There needs to be continued awareness that pathologic processes such as extracellular myxoid chondrosarcoma can present in bone. Referrals for benign conditions like fractures can have the potential for becoming complicated work-ups for malignancy and require physicians’ due diligence.
Dr. Thomas Revak, Department of Orthopaedic Surgery, Division of Orthopaedic Trauma, School of Medicine, Saint Louis University, St. Louis, Missouri. E-mail: thomas.revak@health.slu.edu
Introduction: Extraskeletal myxoid chondrosarcoma (EMC) is a rare soft-tissue sarcoma that typically presents in the proximal lower extremity and limb-girdle. It can be easily misdiagnosed, especially when located in atypical locations like the foot.
Case Report: We present the case of an 80-year-old Caucasian female with a left 3rd toe pain and swelling that was initially misdiagnosed as a traumatic fracture on radiographs but later determined to be an indolent EMC based on histology. She was successfully treated with amputation of the toe.
Conclusion: EMC should be considered in the differential of osseous and soft-tissue abnormalities on radiographic imaging of the extremities. As reported in the literature, it can present in atypical locations with minimal symptoms and successful treatments include resection. Future cases presenting similarly should be evaluated for EMC and, if present, reported along with their applied treatment protocols to allow for further assessment of current therapeutic guidelines.
Keywords: Extraskeletal myxoid chondrosarcoma, toe, fracture, trauma.
Extraskeletal myxoid chondrosarcoma (EMC) is a rare indolent sarcoma of the soft tissue [1]. It is twice as likely to be diagnosed in males, typically at 50–60 years of age [2, 3] and is most commonly identified in the proximal lower extremity and limb girdle [4]. Approximately half of patients with this neoplasm develop a metastasis [5], most frequently to the lung, followed by soft tissue and bone, typically between 6 and 15 years post-diagnosis [6]. Diagnoses of these neoplasms can be delayed because of their indolent nature and can have a propensity for misdiagnosis because of their rare and generally asymptomatic presence, especially when found in atypical locations like the foot [7, 8, 9]. We present the following case of a traumatic toe injury that was later diagnosed as an EMC.
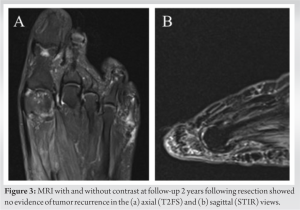
An 80-year-old Caucasian female presented to the clinic with complaints of the left 3rd toe pain and swelling that began after a traumatic impact to the foot while walking. The patient was initially seen in the emergency department and referred for orthopedic evaluation of a questionable non-displaced fracture seen on radiographs. Her medical history included stage T1a endometrial cancer treated with hysterectomy and bilateral salpingo-oophorectomy and invasive ductal breast cancer (estrogen receptor positive) treated with radiation therapy and long-term use of selective estrogen receptor modulators. Notable family medical history includes colon cancer in her mother and prostate cancer in her father. Radiographs demonstrated a fracture through the mid-portion of the third proximal phalanx with a lytic lesion, cortical erosion, and soft-tissue shadowing (Fig. 1).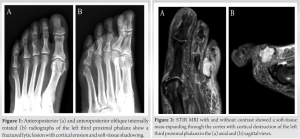
To the best of our knowledge, only 19 cases of EMC in the foot have been previously discussed in the literature [7, 9, 11]. A unique feature of this case was that the EMC was identified incidentally in a patient with a history of the previous malignancies including endometrial cancer and invasive ductal breast carcinoma. The erosive changes and osseous lesions were initially misdiagnosed as a fracture. The indolent nature of EMC that has been demonstrated indicates that it should be considered in the differential diagnosis of incidentally identified masses in the soft tissue of the distal extremities and osseous abnormalities seen on radiographs. This tumor presented with typical histological features of EMC: Elongated malignant cells characterized by ovoid nuclei within eosinophilic cytoplasm and arranged in a cord-like fashion within a myxoid stroma [4]. S-100 positivity is considered non-specific for EMC [9] but was observed. Negative keratin staining and the NR4A3 rearrangement were characteristic of this case and are confirmatory for EMC [12]. The ideal imaging technique for EMC is MRI [12]. Once a diagnosis of EMC is confirmed through biopsy, the curative treatment is a complete resection of the lesion, and potential post-operative radiation [7]. For this case, identification of the lesion using MRI and complete surgical resection without radiation therapy resulted in symptomatic improvement without metastasis. No chemotherapeutic was used and is known to be generally ineffective for EMC [7]. Therefore, the presented case further suggests that the diagnostic and treatment protocol for EMC consisting of MRI, biopsy, and complete surgical resection is effective. Per National Comprehensive Cancer Network recommendations for chondrosarcomas, follow-up should include repeat imaging of the chest and original tumor site, along with complete blood count and physical exam, every 3–6 months for the first 5 years and then annually, ideally up to 10 years following treatment [13].
