Cognizance of a non-accidental trauma to a child is crucial to prevent future psychological dilemmas.
Dr. Adnan Anwer, Department of Orthopaedic Surgery, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. E-mail: dr.adnan.amu@gmail.com
Introduction: Chondro-epiphyseal separation of the distal humerus is a rare injury, which can occur as a consequence of excessive traction on the upper extremity accompanying a dystocic birth or one complicated by cephalopelvic disproportion. Such fracture patterns can also result from a combination of rotatory and shear forces, also typically seen following child abuse. It can be easily mistaken for a posterior elbow dislocation, creating a delay in diagnosis. Since unossified cartilage cannot be seen radiographically, these injuries are better appreciated by ultrasound or magnetic resonance imaging.
Case Report: We present a case of an 8-day-old neonate who presented with pseudoparesis of the left arm following birth. Posterior displacement of the elbow joint was identified on the radiograph. On ultrasound, a trans-physical supracondylar distal humerus fracture was identified. This was presumed as trauma secondary to a difficult delivery. At the 11th week of follow-up, the patient presented with a fracture of the right proximal tibia, followed by a fracture shaft left femur at 5 months of follow-up. Chest X-ray at this time revealed uniting rib fractures with callus formation. After ruling out any congenital collagen disorder (osteogenesis imperfecta), the patient was diagnosed with a case of battered baby syndrome. The case was reported to child protection services and parents were questioned and counseled for the same.
Conclusion: This case report highlights the importance of a high degree of suspicion of child abuse in any child with a rare fracture pattern, uncommon serial fracture occurrence, and unconventional clinic-radiological presentation.
Keywords: Neonate, birth trauma, physeal separation, battered baby, child abuse.
Bilateral distal humerus physeal separation is a rare entity, which usually occurs in children <2 years old [1, 2, 3]. The mechanisms of injury generally responsible for such trauma are either fall on an outstretched hand or hyperextension and forceful rotation of the forearm and elbow [1]. Hence, chondro-epiphyseal separation of the distal humerus can rarely occur as a consequence of excessive traction on the upper extremity accompanying a dystocic birth or one complicated by cephalopelvic disproportion [4, 5]. Apart from birth-related trauma, this rare pattern of injury occurring in bilateral upper limbs is also possible with either a skeletal developmental defect or child abuse. The initial imaging modality for evaluating injuries around the elbow joint is radiography. However, the capitellum ossification center typically appears around 8 months of age, and therefore in children younger than that, most of the distal humerus epiphysis is cartilaginous [1, 2]. On a radiograph, distal humerus physeal separation can be misdiagnosed as elbow dislocation in children because the cartilaginous epiphysis is radiolucent. A high degree of clinical suspicion reinforced by history supportive of such injury and that elbow dislocation is rare in neonates, is therefore warranted to make the diagnosis. Hence, ultrasonography is a useful evaluation tool in young children for evaluating musculoskeletal abnormalities [2, 6]. In this case report, our goal is to highlight a rare pattern of physeal separation injury in a neonate, its diagnostic dilemma, and alarming clinicians of a potential child abuse early on witnessing this injury in bilateral upper extremities.
We present a case of an 8-day-old neonate who presented to the outpatient clinic with swelling and deformity over the right elbow, left elbow, and left knee. The child was born full-term, through normal vaginal route and the delivery was uneventful. The child cried immediately after birth and started breastfeeding during the 1st h of delivery. The child was discharged under satisfactory conditions and no bony abnormality or abnormal attitude of the limb was noted at the time of discharge. On performing radiographs (Fig. 1) and ultrasonographic examination (Fig. 2) of both the upper and lower limbs, the patient was diagnosed with bilateral distal humeral physeal separation with the left proximal tibia physeal injury. 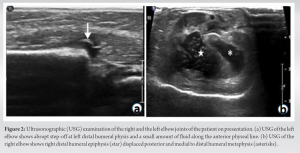 Although unsure, the etiology of multiple fractures at this age was considered most likely to be “birth-related trauma”. The patient’s injuries were managed conservatively by minimal traction application and splinting the limbs in a cuff and collar sling. At 4 weeks follow-up, there was evidence of fracture healing present with bridging callus formation with no further complaints. Three months later, the child was brought to the outpatient clinic for follow-up when swelling and abnormal posture of the right knee was observed. Antero-posterior (AP) and lateral radiographs (Fig. 3d) of the right knee revealed a fracture right proximal tibia and fracture mid-shaft right fibula, with healing callus formation present.
