera-Perez M, De Mendoza MA, De Bergua-Domingo JM, Pais-Brito JL. Osteochondromas around the ankle: Report of a case and literature review. Int J Surg Case Rep 2013;4:1025-7. [Google Scholar]