EMC, a rare soft-tissue mass of the bone, can present in atypical locations and is predisposed to misdiagnosis secondary to its indolent and asymptomatic qualities. Radiographic assessment of osseous and soft-tissue abnormalities, including those in the distal lower extremities, should include EMC in differential diagnosis. Successful treatment of this patient with surgical resection is consistent with previously published cases.
Incidentally identified soft-tissue masses of the bone should be evaluated for EMC. This would allow for improved diagnostic accuracy and prompt initiation of treatment. Future cases and their treatments should continue to be reported to allow for an analysis of their unique clinical presentations and treatment outcomes.
References
- 1.Demicco EG, Wang WL, Madewell JE, Huang D, Bui MM, Bridge JA, et al. Osseous myxochondroid sarcoma: A detailed study of 5 cases of extraskeletal myxoid chondrosarcoma of the bone. Am J Surg Pathol 2013;37:752-62. [Google Scholar]
- 2.Antonescu CR, Argani P, Erlandson RA, Healey JH, Ladanyi M, Huvos AG. Skeletal and extraskeletal myxoid chondrosarcoma: A comparative clinicopathologic, ultrastructural, and molecular study. Cancer 1998;83:1504-21. [Google Scholar]
- 3.Drilon AD, Popat S, Bhuchar G, D’Adamo DR, Keohan ML, Fisher C, et al. Extraskeletal myxoid chondrosarcoma: A retrospective review from 2 referral centers emphasizing long-term outcomes with surgery and chemotherapy. Cancer 2008;113:3364-71. [Google Scholar]
- 4.Lubana SS, Bashir T, Tuli SS, Kemeny MM, Heimann DM. Breast metastasis of extraskeletal myxoid chondrosarcoma: A case report. Am J Case Rep 2015;16:406-14. [Google Scholar]
- 5.Fotiadis C, Charalambopoulos A, Chatzikokolis S, Zografos GC, Genetzakis M, Tringidou R. Extraskeletal myxoid chondrosarcoma metastatic to the pancreas: A case report. World J Gastroenterol 2005;11:2203-5. [Google Scholar]
- 6.Meis-Kindblom JM, Bergh P, Gunterberg B, Kindblom LG. Extraskeletal myxoid chondrosarcoma: A reappraisal of its morphologic spectrum and prognostic factors based on 117 cases. Am J Surg Pathol 1999;23:636-50. [Google Scholar]
- 7.Wilson JT, Pitts C, Hess M, Phillips SG, Siegal GP, Johnson MD. Extraskeletal myxoid chondrosarcoma of the midfoot presenting as charcot arthropathy: A case report. JBJS Case Connect 2019;9:e0458. [Google Scholar]
- 8.Lockyer MG, Rosen DG. Extraskeletal myxoid chondrosarcoma presenting as a plantar fibroma: Case report and review of the literature. Anticancer Res 2015;35:6171-4. [Google Scholar]
- 9.Saraggi D, Salmaso R, Montesco MC, Zamuner C, Tiengo C, Rugge M, et al. Extraskeletal myxoid chondrosarcoma of the foot clinically mimicking plantar fibromatosis. Am J Dermatopathol 2017;39:e38-40. [Google Scholar]
- 10.Benini S, Cocchi S, Gamberi G, Magagnoli G, Vogel D, Ghinelli C, et al. Diagnostic utility of molecular investigation in extraskeletal myxoid chondrosarcoma. J Mol Diagn 2014;16:314-23. [Google Scholar]
- 11.Masrouha K, Multani I, Bhatt O, Ghert M. Extraskeletal myxoid chondrosarcoma: Long-term survival in the setting of metastatic disease. Case Rep Orthop 2020;2020:2684746. [Google Scholar]
- 12.Flucke U, Tops BB, Verdijk MA, van Cleef PJ, van Zwam PH, Slootweg PJ, et al. NR4A3 rearrangement reliably distinguishes between the clinicopathologically overlapping entities myoepithelial carcinoma of soft tissue and cellular extraskeletal myxoid chondrosarcoma. Virchows Arch 2012;460:621-8. [Google Scholar]
- 13.Giuffrida AY, Burgueno JE, Koniaris LG, Gutierrez JC, Duncan R, Scully SP. Chondrosarcoma in the United States (1973 to 2003): An analysis of 2890 cases from the SEER database. J Bone Joint Surg Am 2009;91:1063-72. [Google Scholar]