Although unsure, the etiology of multiple fractures at this age was considered most likely to be “birth-related trauma”. The patient’s injuries were managed conservatively by minimal traction application and splinting the limbs in a cuff and collar sling. At 4 weeks follow-up, there was evidence of fracture healing present with bridging callus formation with no further complaints. Three months later, the child was brought to the outpatient clinic for follow-up when swelling and abnormal posture of the right knee was observed. Antero-posterior (AP) and lateral radiographs (Fig. 3d) of the right knee revealed a fracture right proximal tibia and fracture mid-shaft right fibula, with healing callus formation present. 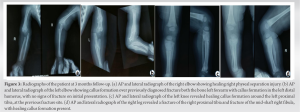 Follow-up radiographs of both the elbow joints and the left knee joint (AP and lateral views) revealed well-healing physeal injury with callus formation around fractured both bones of the left forearm. Moreover, it showed callus formation in the left distal humerus also with no signs of fracture on initial presentation. On questioning the parents, they revealed that they loved their only born child a lot and that they believed he had a tendency of easy bruising and injuring easily. For this, complete workup for any congenital or collagen disorder was done, revealing no significant results. At 5 months follow-up, the child was brought with a newly developed deformity of the left thigh, for which radiographs (AP and lateral), Fig. 4a, were done and the patient was diagnosed with mid-shaft fracture left femur. Furthermore, a radiograph of the chest (AP view), Fig. 4b, showed multiple rib fractures, at different stages of healing and callus formation. At this stage, with ongoing new-onset injuries, the patient was diagnosed as a case of “Battered Baby Syndrome”.
Follow-up radiographs of both the elbow joints and the left knee joint (AP and lateral views) revealed well-healing physeal injury with callus formation around fractured both bones of the left forearm. Moreover, it showed callus formation in the left distal humerus also with no signs of fracture on initial presentation. On questioning the parents, they revealed that they loved their only born child a lot and that they believed he had a tendency of easy bruising and injuring easily. For this, complete workup for any congenital or collagen disorder was done, revealing no significant results. At 5 months follow-up, the child was brought with a newly developed deformity of the left thigh, for which radiographs (AP and lateral), Fig. 4a, were done and the patient was diagnosed with mid-shaft fracture left femur. Furthermore, a radiograph of the chest (AP view), Fig. 4b, showed multiple rib fractures, at different stages of healing and callus formation. At this stage, with ongoing new-onset injuries, the patient was diagnosed as a case of “Battered Baby Syndrome”.  The case was reported to child protection services and other concerned authorities and the patient was managed conservatively. Recently, at 1-year follow-up, the patient showed healing of fractures with the development of deformities around the elbow. Fig. 5 shows a clinical image of the patient’s elbow with the development of varus deformity over the right elbow due to distal humerus physeal separation, which occurred around the time of birth. However, on the left side, the patient developed cubitus valgus deformity due to distal humerus physeal separation injury at birth, as well as, a fracture of both bones of the left forearm, forcing it into the valgus.
The case was reported to child protection services and other concerned authorities and the patient was managed conservatively. Recently, at 1-year follow-up, the patient showed healing of fractures with the development of deformities around the elbow. Fig. 5 shows a clinical image of the patient’s elbow with the development of varus deformity over the right elbow due to distal humerus physeal separation, which occurred around the time of birth. However, on the left side, the patient developed cubitus valgus deformity due to distal humerus physeal separation injury at birth, as well as, a fracture of both bones of the left forearm, forcing it into the valgus.
Distal humerus physeal separation is a rare injury occurring generally in children <2 years old [1]. The mechanism of injury could be a combination of rotational, angulation, and extension forces. Due to the application of the considerable amount of traction at birth, such injuries have been described in the literature, as secondary to birth trauma [1, 3, 5]. It classically presents a few days later with diffuse swelling around the elbow joint along with the inability to do a full range of motion around the joint. To differentiate between a physeal injury and elbow dislocation, a three-point bony relationship understanding has been described in the literature. However, with the swollen elbow joint and difficulty in palpation of bony landmarks, it is challenging to differentiate the condition clinically. Moreover, the ossification center of the capitellum first appears at around 8 months of age. Hence, it is commonly confused with elbow dislocation on a plain radiograph, and ultrasonography of the elbow joint is necessary to make a definitive diagnosis [2, 6]. The formation of callus and periosteal new bone is variable in fractures of the proximal humeral epiphysis since the joint capsule extends to the anatomical neck of the humerus. Thus, a completely intra-articular epiphyseal plate fracture (Salter-Harris I) will show no callus formation. Typical periosteal callus formation about the proximal humerus 7–10 days after injury indicates more extensive metaphyseal injury [7]. The differential diagnosis for an acutely swollen elbow joint could range from traumatic elbow dislocation, septic arthritis, osteomyelitis, brachial plexus injury, genetic abnormality (e.g., osteogenesis imperfecta), and non-accidental trauma (child abuse). There have been multiple series published in the literature, documenting the association between distal humerus epiphyseal separation and child abuse [8]. In a series of 16 patients, DeLee et al. documented suspicion of child abuse in 6 patients [9]. However, in neonates, birth-related trauma poses an equal likelihood of injury. Supakul et al. reported a series of 16 patients with distal humerus physeal separation, with six of these being caused due to birth-related trauma [1]. Scurvy, vitamin A intoxication, Caffey’s disease, leukemia, and treatment with prostaglandin E all cause subperiosteal new bone formation, both diffusely and focally, and, to that limited extent, can be confused with abuse, but in each case, the related signs, symptoms, and radiographic changes provide easy differentiation from abuse. However, both copper deficiency and Menke’s kinky hair syndrome, itself an abnormality of copper metabolism, can be difficult to differentiate from abuse. Radiographic findings include osteopenia, subperiosteal new bone formation, and metaphyseal spurs with fractures indistinguishable from classic metaphyseal lesions of abuse [10]. In our case, the patient presented on the 8th day, with complaints of bilateral physeal separation injury, along with multiple other fractures. In the setting of no potential hints of child abuse, congenital disorders like osteogenesis imperfecta or birth trauma were considered the most probable diagnosis. However, with a series of consecutive fractures occurring at different sites and signs of rib fractures at multiple stages of healing, child abuse was subsequently confirmed. Although considered, this diagnosis was missed at initial visits due to insufficient evidence as per the child abuse assessment personnel at our hospital. Most fracture patterns in this age group are treated conservatively. The most common complication of distal humerus physeal separation is the development of cubitus varus deformity [3]. The degree of cubitus varus caused has been reported to be mild, ranging up to 5° of varus angle. This substantially benign outcome suggests the role of conservative management in the treatment of such physeal injuries and open reduction, internal fixation seems to be hardly justified. In our case, the patient developed a cubitus varus deformity of the right elbow (Fig. 5), with five degrees varus angle. However, on the left side, the patient developed a valgus deformity, due to the presence of a fracture of both bones of the left forearm.
Ruling out non-accidental trauma as an important cause of bilateral distal humerus physeal separation in young children is crucial. Multiple imaging modalities should be utilized, whereas evaluating a child as injuries around the cartilaginous zones are often missed on radiographs and present with subsequent development of deformity with insidious onset in the future. Further, the child abuse assessment team should be alerted at the very initial presentation and child protection services intimated about the presentation of the child. This could lead to the prevention of limb and life-threatening injuries to the child in the future.
The article summarizes the approach to the diagnosis of battered baby syndrome and the prevention of child abuse. A high suspicion should always be kept when attending to a child with multiple fractures at different stages of healing. Early recognition prevents future mental illnesses such as depression and nightmares.
References
- 1.Supakul N, Hicks RA, Caltoum CB, Karmazyn B. Distal humeral epiphyseal separation in young children: An often-missed fracture-radiographic signs and ultrasound confirmatory diagnosis. AJR Am J Roentgenol 2015;204:W192-8. [Google Scholar]
- 2.Ruo GY. Radiographic diagnosis of fracture-separation of the entire distal humeral epiphysis. Clin Radiol 1987;38:635-7. [Google Scholar]
- 3.Mizuno K, Hirohata K, Kashiwagi D. Fracture-separation of the distal humeral epiphysis in young children. J Bone Joint Surg Am 1979;61:570-3. [Google Scholar]
- 4.Mathew DK, Gangadharan S, Krishnamoorthy V, Shanmughanathan R. Anterior physeal separation of distal humerus: Report of a rare case with review of literature. Indian J Orthop 2021;55:208-12. [Google Scholar]
- 5.Aldossari A, Alsagr G, Alotaibi R, Shogair M, Alharbi H, Alrashedan B. Birth-related distal humerus epiphyseal separation: Outcome following surgical management. J Musculoskeletal Surg Res 2020;4:232-235. [Google Scholar]
- 6.Eckert K, Ackermann O, Schweiger B, Radeloff E, Liedgens P. Ultrasound evaluation of elbow fractures in children. J Med Ultrason (2001) 2013;40:443-51. [Google Scholar]
- 7.Merten DF, Kirks DR, Ruderman RJ. Occult humeral epiphyseal fracture in battered infants. Pediatr Radiol 1981;10:151-4. [Google Scholar]
- 8.Hansen M, Weltzien A, Blum J, Botterill NJ, Rommens PM. Complete distal humeral epiphyseal separation indicating a battered child syndrome: A case report. Arch Orthop Trauma Surg 2008;128:967-72. [Google Scholar]
- 9.DeLee JC, Wilkins KE, Rogers LF, Rockwood CA. Fracture-separation of the distal humeral epiphysis. J Bone Joint Surg Am 1980;62:46-51. [Google Scholar]
- 10.Dwek JR. The radiographic approach to child abuse. Clin Orthop Relat Res 2011;469:776-89. [Google Scholar]











